Chase-Lindsay-ppt2014
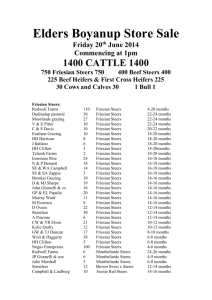
advertisement
Gastric and Esophageal Diverticulum Rupture in a Friesian Gelding LINDSAY CHASE M A Y 7 TH 2 0 1 4 CLINICAL ADVISOR: DR. KATHLEEN MULLEN BASIC SCIENCE ADVISOR: DR. ELIZABETH BUCKLES http://tinyurl.com/k4balp7 Signalment and History 17 year old Friesian Gelding 1 day history of inappetence and lethargy Approximately 8 hour history of colic and dyspnea rDVM Findings Tachycardic (80 bpm) Dyspneic Febrile (102.60F) Muddy mucous membranes – CRT 3 seconds Absent GI motility Normal rectal palpation rDVM Therapy Flunixin meglumine, detomidine, ceftiofur crystalline free acid Nasogastric tube No gastric reflux Instilled water and mineral oil Horse became uncomfortable during administration Referred to Cornell for suspected colitis Physical Exam Vital Signs: T:101.7oF (99-101.5oF) P: 86 bpm (28-44 bpm) R: 52 bpm (8-16 bpm) Depressed BCS 7/9 Small amount of malodorous nasal discharge Cardiovascular Injected mucous membranes with a toxic line CRT 3 seconds Gastrointestinal Absent gut sounds in all quadrants Diagnostics Blood work PCV: 62% (34-46) TP: 6.3 g/dL (6.2-7.8) Hypochloremic metabolic alkalosis Cl 92 (100-110 mEq/L) pH 7.523 (7.32-7.44) BE 8 HCO3 31 (25-30 mmol/L) Ionized Hypocalcemia Hyperlactatemia Elevated Creatinine Elevated Troponin Neutropenia Lymphopenia 1.19 4.8 2.6 0.68 2.0 1.o (1.25-1.78 mg/dL) (0.3-1.5 mmol/L) (0.4-2.2 mg/dL) (0-0.06 ng/mL) (3.0-7.0 thou/uL) (1.8-5.0 thou/uL) Additional Diagnostics Thoracic Ultrasound No pleural fluid or evidence of pleuritis Abdominal Ultrasound Stomach of normal size Thickened large colon and small intestinal walls Imaging was difficult because of BCS No appreciable peritoneal fluid Rectal Exam Thickened but compressible loops of small intestine Nasogastric Intubation Unable to pass tube beyond the cardia Problem List Colic Thickened SI and colon Inability to pass NG tube into stomach Tachypnea Endotoxemia Dehydration Hypoproteinemia Hypochloremic metabolic alkalosis Hypocalcemia Hyperlactatemia Leukopenia http://pad2.whstatic.com/images/b/ba/ Sickhorse.jpg Differential Diagnoses for Colic Colic NonGastrointestinal Gastrointestinal Proximal GI Gastric Impaction, Gastric Ulcers, Gastric Rupture, Choke, Esophageal Rupture Small Intestine Strangulating Non-Strangulating Lipomas, Rents/Hernias Enteritis, IBD, Ileal Impaction Large Intestine Other Genitourinary Musculoskeletal Large colon volvulus, Colitis, Displacements, Impactions, Cecal Disease, Enteroliths Pleuropneumonia, Hepatopathy, Neuropathy Urinary Calculi, Uterine Artery Rupture Rhabdomyolysis, Laminitis Initial Stabilization and Treatment 1L Hypertonic saline bolus 20L Plasmalyte bolus Plasmalyte CRI with electrolyte supplementation Hetastarch CRI Lidocaine CRI Antiendotoxic dose of flunixin (0.25 mg/kg) Cryotherapy Offered 3L of water – after drinking became uncomfortable Photo courtesy of Dr. Sally Ness Re-evaluation No clinical improvement Thoracic ultrasound Pleural fluid Abdominal ultrasound Copious amounts of flocculant peritoneal fluid Upper GI Endoscopy Photo courtesy of Dr. Sally Ness Impaction of feed material in distal esophagus Abdominocentesis Septic peritonitis consistent with GI rupture Euthanasia was elected and a necropsy was performed Photo courtesy of Dr. Katie Mullen Gross Findings Photo courtesy of Dr. Kim Bonner Peritoneal cavity contained ~60 L of peritoneal effusion with copious amounts of fibrin. No feed material was found in the fluid. Gross Findings Photos courtesy of Dr. Kim Bonner Left: 8 cm tear in impacted esophageal pulsion diverticulum caudal to the diaphragm Right: Severe smooth muscle hypertrophy of caudal esophageal wall (1.7 cm (normal thickness 0.5 +- 0.1 cm)) Esophageal Diverticula Types of Diverticula Traction Shallow body and wide opening Usually secondary to esophageal injury Able to transmit peristalsis Not prone to impaction Pulsion Flask-like body and narrow opening Mucosa protrudes through a defect in esophageal wall Prone to impaction Usually located in cervical region in the horse Gross Findings Photos courtesy of Dr. Kim Bonner Left: Full thickness gastric tear (5.5 cm) located within a 10 cm partial tear (separation of tunica muscularis) along the lesser curvature Right: Severe edema in pyloric gastric wall Regional Anatomy 1. 2. 3 1 3. 4. 2 5. 4 6. 5 6 Color Atlas of Veterinary Anatomy, Volume 2, The Horse. Vol. 2: Elsevier Health Sciences, 2012. 160. Print. Esophagus Stomach Diaphragm Liver Left Dorsal Colon Left Ventral Colon Histopathology Distal Esophagus Thickened tunica muscularis No underlying condition was found that would have predisposed to either the gastric or esophageal lesions Photo courtesy of Dr. Elizabeth Buckles History of the Breed 1500-1600 - Developed in the Friesland province of the Netherlands 1879 – Studbook was founded 1913 – Only 3 approved stallions 1928 – 8 approved stallions bred 358 mares Currently 45,000 registered Friesians http://tinyurl.com/lcyvxcl http://tinyurl.com/ophacvb Common Anomalies and Diseases Dwarfism Hydrocephalus Retained placenta Chronic Proliferating Lymphangitis Megaesophagus Aortic rupture Aortopulmonary fistulas All photographs: Boerma, S., W. Back, and M. M. Sloet Van OldruitenborghOosterbaan. "The Friesian Horse Breed: A Clinical Challenge to the Equine Veterinarian?" Equine Veterinary Education 24.2 (2012): 66-71. Web. Current Research Retrospective study conducted in 2013 852 horse necropsies over 6 years at Michigan State University 42 horses had gross esophageal lesions, 10 were severe 35.3% of Friesians submitted had severe esophageal lesions compared to 0.5% of other breeds Most common lesion was caudal esophageal smooth muscle hypertropy Prevalence in Friesians: 35% and all other breeds <3% Usually an incidental idiopathic finding in older horses Megaesophagus was present in 6 Friesian horses, 5/6 had severe muscular hypertrophy Current Research Aortic Rupture Study published in April 2014 showed specific histological changes Accumulation of mucoid material Disorganization and fragmentation of elastic laminae Smooth muscle hypertrophy Medial necrosis Hypothesized to be a genetic connective tissue disorder of elastin or collagen Dwarfism Tendons of dwarf Friesians and non-dwarf Friesians have been shown to have more elastic properties compared to control ponies Fenway Foundation for Friesian Horses Mission Statement “The Fenway Foundation for Friesian Horses is a not for profit corporation created to preserve and enhance the longevity and quality of life of Friesian horses by accruing pertinent equine, more specifically Friesian, information to educate the public and offering assistance regarding Friesian horses and their owners throughout North America.” Services Rescue assistance Necropsy assistance Health assistance Genetic assistance http://www.fenwayfoundation.com/index.html Educational assistance Continuing Care Assistance Upon Incapacitation Or Death Necropsy Assistance The foundation will reimburse for necropsies on Friesians 17 years old and younger Work in conjunction with Dr. Back at Utrecht University on the following: Hydrocephalus Dwarfism Aortic rupture Megaesophagus Detailed necropsy guidelines and sample information found at: http://www.fenwayfoundation.com/services.html Final Cost Emergency Colic Work-up $768 Medications, Fluids and Supplies $852.23 Diagnostics $393.19 Necropsy $214.40 http://www.kimballstock.com/pix/HOR/01/HOR_01_MB0134_01_P. JPG Total: $2227.82 - Reimbursement from Fenway Foundation References Benders, N. A., J. B. Veldhuis Kroeze, and J. H. Van Der Kolk. "Idiopathic Muscular Hypertrophy of the Oesophagus in the Horse: A Retrospective Study of 31 Cases." Equine Veterinary Journal 36.1 (2004): 46-50. Web. Boerma, S., W. Back, and M. M. Sloet Van Oldruitenborgh-Oosterbaan. "The Friesian Horse Breed: A Clinical Challenge to the Equine Veterinarian?" Equine Veterinary Education 24.2 (2012): 66-71. Web. Fenway Foundation for Friesian Horses. N.p., n.d. Web. <http://www.fenwayfoundation.com/index.html>. "Friesian Timeline." Friesian Horse Association of North America. N.p., 2014. Web. 01 May 2014. <http://www.fhana.com/timeline/>. Komine, M., I. M. Langohr, and M. Kiupel. "Megaesophagus in Friesian Horses Associated With Muscular Hypertrophy of the Caudal Esophagus." Veterinary Pathology Online (2013): n. pag. Sage Publications. Web. 1 Apr. 2014. <http://vet.sagepub.com/content/early/2013/11/13/0300985813511126>. Ploeg, M., V. Saey, C. Delesalle, et. al. "Thoracic Aortic Rupture and Aortopulmonary Fistulation in the Friesian Horse: Histomorphologic Characterization." Veterinary Pathology Online (2014): n. pag. Sage Publications. Web. 25 Apr. 2014. <http://vet.sagepub.com/content/early/2014/04/16/0300985814528219>. Yamout, S. Z., K. G. Magdesian, and D. A. Tokarz. "Intrathoracic Pulsion Diverticulum in a Horse." Canadian Veterinary Journal 53 (2012): 408-11. Web. Questions? Thank you to: My advisors Dr. Buckles Dr. Mullen Class of 2014! http://animals.desktopnexus.com/wallpaper/533523/