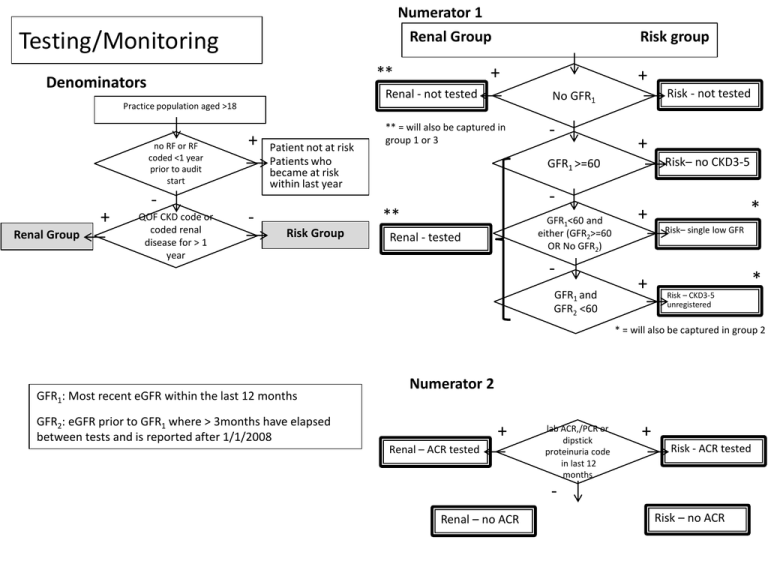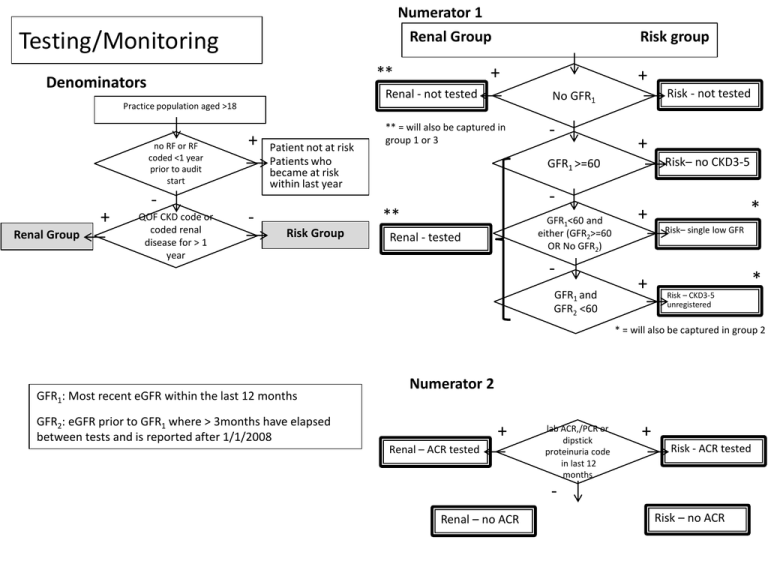
Numerator 1
Testing/Monitoring
Renal Group
+
**
Denominators
Risk group
Renal - not tested
no RF or RF
coded <1 year
prior to audit
start
+
Renal Group
QOF CKD code or
coded renal
disease for > 1
year
-
Patient not at risk
Patients who
became at risk
within last year
** = will also be captured in
group 1 or 3
-
+
Risk– no CKD3-5
GFR1 >=60
**
Risk Group
Risk - not tested
No GFR1
Practice population aged >18
+
+
GFR1<60 and
either (GFR2>=60
OR No GFR2)
Renal - tested
GFR1 and
GFR2 <60
*
+
Risk– single low GFR
+
*
Risk – CKD3-5
unregistered
* = will also be captured in group 2
GFR1: Most recent eGFR within the last 12 months
Numerator 2
GFR2: eGFR prior to GFR1 where > 3months have elapsed
between tests and is reported after 1/1/2008
+
Renal – ACR tested
lab ACR,/PCR or
dipstick
proteinuria code
in last 12
months
+
Risk - ACR tested
Renal – no ACR
Risk – no ACR
Group 1 Coded CKD
Denominator
Practice CKD QOF register, age >18
Numerator
Practice CKD QOF register
+
Coded – no GFR past 2 year
No GFR1
-
+
GFR1 >=60
GFR1: Most recent eGFR within the last 24 months
GFR2: eGFR prior to GFR1 where > 3months have elapsed
between tests and is reported after 1/1/2008
No GFR2 OR
GFR2>=60
Coded- CKD3-5
Coded – no CKD 3-5
based on last GFR
+
Coded- single GFR
Group 2 Uncoded with CKD
Numerator
Denominator
Uncoded patients
Practice population aged >18
on QOF CKD
register
+
Patients with registered CKD 3-5
Uncoded patients
GFR1: Most recent eGFR within the last 24 months
GFR2: eGFR prior to GFR1 where > 3months have elapsed
between tests and is reported after 1/1/2008
GFR1 <60 and
either (No GFR2
OR GFR2>=60)
GFR1 and
GFR2 <60
+
Uncoded – single low GFR
+
Uncoded – CKD3-5
Group 3 Early CKD
Denominator
Practice population aged >18
on QOF register
or uncoded
(group1 and 2)
+
CKD captured elsewhere
coded as CKD
stage 1/ 2
+
Numerators
Early – CKD coded
+
coded with renal
disease code
Early – non CKD coded
Data extract for all cases (numerators and denominators)
Data extract
practice
date of extraction
NHS number
postcode
DOB
NHS no.
age
Can we identify nursing home residents?
sex
weight/bmi plus date
ethnicity
smoking status plus date
risk factors (appendix 1)
date of risk factor
first QOF CKD code
date of first QOF code
most recent QOF CKD code
date of recent QOF code
renal disease code (appendix 2)
date of renal code
CKD 1/2 code (appendix 3)
date of CKD 1/2 code
proteinuria/dipstick code (appendix 4)
date of proteinuria code
GFR1 and GFR2 (N.B. these values are different in the ‘testing’ algorithm
from the ‘group’ algorithm
creatinine on same dates
date of GFR1 and GFR2
most recent ACR or PCR
date of ACR/PCR
Risk Factors
Risk Factors (RFs):
Hypertension
Diabetes
Gout
IHD, congestive cardiac failure, atrial fibrillation
Cerebrovascular disease
Peripheral arterial disease
Kidney stones
Prostatic hypertrophy
Prescription of lithium last 1 year
Prescription of tacrolimus or cyclosporin last 1 year
Systemic lupus erythamatosis and connective tissue diorders
Agreed Exclusions (as to 29/5/13)
family history – inadequate data available to GPs
NSAIDs – inadequate coding (non-prescription use, prescription but no use)
Haematuria – impossible to interpret
Conditions with renal involvement which will be under the care of a hospital specialist:
• sarcoid
• amyloid
• myeloma
• TB
Renal disease codes
[This list needs populating from the meeting 29/5/13]
Inclusions (agreed 29/5/13):
DM with microalbuminuria
Systemic disease coded only where nephritis/renal involvement
is specified.
Alports, Cystic disease, Fabry’s
identification of the risk factor). Of those with an eGFR<60 on initial testing a repeat measurement within
14 days. Of those with a ACR>30<70 (or PCR >50<100) a repeat test within 3 months.
(ii) Denominator: All patients over 18 not on the pre-existing practice CKD3-5 register, not on dialysis and
not transplanted.
Numerator: Patients with two eGFR measurements <60mL/min at least 3-months apart during the last 7
years.
2. Proteinuria
Appropriate Staging.
Codes
Denominator:
Those
the CKD3-5
practice register.(as a renal condition) and codes
This is both aoncode
for proteinuria
Numerator: No. of patients appropriately staged with reference to the two most recent eGFR
for dipstick
positive
(>1+).
[Sally to update]
measurements
at least
3-monthsproteinuria
apart within the
last 2 years
3. Prevalence of identified CKD stage 1 and 2.
Denominator:
All patients
over 4676
18.
467, 4672
to 4675,
to 4678, 467A, 467E, 467H
Numerator: Number of patients eGFR>60mL/minute with the following read codes listed below* and
those with ACR > 30 or PCR> on 2 occasions >3-months apart within last year. Exclude those ACR<30
(PCR<50) on 2 occasions > 3-months apart within the last year.
1Z11.00
Chronic kidney disease stage 2
1Z10.00
Chronic kidney disease stage 1
1Z1A.00
Chronic kidney disease stage 2 without proteinuria
1Z19.00
Chronic kidney disease stage 2 with proteinuria
1Z18.00
Chronic kidney disease stage 1 without proteinuria
1Z17.00
Chronic kidney disease stage 1 with proteinuria
1Z19.11
CKD stage 2 with proteinuria
1Z1A.11
CKD stage 2 without proteinuria
1Z17.11
CKD stage 1 with proteinuria
CKD stage 1/2 codes
CKD
stage
1 without
*The audit will also look
at renal
diagnostic
codesproteinuria
recorded by GP’s.
Investigation and referral
4. Monitoring CKD.
Denominator: All patients with CKD (i.e. patients on the CKD 3-5 register and those identified in 1(ii) and 3)
but excluding those receiving hospital follow-up in outpatient nephrology more than once/year (HES
linkage).
Numerator: Those patients receiving eGFR monitoring at least as frequently as recommended by
guidelines (see chart from KDIGO) within the last year:
Heamaturia codes
Page 43 of 46
Staging
Numerator
Denominator
Confirmed CKD 3-5
Uncoded – CKD3-5
+
=
+
Confirmed CKD3-5
CKD 3a
GFR1 >=45
Coded- CKD3-5
-
+
CKD 3b
GFR1 >=30
GFR1 >=15
GFR1: Most recent eGFR within the last 24 months
CKD 5
+
CKD 4
Monitoring
This has now been incorporated into the testing algorithm (first
slide). It therefore excludes patients with low GFR but without a
QOF code or a renal disease code. [agreed 6 July]
BP control
Blood Pressure
+
<=130
systolic
and <=80
diastolic
Denominator
Group 2 Uncoded – CKD3-5
+
+
Group 1 Coded- CKD3-5
=
All CKD
+
ACR>=30
(PCR>=50),
proteinuria
code or
diabetes code
Contraindication to ACE/ARB
BP subopt
BP control
+
-
Non-proteinuric CKD
Group 3 CKD1/2
Collect: Antihypertensive medication classes
Angiotensin Converting Enzyme
Angiotensin Receptor Blocker
Alpha Blocker
Beta Blocker
Calcium Channel Blocker
Diuretic
Aldosterone antagonists
Other Antihypertensive
-
Proteinuric CKD/DM
<=130
systolic
and <=80
diastolic
-
Last systolic BP
Last diastolic BP
BP subopt
Referral
Denominator
All CKD
Referred or
reviewed by
nephrology/diabet
es specialist in last
24 months
Referred
GFR1: Most recent eGFR within the last 12 months
eGFR1<30
(GFR2 – GFR1) >5 and GFR1 is <45ml/min
Taking 4 antihypertensive classes (see previous) and last
BP>140/90 in last 12 months
ACR>=70 (PCR>=100) and no diabetes in last 12 months
ACR>=30 (PCR>=50) and heamaturia code in last 12 months
Coded genetic kidney disease – see renal disease codes
GFR2: eGFR prior to GFR1 where > 3months but <15months
have elapsed between tests
CV risk
All CKD
No code for IHD,
CCF, AF, PVD,
cerebrovasc
disease
CV risk - secondary
additionally collect:
aspirin prescription
contraindication to aspirin prescription – eg GI
bleeding/ulcer
warfarin/clopidogrel prescription
CV risk - primary
CV risk
assessment
e.g Q risk,
framingham
CV primary assessed
collect:
statin prescription
contraindication to statin prescription
exercise advice/weight loss advice
stop smoking advice
CKD care plan
Can only be ascertained by patient reported outcomes
Immunisation 1
Uncoded – CKD3-5
+
Coded- CKD3-5
=
Confirmed CKD3-5
Influenza
immunisation in
last 12 months
Flu immunised
Immunisation 2
Hep immune
pos
Uncoded – CKD4-5
+
Coded- CKD4-5
=
Confirmed CKD4-5
Hepatitis
HsAb in last 5
years
neg
Hepatitis B
immunisatio
n in last 5
years
yes
Hep immunised
unknown
Hep unknown
Hep non-immunised
n.b. this will depend on local practice – will need survey results to interpret these data
Immunisation 3
Uncoded – CKD4-5
+
Coded- CKD4-5
=
Confirmed CKD4-5
Pneumococus
immunisation
in last 5 years
yes
Pneumo non-immunised
Pneumo immunised
Hb monitoring
Uncoded – CKD3b-5
+
Coded- CKD3b-5
=
Confirmed CKD3b-5
Hb sample sent in
last 12 months
Hb monitored
BMD
Uncoded – CKD4-5
+
Coded- CKD4-5
=
Confirmed CKD4-5
Bone metabolism
(Ca/PO4/PTH/vit D
level) checked in
last 12 months
Collect:
Vitamin D preparations (long list)
alphacalcidol
ergocalciferol
calcium tablets + variants
sevalemer
lanthanum
aluminium hydroxide
calcium acetate
‘dulwich mixture’/magnesium+calcium
BMD monitored
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
The percentage of people with CKD who are assessed for kidney disease progression and related problems according to their disease stage [*, QS6]
Based on eGFR/urine laboratory results/timing. For CKD 3B percentage that had Hb measured.
The percentage of people with defined indicators for referral who were referred to secondary care [*, QS2] within 3 months of abnormal results
eGFR/urine results and timing, high blood pressure despite 4 antihypertensive drug classes, read-codes for referral and/or renal ultrasound, pop-up
box for GPs to fill in if phone or e-mail advice from specialistswas given
The percentage of people with CKD who are assessed for cardiovascular risk [*, QS4]
Management
The percentage of people with CKD who have a current agreed care plan [QS3] by 1 year
read-code on whether patients were informed about their diagnosis (once available), see 4.3.
The percentage of people with CKD who have blood pressures in the NICE recommended target range by 1 year [*, QS5]
Includes proportion of patients on renin-angiotensin blocking drugs according to proteinuria status
The percentage of people with CKD who are treated with statins according to their cardiovascular risk by 1 year [*]
Primary and secondary prevention as per updated NICE lipid guideline (once available)
The percentage of people with CKD who had their medication reviewed whilst acutely unwell
The percentage of people with CKD who were vaccinated for influenza (NICE TA158)
For CKD stages 4 &5 this would also apply to pneumococcal virus and Hepatitis B if seronegative (KDIGO CKD guideline 2013).
The percentage of people with CKD 4&5 who have phosphate and haemoglobin measurements on GP laboratory systems. [*] #