Cryptogenic organizing pneumonia
advertisement
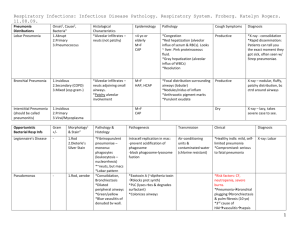
PULMONARY GRAND ROUNDS Eduardo Santiago March 08,2012 HPI • 65 year old woman, no PMH. • Subjective fever, chills, malaise and mild cough 1 month ago. • Progressive shortness of breath. • Dry cough. HPI • Seen by her PCP: Diagnosis of CAP. • Azithromycin for 1 week. • Started on oxygen. • PMH: Unremarkable. • SH: ½ pack per day for 20 years. • Denies any occupational or recreational exposure. • Denies any prior use of medications. • ROS: Unremarkable. PE • HR 70, BP 126/80, RR 14, T 100, O2 SAT 90% on 2 LPM Weight:172.92 • CHEST EXAM: Decreased breath sound at both bases. Diffuse inspiratory crackles at both lower lungs. • CARDIAC EXAM: RRR, S1 and S2 within normal limits. No S3 or S4. • EXTREMITIES: No edema. No clubbing or cyanosis. • SKIN: No skin rash. WBC 9.8 HB 14.4 HT 44 Platelets 366 ESR 44 ANA None detected RF <7 Jo-1 IgG 0 ANCA <1/20 Scl 70 0 • • • • FVC: 1.36L (46%) FEV1: 0.91 (40%) FEV1/FVC: 87% DLCO:5.89 (25%) BAL • • • • Macrophages :46% Lymphocytes:7% Neutrophils:43% Bronchial lining cells:4% Pathology • Patchy organizing pneumonia, fibroblastic intra alveolar infiltrate, scattered lymphocytes within the interstitium. • No significant acute inflammation. • No granulation tissue. • No evidence of vasculitis. Date FEV1 FVC FEV1/FVC DLCO Aug 11 0.91 (40%) 1.36L (46%) 87% 5.89 (25%) Nov 11 1.35(60%) 1.64 (56%) 82% 9.46(40%) COP COP • J.M Charcot 1877–1878. • Milne: Type of pneumonia where the usual process of resolution has failed and organization of the inflammatory exudate in the air alveoli of the lung by fibrous tissue has resulted. COP • Organizing pneumonia: Endobronchial connective tissue masses composed of myxoid fibroblastic tissue resembling granulation tissue. • Central cluster of mononuclear inflammatory cells. • Chronic inflammation in the walls of the surrounding alveoli. • Preserve lung architecture. COP • Organizing pneumonia pathologic pattern is a nonspecific reaction that results from alveolar damage with intra-alveolar leakage of plasma protein with alveolar organization. COP • Clinical, radiological and pathological diagnosis. • Pattern of organizing pneumonia must be prominent. Pathogenesis • The intra alveolar fibrosis is its usual dramatic reversibility with corticosteroids and not associated with progressive irreversible fibrosis . Pathogenesis/ First Stage • Alveolar epithelial injury with necrosis and sloughing of pneumocytes resulting in the denudation of the epithelial basal lamina. • The endothelial cells are only mildly damaged. • Infiltration of the alveolar interstitium by inflammatory cells: lymphocytes, neutrophils and eosinophils. Pathogenesis/ Second Satge • Intra alveolar stage: formation of fibrinoid inflammatory cell clusters with prominent bands of fibrin and inflammatory cells. • Formation of fibro inflammatory buds, fibrin is fragmented and reduction of inflammatory cells. • Migration of fibroblast from the interstitium and proliferation. Pathogenesis/Second Stage • Myofibroblast. • Proliferation of the alveolar cells and re epithelialization of the basal lamina. Pathogenesis/Third stage • Inflammatory cells have disappeared. • There is no fibrin within the alveolar lumen. • Concentric rings of fibroblasts alternate with layers of connective tissue. Connective Matrix • Loose connective matrix with high type III collagen content which is more susceptible to degradation and reversal of fibrosis. Angiogenesis • Prominent capillarization of the intra alveolar buds. • Vascular endothelial growth factor and basic fibroblast growth factor. • Angiogenesis could contribute to the reversal of buds in OP. Pathogenesis • The opposing mechanisms of reversibility of fibrosis in COP and ongoing fibrosis in UIP are not yet established. Radiology Radiology • Multiple alveolar opacities: typical COP. • Solitary opacity: focal COP. • Infiltrative opacities: infiltrative COP. Diagnosis • Diagnosis of organizing pneumonia. • Exclusion of any possible cause. • Histopathology: Buds of granulation tissue consisting of fibroblasts myofibroblasts embedded in connective tissue. Diagnosis • Definite: compatible clinicoradiologic manifestations and typical pathologic pattern on a pulmonary biopsy of sufficient size. • Probable: findings of organizing pneumonia on transbronchial biopsy and a typical clinicoradiologic presentation without pathologic confirmation. • Possible: typical clinicoradiologic presentation without biopsy confirmation. Treatment • Rapid clinical improvement and clearing of the opacities. • The precise dose and duration of treatment have not been established. • Prednisone 0.75–1.5 mg/kg/day. • 0.75 mg/kg/day during 4 weeks, followed by 0.5 mg/kg for 4 weeks, then 20 mg for 4 weeks, 10 mg for 6 weeks, and then 5mg for 6 weeks. Treatment • Complete clinical and physiologic recovery in 65 % of patients. Gary Epler. Bronchiolitis Obliterans Organizing Pneumonia. NEJM; 1985:152-8 Treatment • Predictors of relapse: delayed treatment and mildly increased gammaglutamyltransferase and alkaline phosphatase levels. Treatment • Severe cases: prednisolone 2mg/kg/day for the first 3-5 days. Treatment • Spontaneous improvement. • Macrolides: • Patients with minimal symptoms and/or minimal physiologic impairment. • Adjuvant therapy in patients receiving steroids. • Patients who cannot tolerate steroids. • 3 to 6 months or longer. Diane E. Stover.Macrolides: A Treatment Alternative for Bronchiolitis Obliterans Organizing Pneumonia?. CHEST 2005; 128:3611–3617 Reference • American Thoracic Society/European Respiratory Society. Classification of the idiopathic interstitial pneumonias: international multidisciplinary consensus. American Thoracic Society/European Respiratory Society. Am J Respir Crit Care Med 2002;165: 277–304. • J.-F. Cordier. Cryptogenic organizing pneumonia. Clinics in Chest Medicine 2004;25 : 727– 738. • J.-F. Cordier. Organising pneumonia. Thorax 2000;55:318–328. • J.-F. Cordier. Cryptogenic organizing pneumonia. Eur Respir J 2006; 28: 422–446.