Seventh International Symposium in Continuing
Nursing Education/March, 2014
3/2014
Donald W. McLaren, MD
Objectives
To discuss how to evaluate and
determine cause of anemia
To discuss Iron deficiency (ID) and Iron
Deficiency Anemia (IDA) - causes,
evaluation, signs, symptoms, treatment
and prevention at different ages
To discuss briefly few other common
causes of anemia
Burden of anemia globally
24% of world population; 1.62 billion
anemic
Greatest burden pregnant women
and children < 5
Highest prevalence Africa and SE Asia
In these locations > 65% of children < 5
years are anemic
http://www.k4health.org/toolkits/anemia-prevention/anemia-causes-prevalence-impact
Definitions
Anemia – reduced # circulating RBCs or
decreased circulating hemoglobin as
measured by decreased Hgb, Hct or RBC
count
Hgb – concentration of hemoglobin (gm/dl)
Hct – % of sample of whole blood (WB)
occupied by intact RBCs.
RBC count: # RBCs in specified volume of
blood – usually millions of RBC / μL of
whole blood (WB)
Indices
MCV (mean corpuscular volume) – volume of
average RBC measured or calculated as MCV
(femtoliters; 10-15) = 10 X Hct ÷ RBC; indication of
cell size
MCH (Mean Corpuscular Hemoglobin) - mass of
Hgb in a RBC
MCHC (mean corpuscular hemoglobin
concentration) – measure of concentration of
hemoglobin in a given volume of packed RBCs
Microcytosis: ↓MCV; RBC size small
Macrocytosis: ↑MCV; RBC size large
Normocytosis : MCV WNL; RBC size
normal
Hypochromic: paler than normal –
↓Hgb as measured by ↓MCH, MCHC
Hyperchromic: ↑Hgb – ↑MCH, MCHC
RDW (RBC distribution width) – measure
of variability of size of RBCs - normal about
11.5-14.5 – increased in nutritional
deficiencies (like Fe, B12)
Anisocytosis – when there is a lot of
variation of sizes of RBC as seen on
microscope - ↑RDW
Peripheral smear – blood smear stained
to be looked at to see cell size, shape,
abnormal cells, etc.
Reticulocyte – immature RBC usually
released into blood 1 day prior to
becoming mature RBC
Reticulocyte count – number of
reticulocytes in peripheral blood
expressed as % of total RBCs
What is included in a CBC
Hgb, Hct
RBC count
Indices – MCV, MCH, MCHC
RDW
WBC and differential or diff indicating
how many of each type of WBC is there
Platelet count
Normal values vary with age and sex
http://upload.wikimedia.org/wikipedia/en/4/49/CBC_With_Differential.jpg
http://www.childrensmn.org/manuals/lab/hematology/018981.asp
RBC and appearance in
peripheral smear
http://en.wikipedia.org/wiki/Reticulocyte_index
Reticulocyte unstained and
stained
http://en.wikipedia.org/wiki/Reticulocyte_index
http://www.med-ed.virginia.edu/courses/path/innes/nh/morphology.cfm
Define anemia
Hgb, Hct (H/H) > 2 SD below the mean
H/H < 12g/dl or 36% for adult women
H/H < 13.5(14.0) and 41(42)% for men
Higher if live at altitude, smokers, athletes
Consider volume shifts: bleed, pregnancy
African-Americans Hgb 0.5-1.0 g/dl < white
Can drop 15%, be significant drop, still WNL
Other basics of erythropoiesis
(making of red cells)
EPO (erythropoietin) from kidney ↑ if
anemia.
If marrow functioning, raw materials
present (iron, B12) EPO stimulates marrow
to produce more RBCs – leads to
increased reticulocytes.
Reticulocytes released from bone marrow
and circulate normally 1 day before
becoming mature RBC
Normal RBCs circulate for about 110-120
days before being removed from circulation
Some more basics
Ordinarily rate of production = rate of
removal
Retics replace about 1% of cells daily so
normal retic count around 1% (0.5-1.5%)
If increased RBC destruction (i.e. SCD)
must replace more. If cell lifespan 20
days must replace 5% / day
Will now discuss W/U of anemia
Causes of Anemia – only 3
Decreased RBC production – bone
marrow not keeping up with normal RBC
loses (hypoproliferative)
Increased RBC destruction or
decreased survival time (hemolysis)
Blood loss (hemorrhage)
Combinations not uncommon
Essential Lab for Evaluation of
Anemia
CBC
Peripheral smear read by someone
who knows what they are looking for
Reticulocyte count
Can classify anemia based on these 3
Other testing depending on results
2 General Approaches to
Evaluate Anemia
Kinetic (physiological) approach
addresses the mechanism or cause of
the anemia. Retic count used to divide
into hemolysis or blood loss (↓retic) vs.
hypoproliferative (↓retic count)
Morphologic approach – categorizing
based on RBC size as determined by
MCV and peripheral smear
Will discuss a combination of two
Kinetic approach
Low retic = decreased RBC production
Lack of nutrients (Fe, B12, folate)
Bone marrow disorders or suppression
Low EPO level
High retic = increased destruction of
RBC or blood loss
Morphological Approach to
Anemia
Determine RBCs size: small, normal or
large based on MCV, peripheral smear
For adults MCV range about 80-96
DDx if microcytic anemia fairly short
Retic count helpful to further sort out
normocytic and macrocytic anemias.
Sometimes not straightforward – classic
Fe deficiency microcytic, but if mild and
early is normocytic
Always begin with Hx and Px
Are they stable? Are there S/S of anemia?
Known or obvious bleeding?
Is anemia acute, chronic or subacute
Any chronic illness?
Ethnicity
Alcohol, medications, history transfusions
Good dietary history
Big spleen, liver disease, jaundice, tender
bone, H-S megaly, lymphadenopathy
Look at rest of CBC/peripheral
smear – not just RBCs
Abnormal cells may indicate SCD,
spherocytosis, leukemia, and on
occasion make the diagnosis for you
Pancytopenia changes the differential
diagnosis – likely need hematologist
Destruction in peripheral blood
Aplastic anemia, hematologic malignancy,
B12 deficiency, anorexia, radiation,
chemotherapy, myeloproliferative disease
Microcytic anemia
Relatively few causes
*Fe deficiency anemia (IDA) (early can be
normocytic)
○ ↓RBC, ↓Indices, ↑ RDW
*Thalassemias (↓ globin synthesis)
*Lead toxicity (↓ heme synthesis)
*Anemia of chronic disease (or normocytic)
Sideroblastic anemias
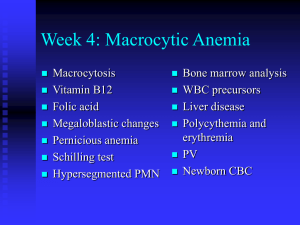
Macrocytic (↑MCV) DDx
*Folate, B12 deficiency (Usual cause of
MCV > 115)
Extreme reticulocytosis
Alcoholism, liver disease, hypothyroidism
*HIV antiviral therapy
*Most chemotherapeutic agents
Myelodysplastic disorders
Adults > 65 may have higher MCV than
younger – use 100 rather than 96 for ULN
Can narrow diagnosis based on
peripheral smear and retic count
*Megaloblastic (macro-ovalocytes and
hypersegmented neutrophils) or Low retic
B12 or folate deficiency
HIV meds, Anticonvulsants (folate depletion)
(dilantin, valproate), Cancer drugs (+ anemia)
Nonmegaloblastic with round macrocytes
and macroreticulocytes –
(low retic) Alcohol, thyroid, liver disease
(high retic) some hemolytic
Myeloproliferative disorders - bone marrow
Normocytic Anemia DDx with
reticulocytosis
Huge category – Narrow ddx with retic count
*Blood loss, hypersplenism
*Increased destruction, loss of RBCs
(hemolysis)
Congenital or intrinsic (Hemoglobinopathy: SS,
SC; RBC membrane disorders: spherocytosis;
RBC enzyme deficiency (G-6-PD, pyruvate kinase)
Acquired (extrinsic): Mechanical, macrovascular,
Micro- angiopathic (DIC, HUS, TTP) autoimmune
hemolytic anemias, drug related (Aldomet,
penicillins, cephalosporins)] PNH
Mixture of micro/macrocytic anemias
Normocytic Anemia With Low
Retic
Decreased production normal sized cells
(*anemia of chronic illness, aplastic
anemia, bone marrow infiltration)
*Uncompensated increase in plasma
volume (pregnancy)
Low EPO states (CRF, liver or kidney
disease, Endocrine deficiency)
Myeloproliferative disorders, dysplasia,
fibrosis, marrow replacement
Bone marrow can get dx 90-92% of time
Summary (read RPI as retic for
now)
Microcytic
Normocytic
↑ RPI
or ARC
↓ RPI
or ARC
Macrocytic
↑ RPI
or ARC
↓ RPI
Or ARC
Then it is easy to look up differential for each combination of MCV and
Retic. *RPI = Reticulocyte production index; ARC = Absolute retic count
Many sites for DDx once anemia
classified MCV and RPI
Just Google causes of ____ anemia.
Microcytic anemia or microcytosis
http://www.aafp.org/afp/2010/1101/p1117.html
Normocytic anemia or normocytosis
http://www.aafp.org/afp/2000/1115/p2255.html
Macrocytic anemia or macrocytosis
http://www.aafp.org/afp/2009/0201/p203.html
Use of retic count
Normal 0.5-1.5% in adult
Normally keeps up with RBC loss so that
Hgb/Hct stable
Can increase significantly to replace lost
RBCs in hemolysis, blood loss if a) marrow
working, b) sufficient EPO, c) nutrients
How do we know in the face of anemia if
elevated retic count is appropriately high
vs. insufficient for degree of anemia. If Hct
is 25, what should retic be? 3? 7? 15?
Most common anemias in U.S.
Copyright © 2000-2013 The Cleveland Clinic Foundation.
http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/hematology-oncology/anemia/
Corrected retic count or RPI
(reticulocyte production index)
Can use either absolute retic count (RBC X
% retics) or RPI to clarify situation
Reticulocyte count is a %. So, if you
decrease RBCs (anemia) with the same
number of retics gives falsely elevated %
How many retics being released from bone
marrow vs. normal - measure of how many
RBCs being made in the bone marrow
1st of 2 corrections is for low RBC count –
to give a “corrected retic count” or “retic
index” = Retic count X Hct/45 (normal Hct)
10% retics
Retic Count X Hct/normal Hct =
20% X 5/10 = 10%
Reticulocyte production index
(RPI)
Second correction needed in anemia, retics
are released early in a less mature state
Retics normally stay in the blood for 1 day
If released early stay in circulation longer
before reaching maturity
Divide previously corrected retic count by
maturation factor corrects for early release
Hct 36-45: 1.0;
Hct < 15: 2.5
Hct 26-35: 1.5
Hct 16-25: 2.0
http://faculty.washington.edu/rrichard/anemia.ppt
RPI
RPI = retic count X Hct/45
Maturation correction
1-2% is normal in non-anemic individual
In anemia, RPI< 2 means there is an
inadequate response to correct anemia
and indicates hypoproliferative anemia
In anemia, RPI> 3 appropriate/adequate
compensatory response to anemia and
represents destruction or decreased
survival or loss of red cells
http://allaboutblood.com/tag/corrected-reticulocyte-index/
Iron (Fe) Deficiency anemia (IDA)
in Infants and Young Children
IDA most common cause anemia in world
1-3 years old: 9% in U.S. have ID, 3% IDA
Risk factors: poverty, Black or Hispanic
race, obesity, prematurity, immigrants
Fe balance
75% bound in heme proteins Hgb & myoglobin
Most rest is storage iron in ferritin, Hemosiderin
Tiny amount bound to transferrin for transport
3% in critical enzyme systems
Adults: 5% of daily Fe needs to come
from dietary sources: absorption = loss
Children: 30% of daily needs come must
from diet due to growth spurt and body
muscle mass increases
Fe Absorption
Very little normally leaves, enters body
daily – little lost in feces, urine. Most
recycled by macrophages
Mechanisms affecting intestinal
absorption, transport a) body Fe stores,
b) rate of erythropoiesis, c)
Bioavailability of dietary Fe, d) hepcidin
Absorption increases with ↑
erythropoiesis.
Intestinal Fe absorption and need
for iron
Bioavailability: Heme sources (meat,
poultry, fish) (30%) > than non-heme
sources (vegetable) (10%)
Hepcidin: made by liver – inhibits GI Fe
absorption and storage Fe release
Healthy term infants have enough Fe
stores for 5-6 months if mother has
enough Fe. Premies much less.
Some Fe sources and infant
needs
Breast milk: low Fe; 50% bioavailability
Formulas: 12-36X more Fe; 4-6%
bioavailability.
Full term breastfed babies need 1 mg/kg
up to 15 mg beginning at age 4 months
Breastfed premies: Need 2-4 mg/kg up
to 15 mg starting at age 1 month of age
Age 1-3: 7; 4-8: 10; 9-13: 8 mg/day
Causes of IDA
Insufficient Fe intake
Poor Fe absorption (poor dietary sources
or other reasons)
Introduction of unmodified cow’s milk at <
age 12 months
FOB loss 2o to cow’s milk proteininduced colitis (6 moa: 30% : 5% FOB +
if on Cow’s milk vs. formula in infants)
Breast milk too long – without
supplementation
Causes of IDA Continued
Giving > 600 ml/day or > 6 breast feeds /
day at 8-12 months of age.
Preschool - > 720 cc milk daily (low
concentration and bioavailability of Fe +
possible ↑ intestinal blood loss increased
Absorbed most from duodenum so
decreased absorption with Celiac,
Crohn’s, giardia, resection proximal SB, H.
pylori.
Blood loss - IBD, cow’s milk proteininduced colitis
Prevention
Exclusive breast feeding till age 4-6 mo.
Supplement with Fe at 4 months
With iron fortified cereal after 6 mo
Only Fe fortified formulas (avoid cow’s
milk) if not breastfed till age 1 year
After 6 mo > one feeding of foods rich in
Vitamin C daily (increase Fe absorption)
After 6 months consider pureed meats
Age 1-5 limit to 24 oz cows milk/day
Development of IDA
Use up storage iron first
Iron limited erythropoiesis
IDA (last stage and first to recover)
Initially normocytic / normochromic
Eventually classic microcytic
hypochromic hypoproductive anemia
Signs/symptoms
Most asymptomatic as develops slowly
Lethargy, irritability, tachypnea, poor feeding
Pallor (not reliable sign till severe), ↑HR
↓ exercise capacity (even pre-anemic)
Pica (appetite for substances not fit for food paper, clay, dirt), pagophagia (pica for ice is
common and specific for ID) – often precede
anemia and resolve early upon treatment
Beeturia (red urine with beets)
Fe deficiency can cause RLS - 9X ↑incidence
Complications of IDA and
treatment
Neurodevelopmental issues
Psychomotor, mental development impairment,
cognitive issues even in adolescents
Fe supplementation can prevent but may not
correct once established.
Improvement of attention, concentration and
cognitive function with Fe supplementation
Auditory and visual dysfunction
Decreased work capacity in adults
Immunity – Fe may increase bacterial,
malaria infection risk. Transferrin has
bacteriostatic effects lost if saturated by Fe
Screening
2/3 with ID don’t have IDA (age 1-3 9% ID,
2-3% IDA)
2/3 those anemic have another diagnosis
Anemia risk assessment at ages 4, 15 18,
24, 30 mo then yearly. All premies at risk.
Use focused dietary history
Standards already listed
< 2 servings of Fe rich foods daily after 6
months or < 3 servings age 1-5 years
Intake of sweets, lots of fatty snacks, soft drinks
Diagnosis/Lab
Universal lab screening of all 9-12 mo.
Hgb, Hct or CBC
If at risk re-screen at 15-18 months
If high risk of Fe deficiency also check
ferritin as one can be ID without IDA
Fe deficiency anemia typically has low
MCV, MCH, MCHC and high RDW
If IDA suspected
Can treat in this age empirically and test
to confirm only if not responding well
If need to prove or if severe check
Ferritin best single test – measure of Fe
stores. (Acute phase reactant so if another
illness can be falsely elevated - ↓ in IDA)
Fe ↓ in IDA
TIBC (total iron binding capacity) ↑in IDA
Fe/TIBC= Fe, transferrin saturation ↓ in IDA
Treatment
If anemic dietary history, correct diet
Lead exposure questionnaire or level
If age > 2 some recommend stool for
FOB X 3, retic count, peripheral smear
If in doubt or severe (< 7 Hgb) check Fe,
TIBC, ferritin (< 12), transferrin sat along
with FOB X 3.
Treatment continued
Most cost effective means to tx if consistent
diet history and no indication of Pb toxicity
is a presumptive trial of iron ($5.00)
3 -6 mg/kg elemental Fe/day up to 150 mg
FeSO4 daily or BID (FeSO4 20% elemental
Fe)
Continue Fe several (3-4) months after
anemia resolved to replace stores
Maximize absorption - give between meals,
with juice
Iron therapy
Repeat CBC 1 month (sooner if severe) for > 1
gm/dl increase in Hgb – if not re-evaluate
Can use other forms of Fe – i.e. Fe Gluconate
Avoid enteric coated if possible
Rarely causes GI upset at this age (10%)
MUST at same time institute dietary changes
Repeat periodically till normal for age
Once normal continue Fe 3-4 months to
replace Fe stores
Nonresponders
Check adherence including diet
Intercurrent illness that can lower Hgb?
Check Ferritin, Hgb electrophoresis, Vit
B12, RBC folate, Fe, TIBC, ferritin
Fe/TIBC = transferrin saturation
Several stool specimens for occult blood
Non-responders continued
Eliminate all cow’s milk protein from diet
R/O Celiac disease
ESR and albumin – to screen for IBD
Consider rare causes, incorrect dx
(Thalassemia, Chronic disease)
Rare to need parenteral Fe
Rare to need transfusion even if Hgb 4-5
g/dl unless in distress
Adolescents
↑ risk due to expansion of blood volume,
increased muscle mass with growth
Eating patterns (vegetarian, anorexia)
Incidence rises with age in females
ID 11% IDA 3% 16-19 in girl vs. < 1% boys
Obesity, training athletes, periods ↑ risk
Screen ALL at risk, girls q 5 yr beginning at
13, boys once during growth spurt
Adolescents
Cutoff Hgb < 11 and cutoff ferritin < 12
For tx least expensive is Fe sulfate 325 Fe
Sulfate = 65 mg elemental Fe.
Ca inhibits, ascorbic acid ↑ absorption
If not tolerating iron consider
Taking with food + ascorbic acid
Feosol 45 mg elemental Fe/5cc better tolerated
More likely not to tolerate, need transfusion
(< 7 Hgb + distress, end organ issues)
Adults
Main difference in adult – Must look for
cause: cause blood loss till proven
otherwise. Overt sources of blood loss
Severe traumatic hemorrhage
Hematemesis, melana, or hematochezia
Hemoptysis
Severe menorrhagia, pregnancies, lactation
Gross hematuria
Frequent blood donating
Marathon running
Occult blood loss – not obvious
Usually GI tract in men and postmenopausal women
Heavy periods in pre-menopausal
women
While reduced Fe absorption and
deficient diet may be cause, must do GI
work-up to avoid missing malignancy
Overall risk of malignancy not high
(12%), but much higher than without IDA
Evaluation of occult blood loss
First study to do based on history –
Colonoscopy vs. EGD
In one study of 100 persons, source
found in 62%: 25 with colonoscopy, 36
with EGD, 1 with both; 11 had cancer
For most do colonoscopy first because
almost all need even if EGD finds lesion
If cause not found EGD
Evaluation of occult blood loss
If no cause found consider SB capsule
endoscopy
R/O Celiac disease, H. Pylori, atrophic
gastritis esp. if refractory to Fe therapy
(100% Celiac, 70% H. Pylori refractory)
Hookworms cause increase losses
Can consume 0.3-0.5 ml blood/day
Often cause eosinophilia
Consider Foods/meds that interfere with Fe
absorption
Other causes
Gastric bypass
Pulmonary hemosiderosis
Intravascular hemolysis leading to urinary
loss of Fe
Congenital Fe deficiency not responsive to
Fe or defects in Fe absorption or utilization
Transient erythroblastopenia of
childhood
Temporary (always) RBC aplasia
occurring at ages 6 mo – 4 yrs
Fairly common but don’t know true
incidence as many cases not detected
Normocytic anemia
Cause not known. Viral? Toxic?
Mild neutropenia possible; normal or
slightly high platelets
TEC
Hgb 6-8 with reticulocytopenia
Normal MCV except during recovery
due to retics (distinguishes from
congenital pure red cell aplasia –
macrocytic anemia)
Lasts 1-2 months then recovery
80% recover within 1 month
Transfusion rarely necessary
Thalassemia
Major forms deadly or very sick
Minor and trait look a bit like IDA
Beta thal minor – has elevated Hgb A2,
F on Hgb electrophoresis, target cells,
low MCV and – W/U for IDA
Alpha more complex
If failed Fe tx important to diagnose to
prevent eventual iron overload from
increases absorption and repeated tx.
B12 (and folate) deficiency
Macrocytic anemia with low retic
Check B12, folate in all with high MCV
B12 variable so if low need repeat
Folate: leafy green veges, fruit, enriched
sources
B12 animal products: eggs, meat, fish,
milk
(homocysteine, MMA) Both high in B12
and only HC in folate deficiency.
Can effect all 3 hematopoietic cell lines
B12 low from poor intake, gastrectomy,
bariatric surgery, H. Pylori, breastfed,
fish tapeworm, drugs (PPI), hereditary
causes, pernicious anemia, Celiac
Folate – Poor intake, drugs (MTX),
increased needs, Celiac
Folate needed in purine synthesis; B12
needed as cofactor in activation of folate
Neurological damage from B12
deficiency which can be permanent
S/S/lab in B12 deficiency
B12 – anemia but not always
Macrocytosis and oval cells
Neuro symptoms
Hypersegmented WBC (> 5 nuclei)
B12 signs/symptoms: Glossitis, +
anemia, memory loss, irritability, ataxia,
dementia, peripheral neuropathy
Danger that neurological symptoms of
B12 can be permanent once established
Cobalamin levels — ”Commercial labs use different
methods for measuring Cbl. …there are different
normal ranges and no "gold standard“ Accordingly,
therapeutic trials of Cbl are warranted when testing
results are in conflict with the clinical diagnosis.”
Interpretation of B12 (Cbl) levels :
“●>300 pg/mL (>221 pmol/L) — normal result; Cbl
deficiency unlikely (ie, probability of 1 to 5 percent)
●200 to 300 pg/mL (148 to 221 pmol/L) — borderline
result; Cbl deficiency possible
●<200 pg/mL (<148 pmol/L) — low; consistent with
Cbl deficiency (specificity of 95 to 100 percent)”
Schrier SL. “Diagnosis and treatment of vitamin B12 and folate deficiency.”
UpToDate accessed on 1/3/2014
http://www.uptodate.com/contents/diagnosis-and-treatment-of-vitamin-b12and-folatedeficiency?source=search_result&search=vitamin+B12+deficiency&selected
Title=1~150
Anemia of chronic disease
Occurs with inflammation (lupus), malignancy, infection
(Tb). But even DM, anemia of elderly.
Mechanism
Cytokines decrease EPO production (relative decrease)
Decreased response to EPO
Interference with Fe absorption and trapping by macrophages
due to increased hepcidin formation
Perhaps some decreased RBC survival
Characteristics
Most normocytic normochromic hypoproliferative – (microcytic
Fe level, TIBC and transferrin saturation (20% low) decreased
but ferritin normal or elevated as acute phase reactant
Decreased absolute retic count, RPI
Usually mild, non-progressive around 11 - (20% < 8%)
Anemia in Malaria
Can cause severe anemia especially in
SSA and often on top of chronic anemia
Multiple mechanisms: acute hemolysis, G6PD deficiency, extravascular clearance in
spleen, intravascular destruction,
suppression of erythropoiesis, others
Fe deficiency may be protective against
malaria infection – reduced parasitemia,
rate of severe malaria by 38%
Especially severe in those with SCD
Anemia in Sickle Cell Disease
Chronic hemolysis with Hct 20-30% and 315% reticulocytosis , elevated indirect bili
2 causes of acute severe anemia - present
with pallor, weakness, lethargy-can be fatal
Splenic sequestration crisis – vaso-occlusion
in spleen with rapid increase in size and drop in
Hgb of at least 2, low platelets, reticulocytosis.
Tend to recur within year
Aplastic crisis – Parvovirus B19 – decreased
reticulocytes. Often need transfusion though
retics return in 2-14 days
G6PD glucose-6-phosphate
dehydrogenase deficiency
Hemolysis precipitated by certain drugs,
infection or occasionally a chronic
hemolytic anemia
13 % of black men and 2% black women
– different genotype in Mediterranean,
Arabic and Asian descent
Primaquine – always check G-6-PD
levels prior to giving
Summary
While anemia can be quite complex, we
presented a fairly simple evaluation of
anemia based on the cell size or MCV
and mechanism of the anemia based on
the retic count of RPI
Anemia is very common with
considerable morbidity around the world
We discussed several specific anemias
especially IDA, it’s causes, prevention,
complications, diagnosis and treatment
Abrams SA. “Iron requirements and iron deficiency in
adolescents.” UpToDate accessed 1/3/2014
http://www.uptodate.com/contents/iron-requirements-andiron-deficiency-inadolescents?source=search_result&search=iron+deficien
cy&selectedTitle=5~150
Brill JR, Baumgardner DJ. “Normocytic Anemia.”
American Family Physician accessed 1/7/2014
http://www.aafp.org/afp/2000/1115/p2255.html
Field JJ, Vichinsky EP, DeBaun MR. “Overview of the
management and prognosis of sickle cell disease.
UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/overview-of-themanagement-and-prognosis-of-sickle-celldisease?source=search_result&search=sickle+cell+disea
se&selectedTitle=4~150
Harper JL. “Pediatric megaloblastic anemia.”
Medscape Reference accessed 1/7/2014
http://emedicine.medscape.com/article/959918
-overview
Inoue S. “Pediatric chronic anemia.”
Medscape reference accessed 1/7/2014
http://emedicine.medscape.com/article/954598
-overview
Kaferle J, Strzoda CE. “Evaluation of
Macrocytosis.” American Family Physician
accessed 1/7/2014
http://www.aafp.org/afp/2009/0201/p203.html
Mahoney DH. “Iron deficiency in infants and young
children: screening, clinical manifestations, and diagnosis.
UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/iron-deficiency-ininfants-and-young-children-screening-prevention-clinicalmanifestations-anddiagnosis?source=search_result&search=iron+deficiency&
selectedTitle=3~150
Mahoney DH. “Iron deficiency in infants and young
children: Treatment.” UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/iron-deficiency-ininfants-and-young-childrentreatment?source=search_result&search=iron+deficiency&
selectedTitle=4~150
Patrick A. “Approach to anaemia Iron-B12-Folate.
Accessed 1/7/2014
http://www.macmurray.co.nz/images/userfiles/file/anaemia
%20and%20B12%20-%20Dr%20Alasdair%20Patrick.pdf
Recht M. “Overview of hemolytic anemia in children.
UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/overview-of-hemolyticanemias-inchildren?source=search_result&search=hemolytic&selecte
dTitle=4~150
Roberts DJ. “Anemia in malaria.” UpToDate accessed
1/7/2014 http://www.uptodate.com/contents/anemia-inmalaria?source=search_result&search=anemia+of+malari
a&selectedTitle=1~150
Sandoval C. “Anemia in children due to decreased red
blood cell production. UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/anemia-in-children-dueto-decreased-red-blood-cellproduction?source=search_result&search=anemia+due+to
+reduced+red+cell&selectedTitle=2~150
Sandoval C. “Approach to the child with anemia.”
UpToDate accessed 1/3/2014
http://www.uptodate.com/contents/approach-to-the-childwithanemia?source=search_result&search=anemia&selectedTi
tle=2~150
Schrier SL. “Anemias due to decreased red cell
production. UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/anemias-due-todecreased-red-cellproduction?source=search_result&search=anemia+due+to
+reduced+red+cell&selectedTitle=3~150
Schrier SL, Camaschella C. “Anemia of chronic disease
(anemia of [chronic] inflammation) UpToDate accessed
1/7/2014 http://www.uptodate.com/contents/anemia-ofchronic-disease-anemia-of-chronicinflammation?source=search_result&search=anemia+of+c
hronic&selectedTitle=1~100
Schrier SL. “Approach to the adult patient with anemia.”
UpToDate accessed 1/3/2014
http://www.uptodate.com/contents/approach-to-the-adultpatient-withanemia?source=search_result&search=adult+anemia&sel
ectedTitle=1~150
Schrier SL. “Approach to the diagnosis of hemolytic
anemia in the adult.” UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/approach-to-thediagnosis-of-hemolytic-anemia-in-theadult?source=search_result&search=approach+anemia&s
electedTitle=3~150
Schrier SL. “Causes and diagnosis of iron deficiency
anemia in the adult.” UpToDate accessed 1/3/2014
http://www.uptodate.com/contents/causes-and-diagnosisof-iron-deficiency-anemia-in-theadult?source=search_result&search=approach+to+the+dia
gnosis+of+iron+deficiency+anemia&selectedTitle=1~150
Schrier SL. “Diagnosis and treatment of vitamin B12 and
folate deficiency.” UpToDate accessed on 1/3/2014
http://www.uptodate.com/contents/diagnosis-andtreatment-of-vitamin-b12-and-folatedeficiency?source=search_result&search=vitamin+B12+de
ficiency&selectedTitle=1~150
Schrier SL. “Etiology and clinical manifestations and
clinical manifestations of vitamin B12 and folate deficiency
UpToDate accessed 1/3/2014
http://www.uptodate.com/contents/etiology-and-clinicalmanifestations-of-vitamin-b12-and-folatedeficiency?source=search_result&search=vitamin+B12+de
ficiency&selectedTitle=2~150
Schrier SL. “Mean corpuscular volume.” UpToDate
accessed 1/7/2014
http://www.uptodate.com/contents/mean-corpuscularvolume?source=search_result&search=mean+corpuscular
&selectedTitle=1~150
Schrier SL, Auerbach M. “Treatment of the adult with iron
deficiency anemia.” UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/treatment-of-the-adultwith-iron-deficiencyanemia?source=search_result&search=iron+deficiency+an
emia&selectedTitle=2~150
Vichinsky EP. “Overview of the clinical manifestations of
sickle cell disease.” UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/overview-of-the-clinicalmanifestations-of-sickle-celldisease?source=search_result&search=sickle+cell&select
edTitle=1~150
Vranken MV. “Evaluation of microcytosis.” American
Family Physician accessed 1/7/2014
http://www.aafp.org/afp/2010/1101/p1117.html
Ware RE. “Autoimmune hemolytic anemia in
children.” UpToDate accessed 1/7/2014
http://www.uptodate.com/contents/autoimmunehemolytic-anemia-inchildren?source=search_result&search=hemolytic+
anemia&selectedTitle=4~150
“Evaluation of the anemic patient.” accessed
1/16/2014
www.medicine.wisc.edu/~williams/anemia1.ppt
“The Reticulocyte count.” All about blood.
Accessed 1/7/2014
http://allaboutblood.com/tag/corrected-reticulocyteindex/
“Reticulocyte index.” Wikipedia accessed 1/7/2014
http://en.wikipedia.org/wiki/Reticulocyte_index
Thalassemias
Check for + FH
Ferritin high or normal
RBC proportionately low in Fe
deficiency, inappropriately high in
thalassemia so > 3 times Hgb
Two types – Alpha and Beta
Beta thal (defect in forming beta
chain of globin)
Beta Thal major serious illness with severe
usually transfusion dependent anemia.
Minor or silent carrier (heterozygote)
Hct: usually > 30
Hgb electrophoresis: A2 and F high
MCV: < 75
RBC: usually increased
Target cells
RDW: usually normal
Risk: overtreating with Fe when not needed
Alpha thal
More complex as there are 4 genes, not 2
– 2 from each parent
4 gene deletion Hgb Barts and fatal early
3 gene deletion Hemoglobin H and severe
2 gene deletion alpha thal minor –
hypochromic microcytic anemia
1 gene deletion silent carrier or minimus –
usually normal; dx only by DNA analysis
Hgb electrophoresis normal
Anemia of Malaria
Major cause of severe malaria
especially in sub-Saharan Africa.
Often on top of already existing chronic
anemia of various etiologies.
Multiple mechanisms causing hemolysis
and bone marrow suppression
Normocytic/normochromic without
reticulocytosis
Multifactorial
Acute hemolysis in Blackwater fever
G-6PD deficiency and use of Quinine
Extravascular clearance (spleen)
Intravascular destruction of RBC
Clearance of uninfected RBC (10 uninfected cells
removed/infected cell
Activation of monocyte/macrophage system
Suppression of erythropoiesis – inadequate EPO,
direct inhibition, dyserythropoiesis, cytokine
suppression, decreased responsiveness to EPO
Iron deficiency
B12 deficiency may contribute
Fe deficiency may be protective against
malaria infection – reduced parasitemia,
rate of severe malaria by 38%, all-cause
mortality by 60%.
Fe supplementation actually increases
malaria morbidity and mortality
Also higher hepcidin – wait till no malaria to
treat with Fe
While SS trait is protective, if one has SCD
and gets malaria, it tends to be much more
severe, deadly than in general population
Hemolytic anemias
Often rapid onset, jaundice, bilirubin
pigment GB stones, splenomegaly,
fragmented cells in peripheral smear
Increased LDH; Reduced haptoglobin
90% specific at diagnosing.
Normal LDH, serum haptoglobin > 25
mg/dl 92% sensitive in ruling out
hemolysis in adults
Many kinds beyond scope of talk
CKD, endocrine disorders can present
similarly
A few need bone marrow to diagnose
Treat underlying condition unless severe
Treat other complicating factors
Occasionally EPO if very low Hgb
If EPO give iron – may need to be
parenteral due to hepcidin blocking
absorption
If rate hemolysis > rate of ability of bone
marrow to replace destroyed cells
develop anemia (AIHA)
CBC, retic, Coombs, urinalysis, blood
smear.
AST and LDH up but not ALT
Some types AIHA respond to steroids
B12 and folate deficiency
Macrocytic anemia with low retic
All with high MCV should have level B12,
folate levels (RBC level better)
B12 variable so if low need two levels
Folate: leafy green veges, fruit and enriched
sources
B12 in animal products, eggs, meat, fish, milk
If not sure true deficiency check homocysteine
and MMA (methylmalanic acid) – both high if
B12 low, homocysteine only if folate deficient
If borderline therapeutic trial reasonable
Can effect all 3 hematopoietic cell lines
B12 low from poor intake, gastrectomy or
gastric bypass, bariatric surgery, H. Pylori,
breastfed, fish tapeworm, drugs (PPI),
Hereditary causes, pernicious anemia
Folate – mainly poor intake and some
drugs (MTX), increased needs, Celiac
Danger is neurological damage from
B12 deficiency which can be permanent
Folate needed in purine synthesis; B12
needed as cofactor in activation of folate
B12 – anemia but not always
Macrocytosis and oval cells
Neuro symptoms
Hypersegmented WBC (> 5 nuclei)
Folate – only anemia symptoms
B12 – neuro sx can be permanent
Glossitis
+ anemia – but more had MCV > 100
Memory loss
Irritability
Ataxia
Dementia
Peripheral neuropathy
Mechanisms of anemia in Sickle
Cell Disease
All have chronic hemolysis with mild-moderate
anemia (Hct 20-30%) and reticulocytosis (3-15%),
elevated unconjugated bili, increased LDH and low
haptoglobin.
Usually normocytic normochromic
High hemoglobin F
2 causes of acute severe anemia and present with
pallor, weakness, lethargy can be fatal
Splenic sequestration crisis – vaso-occlusion in spleen so
size increases rapidly – up to 30% get prior to splenic
fibrosis due to multiple episodes of splenic infarction
(splenic enlargement, drop Hgb of at least 2, low platelets,
reticulocytosis – can get hypovolemic shock. If get one
tend to get recurrence within 12 months
Aplastic crisis – B19 – decreased
reticulocytes < 10,000. Often need
transfusion though retics return in 2-14
days
Some believe a third crisis and some do
not called hyperhemolytic crisis
Teach parents to recognize enlarging
spleen
Fe deficiency in adults
Fe stores in liver, spleen, bone marrow
Normal 3-4 grams
Hgb in circulating cells – 2 grams
Iron containing proteins – 400 mg
Plasma iron bound to transferrin – 3-7 mg
Remainder storage iron in form of ferritin or
hemosiderin.
Stages of iron deficiency
Loss of stores (20% of menstruating women in
U.S. have no stores)
Iron deficient RBC production
After stores gone enough in labile Fe pool to
continue till further losses.
Some with very low ferritin without anemia
have fatigue and decreased exercise tolerance
Further Fe loss- normocytic anemia with
normal absolute retic count (low ferritin, Fe,
high TIBC, low transferrin saturation,
Microcytic anemia with low retic count
For adults draw all at once – CBC,
ferritin, Fe, TIBC
Test of absorption – 325 mg then repeat
Fe 1-4 hours – increase 100 mcg/dL
adequate
Nothing else causes low ferritin levels
Best test is ferritin – if known
inflammation divide by 3
Sensitivity 59%, specificity 99%
Some recommend using higher cutoff to
make more sensitive
Transferrin saturation normal 25-45
High transferrin second in accuracy to
ferritin but BCP and pregnancy raise it
Symptoms
Asymptomatic
HA, weakness, irritability, fatigue
Impaired exercise tolerance
Pica/Pagophagia
Beeturia – excretion of red urine if eats
beets (absorption increased and ferric iron
decolorizes
Fe deficiency can cause RLS – in one
study of 24%, 9X higher than in general
population – may even respond to iron if
not iron deficient
Iron deficiency adult
The safety of routine iron in places with
endemic malaria remains uncertain
Times that intravenous Fe might be
considered: if not tolerating oral iron,
IBD, chemotherapy induced anemia,
unresponsive to oral Fe, if blood loss
exceeds amount one can replace, after
gastric bypass surgery or subtotal
gastric resection
Treatment
Not enteric coated
Not with food (inhibit absorption H2 receptor
blockers, antacids, PPI, Ca, some antibiotics like
tetracycline, fiber, tea, coffee, eggs, milk
Fe ++ best absorbed – give abscorbic acid
If not tolerated:
Try one with less iron like Fe gluconate (28-36 mg)
Try Ferrous sulfate elixir
Give with food
Fe fumarate 106 mg; sulfate 65; gluconate 28-36 mg
elemental iron / tablet
Dose 150-200 / day elemental iron
Lower dose for elderly
If no response
Incorrect diagnosis
Non-adherence
Coexisting disease interfering
Not absorbed for physical reasons
Iron loss > replacement amount
Malabsorption of iron (Celiac)
Inherited condition
Response to treatment
Pagophagia, disappear almost
immediately
Better sense well being first few days
7-10 days maximal reticulocytosis
Retic count increases within 3-5 days
Hgb increases after 1-2 weeks by 2 - 3
gm/dl