20140423imeglimin - 埼玉医科大学総合医療センター 内分泌
advertisement
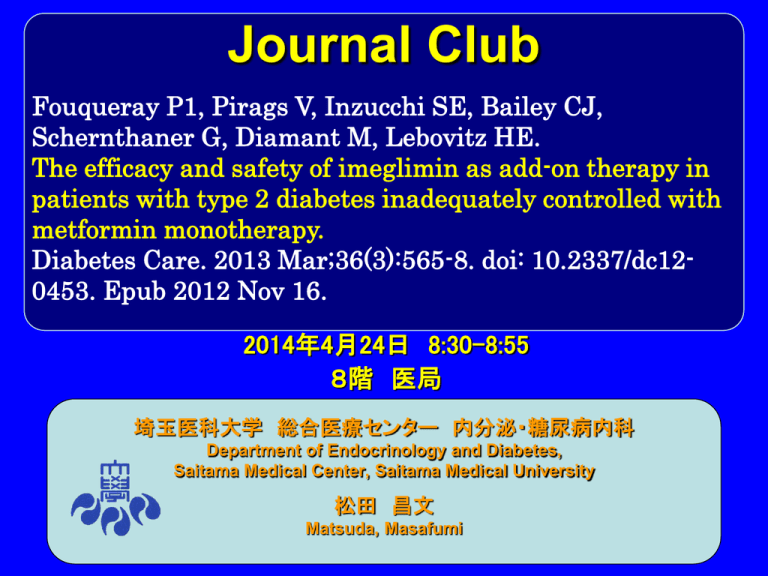
Journal Club Fouqueray P1, Pirags V, Inzucchi SE, Bailey CJ, Schernthaner G, Diamant M, Lebovitz HE. The efficacy and safety of imeglimin as add-on therapy in patients with type 2 diabetes inadequately controlled with metformin monotherapy. Diabetes Care. 2013 Mar;36(3):565-8. doi: 10.2337/dc120453. Epub 2012 Nov 16. 2014年4月24日 8:30-8:55 8階 医局 埼玉医科大学 総合医療センター 内分泌・糖尿病内科 Department of Endocrinology and Diabetes, Saitama Medical Center, Saitama Medical University 松田 昌文 Matsuda, Masafumi Imeglimin ((6R)-(+)-4-dimethylamino- 2-imino-6methyl-1,2,5,6tetrahydro- 1,3,5, triazine hydrochloride) is the first in a new tetrahydrotriazine-containing class of oral antidiabetic agents, the glimins. It is an oxidative phosphorylation blocker that acts to inhibit hepatic gluconeogenesis, increase muscle glucose uptake, and restore normal insulin secretion. 1Poxel SA, Lyon, France 2Paul Stradins Clinical University Hospital, Riga, Latvia 3VU University Medical Center, Amsterdam, the Netherlands 4Rudolfstiftung Hospital, Vienna, Austria 5State University of New York, Health Sciences Center, Brooklyn, NY 6Yale School of Medicine, New Haven, CT 7Aston University, Birmingham, U.K. OBJECTIVE This 12-week study assessed the efficacy and tolerability of imeglimin as add-on therapy to the dipeptidyl peptidase-4 inhibitor sitagliptin in patients with type 2 diabetes that was inadequately controlled with sitagliptin monotherapy. RESEARCH DESIGN AND METHODS In a multicenter, randomized, double-blind, placebocontrolled, parallel-group study, imeglimin (1,500 mg b.i.d.) or placebo was added to sitagliptin (100 mg q.d.) over 12 weeks in 170 patients with type 2 diabetes (mean age 56.8 years; BMI 32.2 kg/m2) that was inadequately controlled with sitagliptin alone (A1C ≧7.5%) during a 12-week run-in period. The primary efficacy end point was the change in A1C from baseline versus placebo; secondary end points included corresponding changes in fasting plasma glucose (FPG) levels, stratification by baseline A1C, and percentage of A1C responders. Supplementary Figure 1. Summary of subject disposition Abbreviations: ITT = Intention-to-treat; PP = Per-protocol Figure 2—A: Effect of sitagliptin-imeglimin vs. sitagliptin-placebo: A1C reductions over the 12- week double-blind treatment period. B: Effect of sitagliptin-imeglimin vs. sitagliptin-placebo: change in A1C depending on baseline A1C value. TEAEs: treatment-emergent adverse events RESULTS Imeglimin reduced A1C levels (leastsquares mean difference) from baseline (8.5%) by 0.60% compared with an increase of 0.12% with placebo (betweengroup difference 0.72%, P < 0.001). The corresponding changes in FPG were 20.93 mmol/L with imeglimin vs. 20.11 mmol/L with placebo (P = 0.014). With imeglimin, the A1C level decreased by ‡0.5% in 54.3% of subjects vs. 21.6% with placebo (P < 0.001), and 19.8%of subjects receiving imeglimin achieved a decrease in A1C level of £7% compared with subjects receiving placebo (1.1%) (P = 0.004). Imeglimin was generally well-tolerated, with a safety profile comparable to placebo and no related treatment-emergent adverse events. CONCLUSIONS Imeglimin demonstrated incremental efficacy benefits as add-on therapy to sitagliptin, with comparable tolerability to placebo, highlighting the potential for imeglimin to complement other oral antihyperglycemic therapies. Message Imegliminという物質も糖尿病治療に使えそうと いう論文。 1Poxel SA, Lyon, France 2Department of Internal Medicine, Paul Stradins Clinical University Hospital, Riga, Latvia 3Section of Endocrinology, Yale School of Medicine, New Haven, Connecticut 4School of Life and Health Sciences, Aston University, Birmingham, United Kingdom 5Department of Internal Medicine, Rudolfstiftung Hospital, Vienna, Austria 6Diabetes Center/Department of Internal Medicine, VU University Medical Center, Amsterdam, the Netherlands 7Department of Medicine, State University of New York, Health Sciences Center, Brooklyn, New York Diabetes Care 36:565–568, 201 OBJECTIVE A 12-week study assessed the efficacy and safety of a new oral antidiabetic agent, imeglimin, as add-on therapy in type 2 diabetes patients inadequately controlled with metformin alone. RESEARCH DESIGN AND METHODS A total of 156 patients were randomized 1:1 to receive imeglimin (1,500 mg twice a day) or placebo added to a stable dose of metformin (1,500–2,000 mg/day). Change in A1C from baseline was the primary efficacy outcome; secondary outcomes included fasting plasma glucose (FPG) and proinsulin/insulin ratio. RESULTS After 12 weeks, the placebosubtracted decrease in A1C with metforminimeglimin was −0.44% (P < 0.001). Metformin-imeglimin also significantly improved FPG and the proinsulin/insulin ratio from baseline (−0.91 mg/dL and −7.5, respectively) compared with metforminplacebo (0.36 mg/dL and 11.81). Metforminimeglimin therapy was generally welltolerated with a comparable safety profile to metformin-placebo. CONCLUSIONS Addition of imeglimin to metformin improved glycemic control and offers potential as a new treatment for type 2 diabetes. テトラヒドロトリアジンを含む全く新しいクラスの経口糖尿病 治療薬(glimins) として注目されているものの1つに imegliminがある。同薬に関する2件の概念実証(proofof-concept)試験は終了しており,現在,第Ⅱ相臨床試験 でメトホルミンへのimegliminの上乗せ効果が検証されてい る。同薬を開発しているPoxel社のPascale Fouqueray氏 は「メトホルミン単剤治療でのコントロールが不十分な2型糖 尿病患者にimegliminを上乗せ投与すれば,より良好な血 糖管理が見込め,忍容性にも問題ないことが12週間の第Ⅱ 相ランダム化比較試験(RCT)により示された」とDiabetes Care 2012年11月16日オンライン版で報告した。同薬の作 用機序としては,2型糖尿病の3大病態を改善する可能性が 指摘されている。