The Resident`s Guide to Pain Management
advertisement

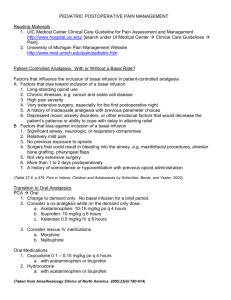
THE RESIDENT’S GUIDE TO PAIN MANAGEMENT AGS Elizabeth Kvale, MD Palliative Medicine THE AMERICAN GERIATRICS SOCIETY Geriatrics Health Professionals. Leading change. Improving care for older adults. PAIN PHYSIOLOGY BASICS: TYPES OF PAIN • Nociceptive — arthritis, fracture, laceration • Visceral — pancreatitis, MI, constipation • Neuropathic — herpes zoster, diabetic neuropathy • Complex regional pain syndromes (RSD) • Central pain Slide 2 PAIN PHYSIOLOGY BASICS: ACUTE VS. CHRONIC PAIN Acute pain • Identified event, resolves in days–weeks • Usually nociceptive Chronic pain • Cause often not easily identified; multifactorial • Indeterminate duration • Nociceptive and/or neuropathic Slide 3 PAIN ASSESSMENT BASICS: BELIEVE THE PATIENT • Pain is a subjective experience ― the patient is the best source of information about their pain • Pain history ― site(s), intensity, temporality, character, exacerbating and alleviating factors Slide 4 PAIN ASSESSMENT BASICS: USE AN ASSESSMENT INSTRUMENT Allows you to know and document whether you have helped the patient Slide 5 PAIN MANAGEMENT BASICS: Match the medication to the amount of the patient’s discomfort 3 Severe 2 Moderate Morphine A/Codeine 1 Mild A/Hydrocodone A/Oxycodone ASA Acetaminophen A/Dihydrocodeine Tramadol NSAIDs ± Adjuvants ± Adjuvants Hydromorphone Methadone Levorphanol Fentanyl Oxycodone ± Adjuvants Slide 6 PAIN MANAGEMENT BASICS • Don’t delay for investigations or disease treatment • Unmanaged pain nervous system changes Permanent damage Amplification of pain • Treat underlying cause (eg, radiation for a neoplasm) Slide 7 PAIN MANAGEMENT BASICS: OPIOID PHARMACOLOGY (1 of 2) • Conjugated in liver • Excreted via kidney (90%–95%) • First-order kinetics • Time to Cmax PO dosing ― 1 hour SC or IM dosing ― 30 minutes IV dosing ― 6 minutes Slide 8 PAIN MANAGEMENT BASICS: OPIOID PHARMACOLOGY (2 of 2) • Steady state after 4–5 half-lives Steady state after 1 day (24 hours) • Duration of effect of “immediate-release” formulations (except methadone) 3–5 hours PO or PR Shorter with parenteral bolus Slide 9 PAIN MANAGEMENT BASICS Oral dosing of immediate-release preparations Codeine, hydrocodone, morphine, hydromorphone, oxycodone • Dose q4h • Adjust dose daily • Mild or moderate pain: ↑ 25%–50% • Severe or uncontrolled pain: ↑ 50%–100% • Adjust more quickly for severe uncontrolled pain Slide 10 PAIN MANAGEMENT BASICS Oral dosing of extended-release preparations • Improve compliance, adherence • Dose q8h, q12h, or q24h (product-specific) Don’t crush or chew tablets May flush time-release granules down feeding tubes • Adjust dose q2–4 days (once steady state reached) Slide 11 PAIN MANAGEMENT BASICS Breakthrough pain • Use immediate-release opioids 5%–15% of 24-h dose Offer after Cmax reached • PO or PR: ~ q1h • SC or IM: ~ q30min • IV: ~ q10–15min • Do not use extended-release opioids Slide 12 PAIN MANAGEMENT BASICS • Ongoing assessment • Increase analgesics until pain is relieved or adverse effects are unacceptable • Be prepared for sudden changes in pain • Driving is safe if pain is controlled, dose is stable, no adverse effects Slide 13 CONCERNS ABOUT OPIOID USE: POOR RESPONSE If dose escalation adverse effects: • Use more sophisticated therapy to counteract adverse effect • Use an alternative: Route of administration Opioid (“opioid rotation”) • Use a co-analgesic • Use a nonpharmacologic approach Slide 14 CONCERNS ABOUT OPIOID USE: CLEARANCE • Conjugated in liver • 90%–95% excreted in urine • If dehydration, renal failure, severe hepatic failure develops: dosing interval, dosage size • If oliguria or anuria develops: Stop routine dosing of morphine Use only PRN Slide 15 CONCERNS ABOUT OPIOID USE: TOLERANCE • Reduced effectiveness to a given dose over time • Not clinically significant with chronic dosing • If dose requirement is increasing, suspect disease progression Slide 16 CONCERNS ABOUT OPIOID USE: ADDICTION • Psychological dependence • Compulsive use • Loss of control over drugs • Loss of interest in pleasurable activities Slide 17 CONCERNS ABOUT OPIOID USE: PHYSICAL DEPENDENCE • A process of neuroadaptation • Abrupt withdrawal may abstinence syndrome • If dose reduction required, reduce by 50% q2–3 days Avoid antagonists Slide 18 CONCERNS ABOUT OPIOID USE: SUBSTANCE ABUSERS • Can have pain too • Treat with compassion • Protocols, contracting • Consult with pain or addiction specialists Slide 19 CONCERNS ABOUT OPIOID USE: THINGS TO AVOID • Meperidine — accumulates toxic metabolite normeperidine • Mixed agonists/antagonists – Nubain, Talwin • Do not use naloxone (Narcan) unless true respiratory crisis (RR < 6) Slide 20 SUMMARY: BASIC PRINCIPLES OF PAIN MANAGEMENT • Ask the patient Palliative medicine corollary ― believe the patient • Match the pain medicine to patient’s level of pain • Increase pain medicine (with awareness of Cmax and half-life) until patient is comfortable Slide 21 MRS PAINE • Very pleasant 68-year-old admitted with COPD exacerbation • Home meds include 2 tablets of oxycodone 5 mg/APAP “whenever my back acts up” — usually 4 tablets a day • Appropriate pain medication order? Slide 22 MRS PAINE • Readmitted months later with stage IV nonsmall cell lung cancer • Taking 2 oxycodone/APAP tabs every 6 hours • Rates her pain as 7/10 “most of the time” Slide 23 KEY POINTS • Maximum acetaminophen dose in 24 hours is 4 grams Tylenol #3 (codeine 30 mg/APAP 325 mg) 24-hr maximum = 12 tablets Percocet (oxycodone 5 mg/APAP 325 mg) 24-hr maximum = 12 tablets Tylox (oxycodone 5 mg/APAP 500 mg) 24-hr maximum = 8 tablets Lortab 5 (hydrocodone 5 mg/APAP 500 mg) 24-hr maximum = 8 tablets • How long does it take to get a PRN dose of pain medication once it is requested? Slide 24 KEY POINTS • Mrs Paine’s total daily oxycodone dose is 40 mg (8 tablets 5 mg) Slide 25 THANK YOU FOR YOUR TIME! Visit us at: www.americangeriatrics.org Facebook.com/AmericanGeriatricsSociety Twitter.com/AmerGeriatrics linkedin.com/company/american-geriatricssociety Slide 26