The Cost-Effectiveness of Sofosbuvir
advertisement

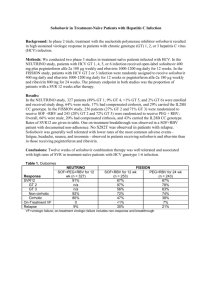
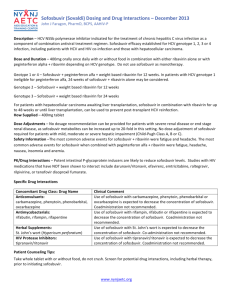
B- CRF: infectious diseases including vaccine F- 08: infectious complications The Cost-Effectiveness of Sofosbuvir-Based Regimens for Treatment of Hepatitis C Virus Genotype 2 or 3 Infection Benjamin P. Linas, MD, MPH; Devra M. Barter, MS; Jake R. Morgan, MS; Mai T. Pho, MD, MPH; Jared A. Leff, MS; Bruce R. Schackman, PhD; C. Robert Horsburgh, MD, MUS; Sabrina A. Assoumou, MD, MPH; Joshua A. Salomon, PhD; Milton C. Weinstein, PhD; Kenneth A. Freedberg, MD, MSc; and Arthur Y. Kim, MD Journal : Ann Intern Med. Year : 2015 / Month : May Volume : 162 Pages : 619-629. DOI:10.7326/M14-1313 ABSTRACT Background Chronic infection with hepatitis C virus (HCV) genotype 2 or 3 can be treated with sofosbuvir without interferon. Because sofosbuvir is costly, its benefits should be compared with the additional resources used. Objective To estimate the cost-effectiveness of sofosbuvir-based treatments for HCV genotype 2 or 3 infection in the United States. Design Monte Carlo simulation, including deterministic and probabilistic sensitivity analyses. Data Sources Randomized trials, observational cohorts, and national health care spending surveys. Target Population 8 patient types defined by HCV genotype (2 vs. 3), treatment history (naive vs. experienced), and cirrhosis status (noncirrhotic vs. cirrhotic). Time Horizon Lifetime. Perspective Payer. Intervention Sofosbuvir-based therapies, pegylated interferon–ribavirin, and no therapy. Outcome Measures: Discounted quality-adjusted life-years (QALYs), costs, and incremental cost-effectiveness ratios (ICERs). Results of Base-Case Analysis The ICER of sofosbuvir-based treatment was less than $100 000 per QALY in cirrhotic patients (genotype 2 or 3 and treatment-naive or treatment-experienced) and in treatment-experienced noncirrhotic patients but was greater than $200 000 per QALY in treatment-naive noncirrhotic patients. Results of Sensitivity Analysis The ICER of sofosbuvir-based therapy for treatment-naive noncirrhotic patients with genotype 2 or 3 infection was less than $100 000 per QALY when the cost of sofosbuvir was reduced by approximately 40% and 60%, respectively. In probabilistic sensitivity analyses, cost-effectiveness conclusions were robust to uncertainty in treatment efficacy. Limitation The analysis did not consider possible benefits of preventing HCV transmission. Conclusion Sofosbuvir provides good value for money for treatment-experienced patients with HCV genotype 2 or 3 infection and those with cirrhosis. At their current cost, sofosbuvir-based regimens for treatment-naive noncirrhotic patients exceed willingness-to-pay thresholds commonly cited in the United States. Primary Funding Source National Institute on Drug Abuse and National Institute of Allergy and Infectious Diseases. COMMENTS. Sofosbuvir, a nucleotide analogue inhibitor of hepatitis C virus (HCV) NS5B polymerase with activity against all HCV genotypes. In combination with ribavirin, sofosbuvir can be used to treat patients with chronic HCV genotype 2 or 3 infection without interferon, yielding cure rates greater than with the previous standard of care. Cure, also known as sustained virologic response (SVR), is associated with a greatly reduced lifetime risk for liver-related morbidity and mortality and increased short-term survival for patients with advanced liver disease (cirrhosis and cancer). These are very spectacular results, obtained without interferon therapy which is frequently toxic. Nethertheless, sofosbuvir currently costs approximately $1000 per tablet, or $28 000 for 4 weeks in the USA. Several state Medicaid programs recently announced that sofosbuvir will be available only to patients with advanced liver disease. The goal of the studyl was to evaluate the cost-effectiveness of sofosbuvir-based treatment strategies for patients with HCV genotype 2 or 3 infection to identify approaches that would maximize the number of patients who achieve HCV cure, given competing demands on resources. A model was constructed and performed analyses were made using TreeAge Pro 2012 software (TreeAge Software). Quality of life (QoL) reflected the combination of 3 independent utility functions, which were combined multiplicatively. First, was considered utility related to non-HCV comorbid conditions; all simulated persons had a “background” QoL that was a function of age and sex. Second, was considered HCV-specific utility; HCV-related QoL was a function of fibrosis stage, with progressively lower utility with advancing disease. Third, was considered treatment-related utility. All patients had decreased QoL while receiving HCV therapy, which reflected the disutility of treatment adverse effects. Quality of life during interferon-free treatment was higher (multiplier, 0.99) than during therapy involving interferon (multiplier, 0.88). At its current cost, sofosbuvir-based HCV therapy improves outcomes and provides good economic value in patients with cirrhosis and genotype 2 or 3 infection and in those who were previously treated with interferon. However, in treatment-naive noncirrhotic patients, for whom pegylated interferon–ribavirin remains a treatment option, the ICER of sofosbuvir-based therapy for genotype 2 or 3 infection is well over $100 000 per QALY. These conclusions were robust to sensitivity analyses that incorporated uncertainty around treatment efficacy, mortality, QoL, and costs. In summary, this analysis shows that at its current U.S. cost of $28 000 for 4 weeks of therapy, sofosbuvir-based treatment for HCV genotype 2 or 3 infection extends QALE and provides good value for money in cirrhotic patients and in treatment-experienced patients. Among treatmentnaive noncirrhotic patients, however, the ICER of sofosbuvir-based treatments exceeds the commonly cited U.S. willingness-to-pay threshold of $100 000 per QALY gained. One option for using sofosbuvir is to treat only cirrhotic patients and those who have previously not benefitted from interferon: To conclude, the Editor outlines the following points: Sofosbuvir effectively treats chronic infection with hepatitis C virus (HCV) genotype 2 or 3 but is expensive. The investigators used models to estimate the cost-effectiveness of alternative therapies and found that sofosbuvir is worth the extra cost when compared with the combination of pegylated interferon and ribavirin for some patients. This type of analysis requires many assumptions. Sofosbuvir provides good value for patients with HCV genotype 2 or 3 infection when the patient has cirrhosis or when the patient does not have cirrhosis but has not benefitted from other treatments Pr. Jacques CHANARD Professor of Nephrology