Anaerobe
advertisement
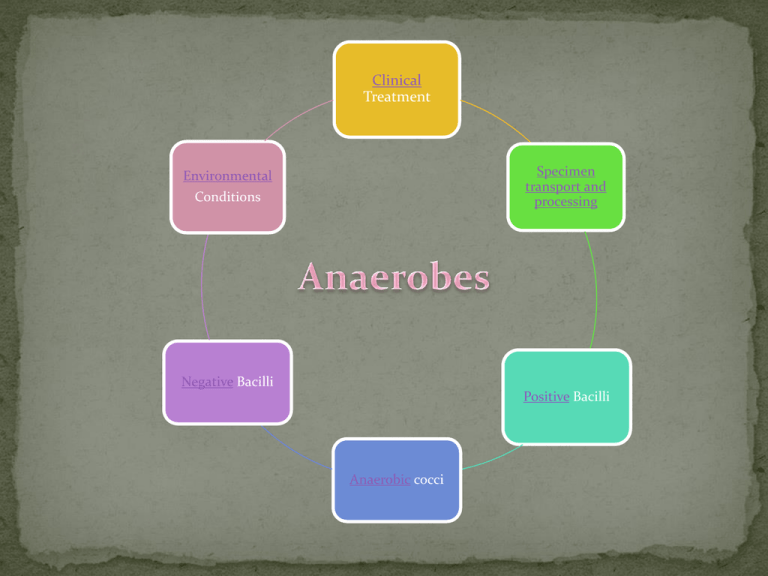
Clinical Treatment Specimen transport and processing Environmental Conditions Negative Bacilli Positive Bacilli Anaerobic cocci Obligate Anaerobes only grow in the absence of oxygen (O2) Aerotolerant / Microaerophilic anaerobes grow in reduced concentration of oxygen (~5% O2), but grow best under strict anaerobic conditions Peptostreptococcus Vieonella??? Get correct spelling Peptostreptococcus (Peptoniphilus) spp. Intestinal gram positive cocci P. anaerobius • Elongated • Produce sweet odor due to the presence of isocaproic acid Key reactions • Nitrate (+) • SPS –sensitive • Indole (-) P. assacharolyticus Form tetrads or pairs Key reactions : SPS resistant, Indole (+), Nitrate (-) Causes: •Head, neck , genital and gut infections Indigenous to oral cavity, upper respiratory, G.I and genitourinary tract Kanamycin (S ) Vancomycin (R ) Colistin (S) Viellonella species Small Gram negative cocci Key reactions •Nitrate (+) •Non-fluorescent, may pigment red Causes : Endocarditis and bacteremia Clostridium species Others ????? Clostridium spp. Gram positive rods Four common species • Clostridium perfringens • Clostridium difficile • Clostridium tetani • Clostridium botulism • Other Clostridium Produce Virulence factors that are responsible for infections Causes : • Food poisoning Spore formers Found commonly in stool specimen •Gas gangrene(myonecrosis) •Neoplasm s •Lock jaw •Pseudomembraneous colitis Appearance: box-shaped gram positive rod Two zone beta hemolytic on SBA Produces alpha and Theta toxin Key reactions: Lecthinase (+), nitrate (+) Reverse camp with group B Strep. Stormy fermentation of litmus milk Kanamycin (S ), Vancomycin (S), Colistin (R) Causes: Gas gangrene, Food poisoning (Enterotoxin A), Soft tissue infections in diabetics and Necrotizing bowel disease Subterminal spore Chartreuse fluorescence Key reactions Ferment fructose Lecthinase (-), Lipase (-) Causes: Pseudomonas colitis and Antibiotic associated diarrhea (AAD) due to enterotoxin A and B Toxin: tetanospasmin (neurotoxic exotoxin) Motile, swarms Appearance: Gram positive rods. Produce terminal spores that appear as drumsticks Biochemical reactions: Lipase (-), Indole (+) Causes: Lockjaw, respiratory failure and tetanus neonatorum Toxin: botulin Key reaction: Lipase (+) Causes: Botulism: Inhibits acetlycholine release from motor neurons Clostridium novyi Clostridium septicum Beta hemolytic Rapid swarmer Characteristic: medusa head, subterminal spores Key reactions: Lecithinase (+), lipase (+), indole (-), urease (-) Causes: Gas gangrene (myonecrosis) and toxic shock Key reactions: Lipase (-), Indole (-) Causes: Neoplasm of the colon, breast leukemia, lymphoma, enterocolitis. myonecrosis Normal flora in the oral cavity, G.I. and female genital tract Key reactions • Catalase (-) •Cephalosporin (R) •Vancomycin (R ) Lactobacillus Gram positive Non-spore forming bacilli Infections caused: Bacterial vaginosis Pelvic inflammatory disease •Protect female genital tract • Produce lactic acid to lower vaginal pH Normal flora of the skin Proprionibacterium acnes Gram positive Non-spore forming bacilli (appear as diptheroids) Reactions • Catalase (+) •Indole (+) •Nitrate (+ ) Can cause: Subacute bacterial endocarditis Bacteremia Bacteroides fragilis Bacteroides ureolyticus Fusobacterium nucleatum Fusobacterium necrophorum Other Fusobacterium Porphyromona spp. Prevotella spp. Gram negative rod Penicillin (R ) Kanamycin (R ) Vancomycin (R ) Colistin (R ) Clindamycin (S) Key reactions •Catalase (+) •Indole (-) •Nitrate (-) Bacteroides fragilis Bile tolerant, Nonmotile Causes : • Inflammation of the intestinal wall • Septic abortion • Thrombosis •G.I. infections Gram negative rod Kanamycin (S ) Vancomycin (R ) Colistin (S) Key reaction •Urease (+) Bacteroides ureolyticus Bile sensitive, Nonmotile Causes : • Respiratory infections •Intestinal tract infections Fusiform Gram negative bacilli Kanamycin (S ) Vancomycin (R ) Fusobacterium nucleatum Colistin (S) Key reactions • Lipase (-) • Indole (+) Causes : Metastatic brain abscess Pleomorphic filamentous gram negative rod Fusobacterium necrophorum Causes : Key reaction •Lipase (+) Pertonsillar abscess in children and young adult Normal flora in the oral, G.I and vaginal area Kanamycin (R ) Vancomycin (R ) Colistin (S) Penicillin (R) Prevotella melaninogenica Gram negative coccobacilli • Produces foul odor • Slow producer of protoporphin Causes : Lung and dental infections Acceptable specimens : Aspirates from sterile site deep wounds , bodily fluids (except urine, sputum and saliva), and suprapubic bladder aspirates Primary media: Brucella (CDC or Schaedler) blood agar- contains hemin, vitamin K and yeast extract. Detect hemolysis in anaerobes Special media: Bacteroides bile esculin (BBE) agar- contains gentamycin (inhibits facultative aerobic gram negative rods ) and 20% bile. Laked Kanamycin Vancomycin (LKV) blood agar – identify pigmented gram negatives . (Kanamycin inhibits facultative gram negative rods and Vancomycin inhibits gram positive rods) Phenyl-ethyl Alcohol (PEA) plate : inhibits swarming Cycloserine cefoxitin fructose (CCFA) agar: selective for Clostridium difficile Egg yolk agar- selective for Lecithinase and lipase production Thioglycollate broth: provides reduced O2 environment Identification tests : Catalase test: distinguish aerotolerant anaerobes from anaerobic organisms Indole: identify organisms that produce tryptophanase (Note: media needs to contain tryptophan) Nitrate test: Urea test: identify organisms that produce urease. Observe pH change. Urea is converted to ammonia Incubate media in anaerobic gas chambers Contains H2, N2, carbon dioxide , palladium catalyst and desiccants (absorb water) Keep media for 7 days Metronidazole – best treatment. Confirms the presence of an anaerobe Clostridium infection: Use antitoxins , antibiotics (i.e. Chloramphenicol, pipercillin, imipramine or ampicillin/sulbactam) and supportive therapy