Understanding the Evolving Rural Marketplace
advertisement

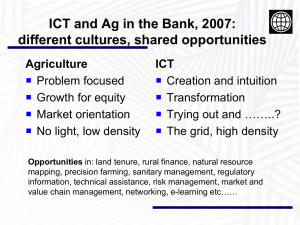
Understanding the Evolving Rural Marketplace Cost, Quality, Access, and Population Health Andrew Busz, FAHM, Policy Director, Finance Ian Corbridge, RN, MPH, Policy Director, Clinical Issues June 24, 2014 How is Rural Different? Geography Population/Demographics Payor Mix Volume of services- Impact on cost per unit due to higher proportion of overhead costs Capitation and risk sharing difficult due to low enrollment numbers. The Jigsaw Puzzle of Provider Types in Rural Areas. • Combines different approaches to ensure access to care in rural areas. • The mix of provider types and degree of collaboration is unique to each community. Critical Access Hospitals Restricted in some ways, granted greater flexibility in others compared to larger hospitals Cost-based payment for Medicare and Medicaid Federally Qualified Health Centers Specific board structure, including consumers Serves underserved clientele in urban and rural areas Provides wrap-around services Required to take all comers on a sliding-scale basis Paid an encounter rate by Medicare and Medicaid FFS, rather than fee schedule Rural Health Clinics Required to employ or contract with mid-level providers (PA or ARNP) Paid an Encounter Rate by Medicare and Medicaid FFS, rather than fee schedule Encounter rate for hospital-based RHCs reflects hospital cost component Free Clinics Primary clientele is uninsured population Primary financial support through donations or hospital sponsorship Clinical care provided by area providers on a volunteer basis Many now closing due to ACA coverage expansions Independent Physicians and Clinics Paid regular fee schedule by Medicare, Medicaid, and Commercial Insurance Increasingly rare in rural areas due to payor mix Public Health and Social Service Agencies Publically funded Focus on population health and preventative services Provides services generally not covered by insurance Regional Support Networks and Community Mental Health Funded directly by the state Regionally organized Generally coordinated with, rather than integrated with medical services Population Health and Quality in Rural Areas – the Current Environment A Health Snapshot County Health Rankings, accessed on 6/1/14 http://www.countyhealthrankings.org/resources What Influences Health County Health Rankings, accessed on 6/1/14 http://www.countyhealthrankin gs.org/resources Funding Population Health National Health Expenditures 2010 Other 14% • Poor incentives • Eroding funding for public health Public Health 3% • Grants, are they a solution or a double edged sword Personal Health Care 83% CDC, accessed on 6/1/14 http://www.cdc.gov/nchs/data/hus/hus13.pdf#112 Community Health Needs Assessment – A Brief Look Priority 2 Priority 1 0 5 10 15 20 25 Health Promotion Behavioral Health Obesity Tobacco Use Chronic Disease Social Determinants of Health/Health Disparities Access to Care 30 Population Health Quality • USPSTF prevention screening recommendations are free under the ACA… however • Poor prevention screening across the state • Rural residents are less likely to receive preventive services The Commonwealth Fund and NORC, accessed on 6/1/14 http://www.commonwealthfund.org and http://NORC.org Population Health Quality (cont’d) Mammography Screening County Health Rankings, accessed on 6/1/14 http://www.countyhealthrankings.org/resources Rural Quality Measurement • Largely sheltered from national level measurement • Us-side vs. Down-side • Challenge of the “small N” • Few rural specific measures • NQF website – 7 measures tagged with a “rural” designation • Total NQF measures = 637 • Are rural specific measures needed? The Managed Care Environment Managed Care Plans Defined population and benefits Historically focused on per unit costs Short term return horizon Risk avoidance Historically not responsible for global issues such as uninsured costs, teaching costs, or overall population health Current Managed Care Workarounds for Rural Providers Medicare Advantage: based on FFS cost-based or encounter rates Medicaid: enhancement/reconciliation to shield plans from higher per unit costs Commercial: percent of charge rather than prospective arrangements Threats to Critical Access Hospitals Cost-based payment/ geographic restrictions Provider supervision changes Length of stay restrictions/ 96 hour rule Inadequate network adequacy standards Threats to FQHCs and RHCs “The FQHC/RHC’s unique payment methodology does not always promote efficiency and value and increasingly impedes some state’s evolving delivery system and payment transformations.” 2/24/2014 letter from National Association of Medicaid Directors to HHS Making the Transition Accountable Care Organizations Requires large population/geography Requires sophisticated data, contracting, and EHR capabilities Ability to provide full range of services Barriers: Lack of data to manage care Restrictions on clinical integration State Health Care Innovation Project (SHCIP) and Transformation All-payor Database –Claims data Availability and sharing of EHR data Role of Accountable Communities of Health (ACH) Proper allocation of funding that targets root determinants of health while maintain viability of medical infrastructure and access to care What Direction Will Things Take? Provider Payor Plan ACO ACH Population Health and Quality in the Emerging World Supporting Population Health • Health care will have greater accountability for the health of a community • Do we have the right: • Partners, • Resources, and • Payment structure… To deliver population health? Improving Population Health – Federal Efforts • ACA • Public Health Fund • Free prevention screening (SUPSTF A & B) • CMS Innovation Center – State Innovation Models (SIM) program grants • Greater focus on population health measures Improving Population Health (cont’d) – State and Local Efforts • State Innovation Bill (2572) • • • • Communities of health Extension program All payer claims database Common performance measures • Behavioral Health Integration Bill (6312) • State SIM grant application – core focus areas: tobacco use, obesity and diabetes… Opportunities to Enhance Rural Population Health Improvement Efforts • Local collaboratives with broad representation • Increased focus on screening and prevention • Measurement • Rural specific measures • Focus on ambulatory care and screening measures • Use of HIT and new data systems to track and improve quality WSHA – Leading Population Health for our Members • WSHA will: • Explore state wide population health goal • Help support partnerships and collaboration • Toolkit to support community engagement • Support the dissemination and spread of new ideas/best practices across stakeholders • Work toward aligning incentives to support population health Questions and Comments Andrew Busz andrewb@wsha.org Ian Corbridge ianc@wsha.org