Coding to Highest Specificity ICD
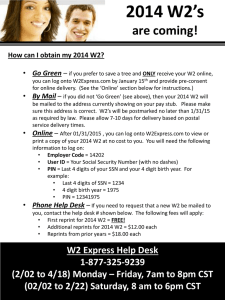
advertisement
Why it is important and how it affects you as a physician. Jeni Smith, CPC Quality Report Suffers It will not paint an accurate picture of the severity of the illnesses Severity of illness is a measure of the patient's overall health status reflected by the resources necessary for care and the risk of morbidity and mortality “severity of illness is understated 8%-15% of the time. Mortality is understated 15%-25% of the time.” (For the Record, page 11) Reporting comorbidities and illness severity will help better define quality of care and medical necessity for that care. RAC Audits 85% of Medicare RAC audit identified overpayments have been directly related to coding, determination of medical necessity and/or a need to enhance detailed documentation gathered in support of submitted claims. RAC took back over $900 Million from hospitals (Took 3 Mil. from AGH) More MCC, can lead to increased level of visit Increases in morbidity, mortality, and length of stay will not correlate with the documented severity of illness which could lead to red flags Transfer to ICD-10 System Inevitable ICD-10 offers more detailed information and the ability to expand specificity Greater specificity and clinical information, which results in: • Improved ability to measure health care services • Increased sensitivity when refining grouping and reimbursement methodologies A code is invalid if it has not been coded to the full number of digits required for that code. Provider reports the full ICD-9-CM ICD-9 codes may have three to five digits depending on their category. Each digit provides important information about the patient's condition. http://www.aafp.org/fpm/990700fm/27.html ICD- D 9-CM Diagnosis Code Descripition (Can be found on lab sheet) 585.1 Stage 1 585.2 Stage 2 (mild) 585.3 Stage 3 (moderate) 585.4 Stage 4 (severe) 585.5 Stage 5 585.6 End Stage Renal Disease 585.9 Chronic Kidney Disease, (unspecified) 250.13, uncontrolled type 1 diabetes with ketoacidosis. Choosing the most specific code means coding only what you know to be a fact. The three-digit code (in this case, 250) represents the diagnostic category. The fourth digit identifies complications associated with diabetes The fifth digit describes the type of diabetes and its level of control. To correctly code an encounter with a patient who has uncontrolled type 1 diabetes complicated by ketoacidosis, you should use all five digits. Patient, follow-up of benign essential hypertension = 401.1 (The fourth digit identifies the disease as benign and thus is the most specific description of your patient's condition) However, patient also has benign hypertensive heart disease, include a fifth digit = 402.10 or 402.11 (depending on the absence or presence, respectively, of congestive heart failure) http://www.aafp.org/fpm/990700fm/27.html You must always code to the highest number of digits that best describe your patient's condition Physicians are legally responsible for the codes selected and submitted to payers. Coding to the highest specificity allows for more accurate report of quality of care and will prepare you for possible RAC audits and the implementation of ICD-10-CM. Heart Failure – Systolic or Diastolic COPD – Need to state acute exacerbation Sepsis – If code as 599.0, translates to UTI -Need to state Sepsis due to UTI CVA – State with Residual or presenting symptoms Anemia – Chronic, Acute blood loss, iron deficiency Pneumonia – Which Bacteria DM – Need type and whether controlled/uncontrolled Morbid Obesity – Must state BMI, can increase reimbursement by thousands (Already calculated on MAR)