Kevin Pham
May 2014
Objective
T o review the management of acute pulmonary
embolism.
Case
A 48-year-old woman is brought to the emergency room
complaining of a sudden onset of dyspnea. She reports she
was standing in the kitchen making dinner, when she
suddenly felt as if she could not get enough air, her heart
started racing, and she became lightheaded and felt as if
she would faint.
On examination, she is tachypneic with a respiratory rate of
28 breaths per minute, oxygen saturations 84% on room
air, heart rate 124 bpm, and blood pressure 118/89 mm Hg.
She appears uncomfortable, diaphoretic, and frightened.
Her right leg is moderately swollen from mid-thigh to her
feet, and her thigh and calf are mildly tender to palpation.
Her chest x-ray is interpreted as normal.
Access Medicine
Case
The CT and V/Q scan are broken. What is the next
best step?
A. Treat empirically with anticoagulation if you cannot
obtain a definitive work up for pulmonary embolism
within 4 hours.
B. Treat empirically with anticoagulation now.
C. Treat empirically with anticoagulation if you cannot
get a definitive work up for pulmonary embolism within
24 hours.
D. Do not treat empirically
Introduction
Mortality without treatment: 30%
Mortality with effective treatment: 3-8%
Most deaths are due to recurrent pulmonary embolism
(PE) within the first few hours of the initial event.
Initial Resuscitation
Hypoxia: routine management.
Hypotension: routine management with IVF.
Be cautious in patients with RV failure.
Vasopressors: Levophed is usually first line. Others can
be considered depending on clinical scenario.
Dobutamine can cause hypotension at low doses since
vasodilation>inotropic effects. Consider concurrent use with
Levophed until higher dose of dobutamine is obtained.
Empiric Anticoagulation
UpToDate
Risk of Bleeding
Empiric anticoagulation therapy
should be considered on a caseby-case basis for patient with
moderate or high risk for
bleeding.
1 risk factor (moderate):3.2
percent risk of bleeding in the
first three months and 1.6 percent
per year thereafter
2 risk factors (high): 12.8 percent
in the first three months and ≥6.5
percent per year thereafter
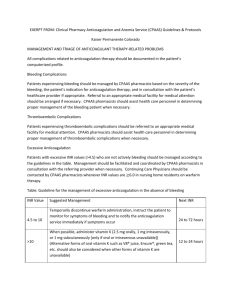
Risk Factors for bleeding
Age >65
Previous bleeding
Thrombocytopenia
Antiplatelet therapy
Recent surgery
Frequent falls
Previous stroke
Diabetes
Anemia
Cancer
Renal failure
Liver failure
Alcohol abuse
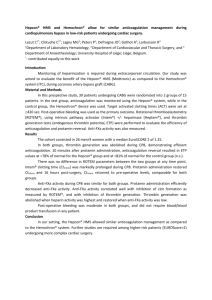
Anticoagulation
Anticoagulation improves mortality in clinical trials
Barritt, DW and Jorder, SC. Anticoagulant drugs in the treatment of pulmonary
embolism. A controlled trial. Lancet. 1960;1(7138):1309.
Initiation of anticoagulation
LMWH is preferred in hemodynamically stable patient.
Subcutaneous fondaparinux is next in line.
UFH is preferred in setting of persistent hypotension,
poor subcutaneous absorption (morbid obesity), modhigh bleeding risk, possible thrombolysis, and renal
failure (Cr eatinine clearance <30)
Anticoagulation
Long-term therapy
Warfarin is recommended due to extensive prior clinical
experience.
Rivaroxaban and other new oral agents can be
considered if warfarin is not an option.
LMWH is preferred in those with active malignancy.
Anticoagulation
Duration
1st episode PE with provoked etiologies (immobility,
surgery, trauma, etc): at least 3 months. (Grade 1B)
1st episode unprovoked with low-mod bleeding risk:
indefinite. (Grade 2B)
1st episode unprovoked with high bleeding risk: at least 3
months. (Grade 1B)
Recurrent with low/mod bleeding risk: indefinite.
(Grade 1A/2B respectively)
Recurrent with high bleeding risk: at least 3 months.
(Grade 2B)
IVC Filter
Indications
Contraindications to anticoagulation
Failed anticoagulation
Developed a complication due to anticoagulation
Severe cardiopulmonary compromise where the next PE
will be lethal
Case
A 48-year-old woman is brought to the emergency room
complaining of a sudden onset of dyspnea. She reports she
was standing in the kitchen making dinner, when she
suddenly felt as if she could not get enough air, her heart
started racing, and she became lightheaded and felt as if
she would faint.
On examination, she is tachypneic with a respiratory rate of
28 breaths per minute, oxygen saturations 84% on room
air, heart rate 124 bpm, and blood pressure 118/89 mm Hg.
She appears uncomfortable, diaphoretic, and frightened.
Her right leg is moderately swollen from mid-thigh to her
feet, and her thigh and calf are mildly tender to palpation.
Her chest x-ray is interpreted as normal.
Access Medicine
Case
The CT and V/Q scan are broken. What is the next
best step?
A. Treat empirically with anticoagulation if you cannot
obtain a definitive work up for pulmonary embolism
within 4 hours.
B. Treat empirically with anticoagulation now.
C. Treat empirically with anticoagulation if you cannot
get a definitive work up for pulmonary embolism within
24 hours.
D. Do not treat empirically
Case
The CT scan was fixed, and CTA chest shows evidence
of pulmonary embolism. What is the best next step?
A. Start subcutaneous LMWH only
B. Start warfarin only
C. Start subcutaneous LMWH and bridge to warfarin
D. Start parenteral unfractionated heparin
E. Start rivaroxaban
Summary
Initial resuscitation is key .
Empiric anticoagulation should be considered when
the diagnosis cannot be a made in a timely manner.
Anticoagulation should be prompted with appropriate
agent(s).
IVF filter should be considered when anticoagulation
is not an option.
References
Kearon, C. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and
Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based
Clinical Practice Guidelines.
Barritt, DW and Jorder, SC. Anticoagulant drugs in the treatment of pulmonary
embolism. A controlled trial. Lancet. 1960;1(7138):1309.
Tapson, VF. Fibrinolytic (thrombolytic) therapy in acute pulmonary embolism and lower
extremity deep vein thrombosis. UpToDate.
Tapson, VF. Treatment of acute pulmonary embolism. UpToDate.