SPIROCHETES
Dr.T.V.Rao MD
Dr.T.V.Rao MD
1
Spirochetes
Spirochetes -are elongated motile,
flexible bacteria twisted spirally along the
long axis are termed spirochetes
Contain – endoflegalla which are polar
flagella wound along the helical
protoplasmic cylinder and situated
between the outer membrane and cell
wall
Dr.T.V.Rao MD
2
Taxonomy
Order: Spirochaetales
Family: Spirochaetaceae
Genus: Trepanoma
Borrelia
Family: Leptospiraceae
Genus: Leptospira
Dr.T.V.Rao MD
3
Human pathogen
A. Genera Trepanoma
B.
C.
Borreilia
Leptospira
Dr.T.V.Rao MD
4
How they appear
Dr.T.V.Rao MD
5
What are Trepanoma
Trepos – Turn
Nema Meaning thread
Relatively short and slender
With fine spirals pointed and round
ends
May be pathogenic or commensals in
the mouth
Dr.T.V.Rao MD
6
Spirochaetales Associated
Human Diseases
Genus
Species
Disease
Treponema pallidum ssp. pallidum
pallidum ssp. endemicum
pallidum ssp. pertenue
carateum
Syphilis
Bejel
Yaws
Pinta
Borrelia
burgdorferi
recurrentis
Many species
Lyme disease (borreliosis)
Epidemic relapsing fever
Endemic relapsing fever
Leptospira
interrogans
Leptospirosis
(Weil’s Disease)
Dr.T.V.Rao MD
7
Venereal Syphilis
Venereal Syphilis caused by
T.pallidum Endemic syphilis
T. pallidum
Yaws T.pertune
Pinta T.carateum
Dr.T.V.Rao MD
8
Discovery
“Everything” happened mostly
in Germany from 1905 to 1910 !
With a short life of 35 years,
Fritz Schaudinn (1871-1906) and
Paul E. Hoffmann (1868-1959)
discovered Treponema pallidum
in serum in 1905.
Paul Ehrlich,
father of
immunochemistry
and his assistent Hati.
Fritz
Dr.T.V.Rao MD
Schaudinn
9
Syphilis
A. Named from poem
published by the
Italian physician
and poet Girolamo
Fracastoro –
shepherd from
Hispaniola named
Syphilis who angered
Apollo and was given
the disease as
punishment
Dr.T.V.Rao MD
10
Syphilis
"He who knows
syphilis,
knows
medicine"
Sir William Osler
Dr.T.V.Rao MD
11
Treponema pallidum
A. Described in
1905 by
Schaudinn
and
Hoffman,
Hamburg
Dr.T.V.Rao MD
12
Trepanoma pallidum
Greek words trepo “turning” & nema “head”
A.
Morphology
1.
2.
Motile, sluggish in viscous environments
Size: 5 to 20 μm in length & 0.09 to 0.5 μm in
diameter, with tapered ends
Structure
3.
•
•
•
•
•
Multilayer cytoplasmic membrane
Flagella-like fibrils
Cell wall
Outer sheath (outer cell envelope)
Capsule-like outer coat
Dr.T.V.Rao MD
13
Treponema pallidum.
A.
Spiral spirochete that is
mobile of spirals varies
from 4 to 14 Length 5 to
20 microns and very thin
0.1 to o.5 microns. Can
be seen on fresh
primary or secondary
lesions by dark field
microscopy or
fluorescent antibody
techniques
Dr.T.V.Rao MD
14
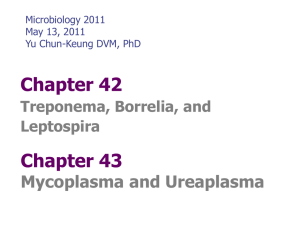
General Overview of
Spirochaetales
A. Gram-negative spirochetes
B. Spirochete from Greek for “coiled
hair”
C. Extremely thin and can be very long
D. Tightly coiled helical cells with
tapered ends
E. Motile by Periplasmic flagella (a.k.a.,
axial fibrils or endoflegalla)
Dr.T.V.Rao MD
15
General Overview of
Spirochaetales
A. Outer sheath encloses axial fibrils wrapped
around
protoplasmic cylinder
B. Axial fibrils originate from insertion pores at
both poles of cell
C. May overlap at centre of cell in Treponema
and Borrelia, but not in Leptospira
D. Differing numbers of endoflegalla according
to genus & species
Dr.T.V.Rao MD
16
Trepanoma palladium
B. Physiology
– Difficult to culture
• Maintained in anaerobic
medium with albumin, sodium
bicarbonate, pyruvate,
cysteine
• Microaerophilic
Dr.T.V.Rao MD
17
Cross-Section
of Spirochete
with
Periplasmic
Flagella
Cross section of
Borrelia burgdorferi
NOTE: a.k.a.,
endoflegalla,
axial fibrils or
axial filaments.
(Outer sheath)
Dr.T.V.Rao MD
18
Staining with special stains
Staining by
Giemsa
and
Fontana
Dr.T.V.Rao MD
19
Antigenic structure
A. The Antigens are complex
B. Infection with Treponema will induce 3
types of Antigens
C. Reagin Antibodies – STS
D. Detected by Standard tests for
Syphilis
E. 1 Wasserman Test, 2 Kahn Test
F. VDRL Test Dr.T.V.Rao MD
20
Beef Heart Extracts Antigen
Lipid Hapten – Cardiolipin
Chemically Dipphostidyl glycerol
Cardiolipin present in the
Trenonems ?
Or a product of tissue Damage ?
Dr.T.V.Rao MD
21
Second Group Antigen
T.pallidum
A.Present in T.pallidum
and Non pathogenic
cultivable treponemes
B.Reiter's Trenonems
Dr.T.V.Rao MD
22
Third Antigen
Polysaccharide
species specific
Positive only in
sera of patients
infected with
pathogenic
Treponema
Dr.T.V.Rao MD
23
Dark field Microscopy
Dr.T.V.Rao MD
24
Treponema cannot be cultivated
in Culture Media
A.
The inability to grow
most pathogenic
Treponema in vitro,
coupled with the
transitory nature of
many of the lesions,
makes diagnosis of
Treponema infection
impossible by routine
bacteriological
methods
Dr.T.V.Rao MD
25
Cultivation of .. ?
A.
Although the Treponemes
are distantly related to
Gram-negative bacteria,
they do not stain by
Gram's method, and
modified staining
procedures are used.
Moreover, the pathogenic
Treponemes cannot be
cultivated in laboratory
media and are
maintained by
subculture in
susceptible animals.
Dr.T.V.Rao MD
26
Trepanoma pallidum
D. Clinical Infection: Syphilis
1.
Transmission
•
2.
Usually through sexual contact from an infected
individual by invading intact mucous membranes or
abraded skin
Pathogenesis
•
•
•
•
Disease of blood vessel & perivascular areas
Primary lesion due to inflammation at site of
inoculation
Secondary lesion due to inflammation of ectodermal
tissues
Tertiary lesion due to diffuse chronic inflammation to
organ systems
Dr.T.V.Rao MD
27
Trepanoma pallidum
D. Clinical Infection: Syphilis
3.
Clinical Manifestations
i. Primary Disease
•
•
•
Chancre: single lesion, non-tender &
firm with a clean surface, raised border
& reddish color
Usually on the cervix, vaginal wall, anal
canal
Draining lymph nodes enlarged & nontender
Dr.T.V.Rao MD
28
Pathogenesis of T. pallidum
Tissue destruction and lesions are primarily a
consequence of patient’s immune response
Syphilis is a disease of blood vessels and of the
perivascular areas
In spite of a vigorous host immune response the
organisms are capable of persisting for decades
• Infection is neither fully controlled nor eradicated
• In early stages, there is an inhibition of cell-mediated
immunity
• Inhibition of CMI abates in late stages of disease, hence
late lesions tend to be localized
Dr.T.V.Rao MD
29
Pathology
Penetration:
1. T. pallidum enters the body via skin and
mucous membranes through abrasions
during sexual contact
2. Also transmitted transplacentally
A. Dissemination:
1. Travels via the lymphatic system to regional
lymph nodes and then throughout the body
via the blood stream
2. Invasion of the CNS can occur during any
stage of syphilis
Dr.T.V.Rao MD
30
Pathology
A. The bacteria rapidly enter the
lymphatic's, are widely disseminated
via the bloodstream and may lodge in
any organ. The exact infectious dose
for man is not known, but in
experimental animals fewer than ten
organisms are sufficient to initiate
infection.
Dr.T.V.Rao MD
31
Pathology
The bacteria
multiply at the initial
entry site forming a
chancre, a lesion
characteristic of
primary syphilis,
after an average
incubation period of
3 weeks
Dr.T.V.Rao MD
32
STAGES OF SYPHILIS
1. Primary
2. Secondary
3. Latent
i. Early latent
ii. Late latent
4. Late or tertiary
i. May involve any organ, but main parts are:
• Neurosyphilis
• Cardiovascular syphilis
• Late benign (gumma)
Dr.T.V.Rao MD
33
Basic lesion of syphilis
The chancre is
painless and most
frequently on the
external genitalia,
but it may occur on
the cervix, perianal
area, in the mouth
or anal canal.
Dr.T.V.Rao MD
34
Stages of syphilis
A.
Untreated syphilis
may be a progressive
disease with primary,
secondary, latent and
tertiary stages. T.
pallidum enters
tissues by
penetration of intact
mucosae or through
abraded skin.
Dr.T.V.Rao MD
35
Primary syphilis
One or more painless chancres
(indurated raise edges & clear bases)
that erupt in the genitalia, anus,
nipples, tonsils or eyelids.
b) Starts as papule and then erode
c) Disappear after three to six weeks
even without treatment.
d) Lymphadenopathy that is either
unilateral or bilateral
a)
Dr.T.V.Rao MD
36
Trepanoma pallidum
D. Clinical Infection: Syphilis
3. Clinical Manifestations
iii. Latent disease
a. Early latent (1st 4 years)
• No signs & symptoms of active
syphilis but remain seroactive
b. Late latent (after 4 years)
• If untreated, 60% continue to be
asymptomatic while 40% progress to
tertiaryDr.T.V.Rao
stageMD
37
Pathology
A.
The chancre is
painless and most
frequently on the
external genitalia, but
it may occur on the
cervix, peri-anal area,
in the mouth or anal
canal. Chancres
usually occur singly,
but in
immunocompromised
individuals,
Dr.T.V.Rao MD
38
Chancre
A. The chancre usually heals spontaneously
within 3-6 weeks, and 2-12 weeks later the
symptoms of secondary syphilis
develop. These are highly variable and
widespread but most commonly involve the
skin where macular or pustular lesions
develop, particularly on the trunk and
extremities. The lesions of secondary
syphilis are highly infectious.
Dr.T.V.Rao MD
39
Progress of Disease
A. Relapse of the lesions of secondary
syphilis is common, and latent syphilis
is classified as early (high likelihood of
relapse) or late (recurrence unlikely).
Individuals with late latent syphilis are
not generally considered infectious,
but may still transmit infection to the
fetus during pregnancy and their blood
may remain infectious.
Dr.T.V.Rao MD
40
Trepanoma pallidum
D. Clinical Infection: Syphilis
3. Clinical Manifestations
i.
Primary Disease
•
•
•
Chancre: single lesion, non-tender & firm
with a clean surface, raised border &
reddish color
Usually on the cervix, vaginal wall, anal
canal
Draining lymph nodes enlarged & nontender
Dr.T.V.Rao MD
41
PRIMARY SYPHILIS
(The Chancre)
A.
B.
C.
D.
E.
F.
G.
H.
Incubation period 9-90 days, usually ~21 days.
Develops at site of contact/inoculation.
Classically: single, painless, clean-based,
indurated ulcer, with firm, raised borders. Atypical
presentations may occur.
Mostly anogenital, but may occur at any site
(tongue, pharynx, lips, fingers, nipples, etc...)
Non-tender regional adenopathy
Very infectious.
May be darkfield positive but serologically
negative.
Untreated, heals in several weeks, leaving a faint scar.
Dr.T.V.Rao MD
42
Primary Syphilis
Dr.T.V.Rao MD
43
Clinical Manifestations
Primary Syphilis- Penile
Chancre
Dr.T.V.Rao MD
Source: CDC/ NCHSTP/ Division of STD Prevention, STD Clinical Slides
44
Primary Syphilis
Dr.T.V.Rao MD
45
Primary Syphilis - Chancre
Dr.T.V.Rao MD
46
Primary Syphilis - Chancre
Dr.T.V.Rao MD
47
Pathogenesis of T. pallidum (cont.)
Secondary Syphilis
Secondary disease 2-10 weeks after
primary lesion
Widely disseminated
mucocutaneous rash
Secondary lesions of the skin and
mucus membranes are highly
contagious
Generalized immunological response
Dr.T.V.Rao MD
48
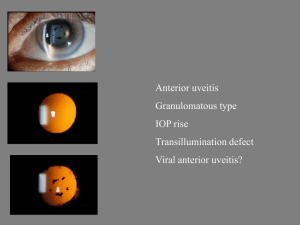
Treponema pallidum
D. Clinical Infection: Syphilis
3.
Clinical Manifestations
iv.
Tertiary Disease
a.
Gummas (3-10 years after secondary disease)
•
Non-progressive, localized dermal lesions
•
Benign tertiary syphilis
•
Pronounced immunologic host reaction
b. Neurosyphilis (>5 years after primary disease)
•
Paralytic dementia, tabes dorsalis, amyotropic
lateral sclerosis, meningovascular syphilis,
seizures, optic atrophy, gummatous changes
Dr.T.V.Rao MD
49
of the cord
Secondary Syphilis
A. Secondary
syphilis at 6-8
weeks – diffuse
symptoms:
1.
2.
3.
Fever
Headache
Skin pustules
B. Usually
disappears
even without
treatment
Dr.T.V.Rao MD
50
Treponema pallidum
D. Clinical Infection: Syphilis
3.
Clinical Manifestations
v. Congenital Syphilis
a.
b.
c.
Transplacental infection of the developing fetus
Abortion occurs during 2nd trimester of pregnancy
Early symptoms:
•
Hepatosplenomegaly, jaundice, hemolytic
anemia, pneumonia, multiple long bone
involvement, snuffles, skin lesions, testicular
masses
Dr.T.V.Rao MD
51
Treponema pallidum
D. Clinical Infection: Syphilis
3.
Clinical Manifestations
v.
Congenital Syphilis
d. Late symptoms:
•
Frontal bossae of Parrott, Short maxilla, high
palatal arch, Hutchinson’s triad (Hutchinson’s
teeth, Interstitial keratitis, eighth-nerve
deafness), saddle nose, mulberry molars,
Higoumenakis sign, relative protruberance of
mandible, rhagades, saber shin, scaphoid
scapulas, Clutton’s joint)
Dr.T.V.Rao MD
52
Secondary Syphilis
Dr.T.V.Rao MD
53
Pathogenesis of T. pallidum (cont.)
Secondary Syphilis
Secondary disease 2-10 weeks after
primary lesion
Widely disseminated
mucocutaneous rash
Secondary lesions of the skin and
mucus membranes are highly
contagious
Generalized immunological response
Dr.T.V.Rao MD
54
Secondary Syphilis
Dr.T.V.Rao MD
55
Secondary Syphilis
Dr.T.V.Rao MD
56
Secondary syphilis
Dr.T.V.Rao MD
57
Tertiary Syphilis
A. Affects 2/3 of untreated cases
1.
2.
3.
4.
5.
6.
Gummata: rubbery tumors
Bone deformities
Blindness
Loss of coordination
Paralysis
Insanity
Dr.T.V.Rao MD
58
Pathogenesis of T. pallidum (cont.)
Latent Stage Syphilis
Following secondary disease, host
enters latent period
•First 4 years = early latent
•Subsequent period = late latent
About 40% of late latent patients
progress to late tertiary syphilitic
disease
Dr.T.V.Rao MD
59
Pathogenesis of T. pallidum (cont.)
Tertiary Syphilis
Tertiary syphilis characterized by
localized granulomatous
dermal lesions (gummas) in
which few organisms are present
• Granulomas reflect containment by
the immunologic reaction of the
host to chronic infection
Dr.T.V.Rao MD
60
Neurosyphilis
A. Late Neurosyphilis develops in about 1/6
untreated cases, usually more than 5 years
after initial infection
B. Central nervous system and spinal cord
involvement
C. Dementia, seizures, wasting, etc.
D. Cardiovascular involvement appears 10-40
years after initial infection with resulting
myocardial insufficiency and death
Dr.T.V.Rao MD
61
Latent Syphilis
A. Latent syphilis
a) Reactive serologic test
b) Asymptomatic until death
A. Late syphilis
Three subtypes of Late syphilis
1. Late, benign syphilis
*Develops between 1 to 10 years after the
infection
*Presence of gumma
Dr.T.V.Rao MD
62
Dr.T.V.Rao MD
63
Mother to Child
Transmission
Infection in utero
may have serious
consequences for
the fetus. Rarely,
syphilis has been
acquired by
transfusion of
infected fresh human
blood.
Dr.T.V.Rao MD
64
Pathogenesis of T. pallidum (cont.)
Congenital Syphilis
Congenital syphilis results from trans
placental infection
T. pallidum septicemia in the developing
fetus and widespread dissemination
Abortion, neonatal mortality, and late
mental or physical problems resulting from
scars from the active disease and progression
of the active disease state
Dr.T.V.Rao MD
65
Treponema pallidum and
Immunity
D. Clinical Infection: Syphilis
4.
Immunity
i.
Syphilis has persistent infection for decades in spite
vigorous host response due to:
•
•
•
ii.
iii.
Dense coat (with fibronectin, transferrin, cerruloplasmin)
Evasion from PMN detection
Inhibition of cell-mediated immunity
Relative but unreliable protection from reinfection in
untreated patients
Minor protection from reinfection in treated patients
Dr.T.V.Rao MD
66
Congenital Syphilis
A. Passed from mother to fetus
during pregnancy
1. Abnormally shaped teeth
2. Nasal septum collapses
3. Skeletal abnormalities
Dr.T.V.Rao MD
67
DIAGNOSIS OF SYPHILIS
A. 1. History and clinical examination.
B. 2. Dark-field microscopy: special
technique use to demonstrate the
spirochete as shiny motile spiral
structures with a dark background.
C. The specimen includes oozing from the
lesion or sometimes L.N. aspirate. It is
usually positive in the primary and
secondary stages and it is most useful in
the primary stage when the serological
tests are still negative.
Dr.T.V.Rao MD
68
Diagnosis of syphilis
A. Direct detection of
spirochetes :
Darkfield microscopy
(motile bugs + experience
+ prompt examination)
Silver stain
A. Culture : not used
B. Serology: non-specific
and specific tests Dr.T.V.Rao MD
69
Serologic Tests
A. Reveal patients immune status not
whether they are currently infected
B. Use lipoidal antigens rather than T.
pallidum or components of it; nontreponemal antigen tests
C. RPR; rapid plasma reagin
D. VDRL; Venereal Disease Research
Laboratory
Dr.T.V.Rao MD
70
Treponema pallidum
F. Laboratory diagnosis
1. Serologic testing
i.
Nontreponemal Tests (uses
Cardiolipin-lecithin as antigen)
a. Complement-fixation tests
(Wasserman & Kolmer test)
b. Flocculation tests (Venereal
Disease Research Laboratory,
(VDRL), Dr.T.V.Rao
Hinton
& rapid reagin tests)71
MD
Serologic Tests
A. Positive within 5 to 6 weeks after
infection
B. Strongly positive in secondary phase
C. Strength of reaction is stated in
dilutions
D. May become negative with treatment
or over decades
Dr.T.V.Rao MD
72
Treponema pallidum
F. Laboratory diagnosis
1. Serologic testing
ii. Treponemal Tests (uses syphilitic
tissue as complement-fixing antigen)
b. Reiter Protein Complement Fixation
• Antigen is an extract from nonvirulent
treponeme (Reiter strain)
• Nonreactive in late stages of syphilis
Dr.T.V.Rao MD
73
Non-treponemal tests
A. Antigen: cardiolipin (beef heart) + lecithin
+ cholesterol
B. Detect nonspecific antibody (Reagin): a
mixture of IgM & IgG direct against some
normal tissue antigens
C. VDRL (Venereal Disease Research
Laboratory) test for serum and CSF
samples
Dr.T.V.Rao MD
74
Venereal Disease Research
Laboratory - VDRL
A.
B.
Flocculation test, antigen consists of very fine particles
that precipitate out in the presence of reagin.
Utilizes an antigen which consists of cardiolipin,
cholesterol and lecithin.
1.
2.
C.
D.
Antigen very technique dependent.
Must be made up fresh daily.
Serum must be heated to 56 C for 30 minutes to
remove anti-complementary activity which may cause
false positive, if serum is not tested within 4 hours
must be reheated for 10 minutes.
Calibrated syringe utilized to dispense antigen must
deliver 60 drops/mL +/- 2drops.
Dr.T.V.Rao MD
75
VDRL
A.
B.
C.
Each preparation of antigen suspension should first be examined
by testing with known positive or negative serum controls.
The antigen particles appear as short rod forms at magnification
of about 100x. Aggregation of these particles into large or small
clumps is interpreted as degrees of positivity
Reactive on left, non-reactive on right
Dr.T.V.Rao MD
76
Rapid Plasma Reagin Test - RPR
A. General screening test, can be adapted to
automation.
B. CANNOT be performed on CSF.
C. Antigen
1.
2.
3.
VDRL cardiolipin antigen is modified with choline
chloride to make it more stable
attached to charcoal particles to allow macroscopic
reading
antigen comes prepared and is very stable.
D. Serum or plasma may be used for testing,
serum is not heated.
Dr.T.V.Rao MD
77
Treponema pallidum
F.
Laboratory diagnosis
1.
Serologic testing
ii.
Treponemal Tests (uses syphilitic tissue as
complement-fixing antigen)
a.
Treponema Pallidum Immobilzation (TPI)
•
Reaginic antibody & complement immobilize a
suspension of living and motile treponemes
maintained in rabbit testes & determined by
darkfield microscopy
•
Difficult, expensive, requires living organisms
•
Positive for nonvenereal treponematoses,
bejels, yaws & pinta
Dr.T.V.Rao MD
78
Treponema pallidum
F. Laboratory diagnosis
1. Serologic testing
ii. Treponemal Tests (uses syphilitic
tissue as complement-fixing antigen)
b. Reiter Protein Complement Fixation
• Antigen is an extract from nonvirulent
treponeme (Reiter strain)
• Nonreactive in late stages of syphilis
Dr.T.V.Rao MD
79
Specific serological tests of
syphilis
A. A. Reiter protein complement fixation
test.
B. B. Fluorescent Treponemal
antibody/absorption test, FTA/ABS.
the most specific and most sensitive .
C. C. Treponema pallidum
haemagglutination test- TPHA- D.
Treponema pallidum immobilization testDr.T.V.Rao MD
80
TPI
Treponema pallidum
haemagglutination (TPHA)
A. Adapted to micro
techniques (MHATP)
B. Tanned sheep
RBCs are coated
with T. pallidum
antigen from
Nichol’s strain.
C. Agglutination of the
RBCs is a positive
result.
Dr.T.V.Rao MD
81
Specific serological tests of
syphilis
A. A. Reiter protein complement fixation
test.
B. B. Fluorescent Treponemal
antibody/absorption test, FTA/ABS.
the most specific and most sensitive .
C. C. Treponema pallidum
Haemagglutination test- TPHA- D.
Treponema pallidum immobilization
Dr.T.V.Rao MD
82
test- TPI
Treponema pallidum
F.
Laboratory diagnosis
1.
Serologic testing
ii.
Treponemal Tests (uses syphilitic tissue as
complement-fixing antigen)
c.
Fluorescent Antibody Tests / Fluorescent Treponemal
Antibody Absorption (FTA-ABS) Test
•
Uses lyophilized Nichols strain organisms as
antigen mixed with antitreponemal antibody
(from test serum) in a slide flourescein
isothiocyanate-labeled antihuman Ig –> presence of
antibody determined by darkfield microscopy
•
Used to diagnosed congenital syphilis & late stage
syphilis, confirmation of nontreponemal tests
Dr.T.V.Rao MD
83
Fluorescent Treponemal Antibody
Absorption Test (FTA-ABS)
A. Diluted, heat inactivated serum added to
Reiter’s strain of T. pallidum to remove
cross reactivity due to other Treponemes.
B. Slides are coated with Nichol’s strain of T.
pallidum and add absorbed patient serum.
C. Slides are washed, and incubated with
antibody bound to a fluorescent tag.
D. After washing the slides are examined for
fluorescence.
E. Requires experienced personnel to read.
F. Highly sensitive Dr.T.V.Rao
and specific,
but
time
MD
84
consuming to perform.
Positive FTA Test for Syphilis Viewed with a
Fluorescent Microscope
Dr.T.V.Rao MD
85
Serologic Tests
A. To improve sensitivity and specificity tests
using a specific treponemal antigen devised
B. MHA-TP: microhemagglutination assay for
T. pallidum
C. FTA-ABS: fluorescent treponemal antibody
absorption test
D. All positive nontreponemal test results
should be confirmed with a specific
treponemal test
Dr.T.V.Rao MD
86
Treponema pallidum
F.
Laboratory diagnosis
1. Serologic testing
ii. Treponemal Tests (uses syphilitic
tissue as complement-fixing
antigen)
d. Haemagglutination Tests
a. Microhemagglutination assay –T.
pallidum (MHA-TP)
Dr.T.V.Rao MD
87
Every Pregnant women Needs
Screening
Dr.T.V.Rao MD
88
Biologic False-Positive
Test Results
A. Positive STS in persons with no
history or clinical evidence of
syphilis
B. Acute BFP: those that revert to
negative in less than 6 months
C. Chronic BFP: persist > 6 months
Dr.T.V.Rao MD
89
BFP Test Results in Syphilis
A.
B.
C.
D.
Acute BFP
Vaccinations
Infections
pregnancy
A. Chronic BFP
B. Connective tissue
disease (SLE)
C. Liver disease
D. Blood transfusions
E. IVDA
Dr.T.V.Rao MD
90
Advantage of VDRL:
• cheap, easy to perform
• quantitative, screen test
• monitor disease course
• trace theraputic effect, become “-” in
6-18 m after effective treatment.
Dr.T.V.Rao MD
91
Treatment of Late Syphilis
A. Late syphilis:
B. benzathine penicillin 2.4 million units
intramuscularly weekly for 3 weeks.
C. procaine penicillin 1.2 million units
intramuscularly daily for 21 days
D. Tetracycline or erythromycin 500 mg 4 times a
day – or doxycycline 100 mg x2- by mouth for
30 days
E. Jarrisch-Herxheimer reaction
F. Follow-up
Dr.T.V.Rao MD
92
Prevention & Treatment of Syphilis
Penicillin remains drug of choice
• WHO monitors treatment recommendations
• 7-10 days continuously for early stage
• At least 21 days continuously beyond the early
stage
Prevention with barrier methods (e.g.,
condoms)
Prophylactic treatment of contacts
identified through epidemiological tracing
Dr.T.V.Rao MD
93
Treponema pallidum
G. Treatment & Prevention
1.
Antibiotic treatment
•
•
2.
DOC: Penicillin (complete recovery for stage
I &II)
streptomycin, tetracycline, erythromycin
(poor passage to fetal circulation)
Treatment of case contacts
3. Barrier methods (condom); “safe
sex”
Dr.T.V.Rao MD
94
Other Related to Treponemes
A. Related
Treponemes cause
the non-venereal
treponematoses
bejel, or endemic
syphilis (T. pallidum
endemicum), yaws
(T. pallidum
pertenue), and pinta
(T. carateum).
Dr.T.V.Rao MD
95
Treponema pallidum
G. Other treponemal diseases
1.
Yaws (Frambesia) -Treponema pertenue
•
•
•
•
•
•
Resembles syphilis
Acquired in childhood other than sexual contact
Mother yaw (or framboise), a painless erythematous
papule occurs a month after primary infection
Secondary lesion resemble primary lesion occurs 1-3
months after
Tertiary lesions involve the skin & bones, crab yaws
DOC: Penicillin
Dr.T.V.Rao MD
96
Treponema pallidum
G. Other treponemal diseases
2.
•
•
•
•
Pinta - Treponema carateum
Acquired by person-to-person contact &
rarely by sexual contact
Primary & secondary lesions are flat,
erythematous & non-ulcerating; healing first
becomes hyper pigmented and later
depigmented scarring; occurs in hand, feet &
scalp
Tertiary lesions are uncommon
DOC: Penicillin
Dr.T.V.Rao MD
97
Treponema pallidum
G. Other treponemal diseases
3. Bejel - Treponema pallidum
variant
•
•
•
•
Endemic syphilis
Acquired by direct contact during
childhood
Similar to syphilis
Dr.T.V.Rao MD
98
DOC: Penicillin
Programme created by
Dr.T.V.Rao MD for Medical and
Health Care Workers in the
Developing World
Email
doctortvrao@gmail.com
Dr.T.V.Rao MD
99