HCV TRANSFORMING MANAGEMENT IN EGYPT
advertisement

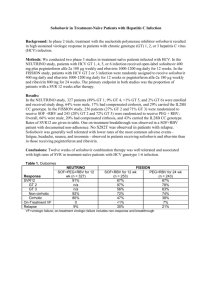
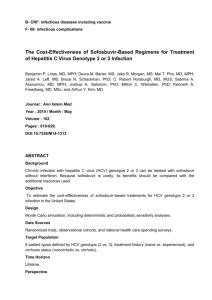
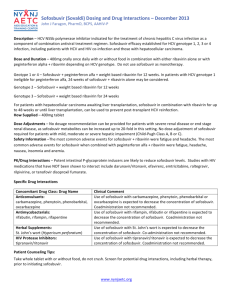
Dr-MOHAMMED EMAM Zagazig university-2014 “We're all really excited that for the first time we have curative therapies for hepatitis C which are much more effective than what we had before and much easier to tolerate,“ “We think the move away from interferon and toward a high probability of success is remarkably encouraging for all of us.... Suddenly, it's true to think that we can cure most patients with hepatitis C," WHERE WE ARE NOW? " " " Sofosbuvir is a game-changer and will allow high cure rates with just 12-week regimens," sofosbuvir holds numerous advantages over current therapy because of its: -Efficacy profile, -Safety, -Tolerability across many different patient populations and HCV genotypes, -Dosing simplicity. - - INDICATIONS AND USAGE : SOVALDI is Indicated for : -Treatment of chronic hepatitis C (CHC) infection as a part of a combination antiviral treatment regimen. Sofosbuvir and Ribavirin in HCV Genotype 4 Egyptian Ancestry Trial: Study Features Egyptian Ancestry Genotype 4 Trial: Features Design: Randomized, open-label, phase 2 study of sofosbuvir + ribavirin in treatment-naïve and treatment-experienced patients with HCV GT 4 Setting: single study center in United States Entry Criteria - HCV Genotype 4 - First generation Egyptian - Treatment naïve or treatment experienced - Age 18 or older - Not co-infected with HIV - Patients with compensated cirrhosis allowed Primary End-Points: Efficacy (SVR12) and safety Source: Ruane P, et al. 49th EASL. April 2014: Abstract P1243. Sofosbuvir and Ribavirin in HCV Genotype 4 Egyptian Ancestry Trial: Baseline Characteristics Chronic HCV GT4: Treatment with Sofosbuvir + Ribavirin Treatment Naive Baseline Characteristic Treatment Experienced 12-Week (n=14) 24-Week (n=14) 12-Week (n=17) 24-Week (n=15) 53 (26-69) 52 (27-75) 54 (32-72) 57 (38-68) 8 (57%) 5 (36%) 14 (82%) 14 (93%) 29.2 30.9 28.1 29.6 Cirrhosis, n % 3 (21%) 3 (21%) 4 (24%) 4 (27%) IL28B non-CC, n (%) 11 (79%) 8 (57%) 16 (94%) 15 (100%) Prior schistosomiasis, n (%) 8 (57%) 3 (21%) 6 (35%) 8 (53%) 5.7 5.9 6.2 6.1 Mean Age, y (range) Male, n % Mean BMI kg/m2 HCV RNA, mean baseline log10 IU/ml Source: Ruane P, et al. 49th EASL. April 2014: Abstract P1243. Sofosbuvir and Ribavirin in HCV Genotype 4 Egyptian Ancestry Trial: Design Week GT 4 Naïve or Experienced 0 12 Sofosbuvir + RBV (n = 32) 24 36 SVR12 Sofosbuvir + RBV (n = 28) SVR12 Drug Dosing Sofosbuvir: 400 mg once daily Weight-Based Ribavirin (in 2 divided doses): 1000 mg/day if < 75 kg or 1200 mg/day if ≥ 75 kg Source: Ruane P, et al. 49th EASL. April 2014: Abstract P1243. Sofosbuvir and Ribavirin in HCV Genotype 4 Egyptian Ancestry Trial: Results SVR 12 by Regimen Duration and Treatment Experience Patients with SVR 12 (%) 100 100 87 80 79 60 59 40 20 0 11/14 14/14 10/17 13/15 SOF + RBV x 12 weeks SOF + RBV x 24 weeks SOF + RBV x 12 weeks SOF + RBV x 24 weeks Treatment Naive Treatment Experienced Source: Ruane P, et al. 49th EASL. April 2014: Abstract P1243. Phase III NEUTRINO study: 96% SVR12 rate in patients with genotype4 HCV treated with sofosbuvir plus pegIFN/RBV for 12 weeks Current pilot study evaluating sofosbuvir plus RBV in immigrants of full Egyptian ancestry in the US infected with genotype 4 HCV " HCV FREE WORLD NO DREAMS WITHOUT PROBLEMS Guidelines for low and middle income countries Most of the existing guidelines for the treatment of hepatitis C have been developed by specialist medical organizations and relate to the treatment of persons with different genotypes and living in high-income countries. There are no evidence-based treatment guidelines that focus on persons living in low- and middle-income countries. The suggestive objective of these guidelines These guidelines will provide a framework for the development or strengthening of hepatitis C treatment programmers' in lowand middle-income countries(especially in Egypt) according to evidence-based recommendations on screening for HCV infection, and the care and treatment of persons with HCV infection aiming to achieve a mass treatment in our locality Price of medicines HCV treatment is expensive. Prices range from US$ 5 000 in Egypt for 48-weeks of PEG/IFN RBV to as much as US$84 000 in the US for a single 12-week course of sofosbuvir. At these prices, these treatments will remain unaffordable for most persons who need treatment. A concerted effort is needed to reduce the price of HCV medicines. The experience with HIV, where the price of antiretrovirals was reduced by nearly a hundred fold through the introduction of generic drugs, has shown that the key to achieving low prices for medicines is to use a multipronged approach.. key to achieving low prices for medicines This can include: 1- Voluntary licensing (where the patent owner licenses the medicine to generics-producing companies or a patent pool), 2- Tiered pricing (where the manufacturer sets different prices for different countries based on their income level and disease burden), 3- compulsory licensing (where a national government grants a license to companies producing generic drugs or importing the product 4-National governments, international agencies, donors, civil-society organizations, and the pharmaceutical industry will need to work together to help assure that hepatitis C treatment is affordable and accessible for all those who need treatment. The primary goal of HCV therapy is to cure the infection. A sustained virological response (SVR) is defined as undetectable HCV RNA 12 weeks (SVR12) or 24 weeks (SVR24) after treatment completion. The infection is cured in more than 99% of patients who achieve an SVR. The SVR is generally associated with resolution of liver disease in patients without cirrhosis. Patients with cirrhosis remain at risk of lifethreatening complications; however hepatic fibrosis may regress and the risk of complications such as hepatic failure and portal hypertension is reduced. More data is required to ascertain the lifetime residual risk of hepatocellular carcinoma after viral infection has been eradicated . In addition to pegylated IFN-α and ribavirin, three new HCV DAAs licensed in the first half of 2014, for use as part Of combination therapies for HCV infection. 1-Sofosbuvir, a nucleotide analogue inhibitor of HCV RNAdependent RNA polymerase, has been approved in January 2014. 2-Simeprevir, a second-wave, first generation NS3/4A protease inhibitor approved in May 2014. 3-Daclatasvir, an NS5A inhibitor, is likely to be approved in August or September 2014. Other drugs may be approved later in 2014 or in 2015. Who should be treated? All treatment-naïve and -experienced patients with compensated disease due to HCV should be considered for therapy (Recommendation A1) • Treatment should be prioritized for patients with significant fibrosis (METAVIR score F3 to F4) (Recommendation A1) • Treatment is justified in patients with moderate fibrosis (METAVIR score F2) (Recommendation A2) • In patients with no or mild disease (METAVIR score F0-F1), the indication for and timing of therapy can be individualized. • Patients with decompensated cirrhosis who are on the transplant list should be considered for IFN-free, ideally ribavirinfree therapy Available drugs (approved by before the end of 2014 Pegylated IFN-α2a should be used at the dose of 180 μg/week, whereas pegylated IFN-α2b should be used at the weight-based dose of 1.5 μg/kg/week. Ribavirin dose should be 1000 or 1200 mg/ day, based on body weight (<75 kg or ≥75 kg, respectively). Sofosbuvir should be administered at the dose of 400 mg (one tablet). Sofosbuvir should be administered at the dose of 400 mg (one tablet) Once per day., No dose recommendation can be given for patients with severe renal impairment (estimated glomerular filtration rate <30 ml/min/1.73m2) or with end-stage renal disease due to higher exposures (up to 20-fold) of the predominant sofosbuvir metabolite. . Sofosbuvir. Sofosbuvir is well tolerated over 12 to 24 weeks of administration. The most common adverse events (≥20%) observed in combination with ribavirin were fatigue and headache. The most common adverse events (≥20%) observed in combination with pegylated IFN-α and ribavirin were fatigue ,headache, nausea, insomnia, and anaemia. Simeprevir should be administered at the dose of 150 mg (one capsule) once per day. No dose recommendation can be Given for patients with Child-Pugh Class B or C cirrhosis, due to Higher simeprevir exposures (particularly in Child-Pugh C patients) that may be associated with increased frequency of adverse reactions. . Simeprevir. is well tolerated. Adverse reactions With at least 3%higher frequency in patients receiving simeprevir in Combination with pegylated IFN-α and ribavirin were rash(including photosensitivity), pruritus and nausea. Because simeprevir is an inhibitor of the transporters ( MRP2,) mild, transient Hyper bilirubinaemia not accompanied by changes in other liver parameters was observed in 10% of cases. Daclatasvir should be administered at the dose of 60 mg (one tablet) once per day. It is overall well tolerated. Dose adjustments are not needed in patients with Child B or C disease. The most frequently reported side effects with daclatasvir were fatigue, headache, and nausea. Little information has been released on daclatasvir drug-drug interactions. 2014 Treatment of chronic hepatitis C -G4 Broad choice of drug combinations 2014 Genotype 4 , 6 Options Genotype 4 , Option 1 weekly pegylated IFN-α, daily weight-based ribavirin (1000 or 1200 mg in patients<75 kg or ≥75 kg, respectively), and daily sofosbuvir (400 mg) 12 weeks Whether longer treatment duration would be needed in the most difficultto-treat population is unknown NO STOPPING RULES IS RECOMMENDED Genotype 4 , Option 1 Comments: This combination has been evaluated in the NEUTRINO Phase III trial in treatment-naïve patients The SVR rate in genotype 4 patients was 96% . Whether longer treatment duration would be needed in the most difficult-to-treat population is unknown Genotype 4 , Option 2 weekly pegylated IFN-α, daily weight-based ribavirin (1000 or 1200 mg in patients<75 kg or ≥75 kg, respectively), and daily semiprevir (150 mg) 12 weeks Semipervir should be continued alone for an in naïve and relapser12 weeks(total duration 24 weeks)An additional 36 weeks (total treatment duration 48 weeks) in prior partial and null responders, including cirrhotics HCV RNA levels should be monitored on treatment. Treatment should be stopped if HCV RNA level is ≥25 IU/ml at treatment week 4, week 12 or week 24 Genotype 4 , Option 2 Comments: Indeed, SVR was achieved in 89% (31/35) of treatment-naïve patients, 86% (19/22) of prior relapsers, 100% (10/10) of prior partial responders, and 75%, (30/40) of prior null responders. Genotype 4 , Option 3 weekly pegylated IFN-α, daily weight-based ribavirin (1000 or 1200 mg in patients<75 kg or ≥75 kg, respectively), and daily daclatasvir (60 mg) 12 weeks patients who do not achieve an HCV RNA level <25 IU/ml at week 4 and undetectable at week 10 Daclatasvir should be continued in combination with pegylated IFN-α and ribavirin an additional 12 weeks(total duration 24 weeks) patients who achieve an HCV RNA level <25 IU/ml at week 4 and undetectable at week 10 Pegylated IFN-α and ribavirin should be continued alone between week 12 and 24 (total duration 24 weeks) Genotype 4 , Option 3 Comments: Although this combination is theoretically effective, few data is available. The SVR rate was 100% (12/12) in the COMMAND-1 trial Genotype 4 , Option 4 Patients infected with HCV genotype 4 who are IFN intolerant or -ineligible Daily weight based ribavirin (1000 or 1200 mg in patients <75 kg or≥75 kg, respectively), and daily sofosbuvir (400 mg) 24 weeks No available trials with simeprevir or dalactaasvir Genotype 4 , Option 4 Comment: Only preliminary data is available (SVR at week 4 post-treatment) in a small number of American patients of Egyptian ancestry The preliminary SVR rates were 79% (11/14) and 100% (14/14) after 12 and 24 weeks of treatment, respectively, in treatment-naïve patients, and 59% (10/17) and 93% (14/15) after 12 and 24 weeks, respectively, in treatment-experienced patients Genotype 4 , Option 5 Patients infected with HCV genotype 4 can be treated of daily sofosbuvir (400 mg) and daily simeprevir (150 mg) 12 weeks There is no data on the impact of adding ribavirin to this regimen Ribavirin should be considered in patients with predictors of poor response to antiHCV therapy, especially prior nonresponders and/or patients with cirrhosis Genotype 4 , Option 5 Comments: There is no data with this combination in patients infected with HCV genotype 4. Nevertheless, given the antiviral effectiveness of both sofosbuvir and simeprevir against this genotype, it is likely that the results of the COSMOS trial in patients infected with genotype 1 can be extrapolated Genotype 4 , Option 6 interferon-free combination of daily sofosbuvir (400 mg) and daily daclatasvir (60 mg) 12 weeks in treatment-naïve patients or 24 weeks in treatment-experienced There is no data on the impact of adding ribavirin to this regimen Ribavirin should be considered in patients with predictors of poor response to anti-HCV therapy, especially prior non-responders and/or patients with cirrhosis Genotype 4 , Option 6 Comments: There is no data with this combination in patients infected with HCV genotype 4. Nevertheless, given the antiviral effectiveness of both sofosbuvir and daclatasvir against this genotype, it is likely that the results in patients infected with genotype 1 can be extrapolated. Post-treatment follow-up of patients who achieve an SVR Non-cirrhotic patients who achieve an SVR should be retested for HCV RNA at 48 weeks post-treatment. If HCV RNA is still not detected, the infection can be considered as definitely eradicated and HCV RNA need not be retested. As hypothyroidism may occur after stopping IFN therapy, thyroxin and TSH levels should also be assessed 1and 2 years after treatment if the patient has received IFN. Cirrhotic patients who achieve an SVR should remain under surveillance for HCC every 6 months by ultrasound, and for oesophageal varices by endoscopy if varices were present at pretreatment endoscopy (though first variceal bleed is seldom observed after SVR). The presence of cofactors of liver disease, such as history of alcohol drinking and/or type 2 diabetes may determine that additional assessments are necessary Perspective of new treatments -A large number of other HCV drugs have reached late clinical development. Phase III data have been presented for the combination of pegylated IFN-α, ribavirin and faldaprevir. - Phase III data presented in April 2014 for the fixed-dose combination of sofosbuvir and ledipasvir, and for the three-drug combination of ritonavir, boosted ABT-450, ombitasvir (formerly and dasabuvir. A large number of additional Phase II data has been and will be presented with other HCV drugs in development. These recommendations will be updated regularly, following approval of new drug regimens by the European Medicines Agency New EGYPTIAN guidelines for management of HCV اللجنة القومية لمكافحة الفيروسات الكبدية 1-Priority for treatment :will be directed towards patients with F3 and F4. 2. No differentiation in treatment priority will be established based on the previous treatment experience. . 3. Assessment of fibrosis stage: will be performed by using a combination of both Fibro scan results and FIB 4 score. F3 & F4 stage will be considered if both Fibro scan result is more than 9.5 and FIB4 score is more than 1.45. If both results are below these cut-off values, patient will not be assigned as a treatment priority. If one of these two methods is above the cut- off values while the other is below, performing liver biopsy or reassessment after one year is recommended to rule out the fibrosis stage of the patient. . . 5. Patients who are eligible to receive Interferon (according to the currently used inclusion/ exclusion criteria for combined INF/RBV treatment ) will be treated with: Daily sofosbuvir (400 mg) and weight-based RBV (1000 mg [ <75 kg ] to 1200 mg [˃75 kg]) plus weekly PEG for 12 weeks. 6.Recommended regimen for patients who are not eligible to receive Interferon is : Daily sofosbuvir (400 mg) and weight-based RBV (1000 mg [ <75 kg ] to 1200 mg [˃75 kg]) for 24 weeks. Inclusion criteria for treatment: will be expanded to adapt for more advanced liver fibrosis patients (who will be treated with interferon free regimen ) as defined with the presence of all the following a-Child score up to 8 b) Total bilirubin < 3 c) Albumin ≥ 2.5 d) Platelet count ≥ 50.000 e) Prothrombin concentration ≥ 50% f) Hemoglobin concentration ≥ 10 mg Otherwise, waiting for new DAAs combination is advised . 7. Patients with more decompensated liver disease: will be exluded from treatment until enough data will be available and this will be applied to: a) Child C patients with scores ≥ 9 b) Presence of ascites (except after control ) c) Patients with HCC except after successful radical curative intervention (4 months after resection or successful local ablation ) d) Presence of large risky esophageal varices (except after prophylactic management ) . 9. Governmental fund supports: will be issued on 2 bases; for the value of the interferon based regimen (for interferon eligible patients ) and for the value of interferon free regimen (for interferon ineligible patients ) according to the aforementioned inclusion / exclusion criteria. The same rules will be applied for all patients regardless the source of payment and there will be on role for patients preferences in deciding the treatment regimen. 8. Age limits for treatment: legibility will be above 18 years and below 70 years for all patients while BMI will be accepted up to 35. . 10-For special population groups: priority for treatment will be awarded for post liver transplantation, post kidney transplantation patients and combined HCV/HBV infection regardless the fibrosis stage. Other groups, like pediatric age group and kidney disease patients will be kept for discussion after the availability of enough data . 11- Patients with documents extra-hepatic manifestations: will be prioritized for treatment according to the same guidelines. 12. Treatment experienced patients: should not start evaluation for new treatment regimens except after 6 months from cessation of interferon therapy .