Document
advertisement

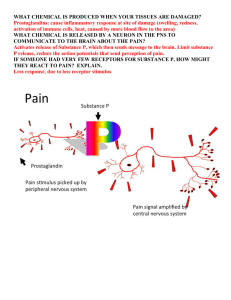
Anti-Inflammatory & Immunosuppressive Drugs 1 I-3 Fall 2012 Marieke Kruidering, Ph.D. Pharmacology in I-3 Week 2 Week 4 Week 5 Anti-inflammatory and immunosuppressive drugs 1 & 2 TBL Antibacterial drugs 1 Antibacterial drugs 2 Antibacterial drugs 3 Drugs for mycobacterial infections Week 6 Week 7 Week 8 Antifungal drugs Antiviral drugs 1 & 2 Antiviral drugs 3 Week 9 Antiparasitic drugs Reminder - Studying Pharmacology • Drug names (focus on prototypes; use flash cards, tables) • Unusual chemical structures (eg, antibody, receptor, cytokine) • Mechanisms of action • Clinical uses (aka “spectrum of activity”) • Pharmacokinetics (eg, notable route administration, elimination) • Adverse effects (predictable, unusual, teratogens) • Drug interactions (eg, CYP450 inducers, inhibitors, narrow therapeutic window AND a CYP substrate) Anti-inflammatory & Immunosuppressant Drugs 1 2 NSAIDS Acetaminophen Immunosuppressants Newer biologic agents Drugs for gout (TBL) (tylenol) Antihistamines Corticosteroids Inflammatory cascade: Triggers Infection Immune response Tissue and/or vessel damage Inflammatory Mediators Acute Inflammatory Response Note this is a common & non-specific response - Redness - Heat - Swelling - Pain (allodynia) - Loss of function Drugs block production or effect of inflammatory mediators Tissue and/or vessel damage Infection Inflammatory Mediators o o o o o Vasoactive peptides: Histamine,serotonin The kinin system Coagulation cascade The complement system Arachidonic Acid metabolites Anti-histamines NSAIDS Corticosteroids Inflammatory Enzymes: PLA2 & COX 3. Zileuton Montelukast, zafirlukast 1. Steroids Phospholipase A 2 2.NSAIDS (including aspirin) Arachidonic acid (AA) Lipoxygenase Lipoxygenase products (leukotrienes) Inflammatory effects (esp. in asthma) Cyclooxygenase (COX) Prostaglandins & thromboxanes Inflammatory effects Homeostatic (inducible) Functions (stomach mucus) Eicosanoids: PGs & TXA Effects AA Cyclooxygenase (COX) Lipoxygenase NSAIDS PGH2,PGG2 unstable) Leukotrienes) • Chemotaxis • Vasodilation Thromboxane A2 Stable prostaglandins PGD2,PGE2,PGF2 Prostacyclin PGI2 1. 1. Vasoconstriction 2. Stimulate platelet aggregation Vasodilation 1. Vasodilation 2. Inhibition of platelet aggregation Notable NSAIDS Aspirin ibuprofen (Motrin, Advil) naproxen (Naprosyn, Aleve) etodolac (Lodine) cox 2 >cox1 indomethacin (Indocin) ketorolac (Toradol) - parenteral (IM) celecoxib (Celebrex) NSAID Dose Dependent Therapeutic Effects Antipyretic, Analgesic Antithrombotic (aspirin only) 0 1 2 Anti-inflammatory 3 4 5 Daily dose of aspirin (g) N-acetyl--aminophenol Acetaminophen (Tylenol; AKA paracetamol) antipyretic, analgesic NOT anti-inflammatory NSAID & Acetaminophen Toxicity NSAIDS: Disruption of homeostatic function GI upset & ulcers (esp. COX-1) Acute renal failure (COX-1 & 2) Thrombosis (COX-2) Bleeding (COX-1, esp. aspirin) Aspirin: Reye syndrome Syndrome of hepatic injury & encephalopathy in kids treated with aspirin after a viral illness Impaired labor (COX-1 & 2) Aspirin & acetaminophen: Dangerous in overdose (OTC: Can be fatal) Aspirin: salicylate poisoning (respiratory alkalosis followed by metabolic acidosis) Acetaminophen: liver failure NSAIDS: Rare hypersensitivity reaction Excessive shunting of arachidonic acid products to lipoxygenase pathway when COX is blocked Acetaminophen Toxicity Acetaminophen UDP glucuronosyltransferase Sulfotransferase glucuronide sulfate CYP2E1 induces Acetylcysteine (antidote) Glutathione-Stransferase glutathione Live r failure protein The Inflammatory Cascade Perceived threat Adaptive immune system Tissue injury Leukocyte & endothelial cell activation NSAIDS, acetaminophen Antihistamines Inflammatory mediators Inflammation (redness, edema, warmth, pain, tissue destruction) Infection Innate immune system IgE-Mediated Mast Cell Degranulation Resting Mast Cell Activated Mast Cell Histamine Proteases Heparin Histamine Histidine Histidine decarboxylase Histamine H receptor 1 -vascular permeability venule vasodilation pruritus Cimetidine, ranitidine H2 receptor - gastric acid secretion H1 Histamine Antagonists (Antihistamines) Prototype Properties Clinical Uses Loratadine (Claritin) Fexofenadine (Allegra) Low affinity for muscarinic receptors, doesn’t cross BBB Allergic reactions Diphenhydramine (Benadryl) Muscarinic antagonist, crosses BBB Allergic reactions, dystonic rxtn to dopamine blockers, OTC sleep aid, antiemetic However, in the case of severe hypersensitivity reactions, including anaphylaxis, drugs of choice are: Epinephrine (need 1 vasoconstriction and 2 bronchodilation) and corticosteroids! The Mighty Corticosteroids Perceived threat Infection Corticosteroids Adaptive immune system Tissue injury Innate immune system Corticosteroids Leukocyte & endothelial cell activation Corticosteroids Corticosteroids Inflammatory mediators Inflammation (redness, edema, warmth, pain, tissue destruction) Glucocorticoids Regulate Transcription Cortisol Cortisol Cortisol GR NUCLEUS ­ transcription (eg, lipocortin) IP HS P GR HSP Cortisol Cortisol GR GR or ¯transcription (IL-1, IL-2, TNF- a, IF-g) GRE mRN A Proteins mRN A GR, glucocorticoid receptor; HSP, heat shock protein; IP, immunophilin;GRE, glucocorticoid receptor Corticosteroids Inhibit Eicosanoid Production Corticosteroids Lipocortin Phospholipase A2 Corticosteroids inhibit induction of COX-2 expression Arachidonic acid Lipoxygenase Lipoxygenase products (leukotrienes) Cyclooxygenase (COX) Prostaglandins & thromboxanes Glucocorticoids Are Powerful Immunosuppressants Corticosteroids affect nearly every facet of immune function, although less inhibition of humoral arm than cell-mediated arm; they also induce apoptosis in rapidly-dividing leukocytes Clinical Use of Glucocorticoids Self-limited reaction (eg, poison oak) Acute flare of a chronic inflammatory condition or organ rejection reaction Toxicity of Chronic Systemic Glucocorticoids Cushing’s syndrome • Fat redistribution • Hypertension • Glucose intolerance • Impaired wound healing • Osteoporosis (prevent with bisphosphonates) • Cataracts • Gastric ulcers (prevent with omeprazole, misoprostol) • Risk of infection • CNS effects, including psychosis • Growth inhibition in children www.sd-neurosurgeon.com/diseases/pit_tumors.html Adrenal Suppression with Chronic Systemic Glucocorticoids Hypothalamus CRH prednisone Anterior pituitary ACTH cortisol, aldosterone Adrenal cortex Some Corticosteroids Relative AntiInflammatory Activity Relative SaltRetaining Activity Oral, parenteral, topical 1 1 Cortisone Oral 0.8 0.8 Prednisone Oral 4 0.3 Triamcinolone Oral, injectable, topical, inhaled 5 0 Dexamethasone Oral, injectable, topical 30 0 Oral 0 250 Agent Cortisol (hydrocortisone) Fludrocortisone (mineralocorticoid) Forms Available Summary Inhibitors of the production or action of inflammatory mediators (NSAIDS, antihistamines, presumably acetaminophen) provide symptomatic relief with reasonable safety in most people but do not ameliorate ongoing immune reaction; Even though aspirin and acetaminophen are OTC overdoses can be fatal. Corticosteroids have powerful anti-inflammatory and immunosuppressant actions but chronic use produces much toxicity FYI: Eicosanoids As Drugs (Additional info that will NOT be tested in I-3) Tip: recognize the “prost” in the drug name so you know it is a prostaglandin analog Drug Name Analog Of Clinical Use Epoprostenol PGI2 Pulmonary hypertension Dinoprostone PGE2 Medical abortion, relax uterine cervix in preparation for induction of labor Misoprostol PGE1 Peptic ulcer, medical abortion Alprostadil PGE1 Maintain a patent (open) ductus arteriosus in neonates with certain cardiac malformations until emergency surgery; erectile dysfunction Carboprost PGF2 Labor induction Latanoprost PGF2 Glaucoma FYI. ASPIRIN: Antiplatelet effect Adverse effects: bleeding due to longer cox -1 inhibition in platelets than in endothelium (why?) Platelets have no nucleus thus cannot resynthesize COX-1 once it is inhibited by aspirin, while endothelial cells can regenerate COX-2. Net result: selective COX 1 inhibition & reduced platelet aggregation.