The disease
advertisement

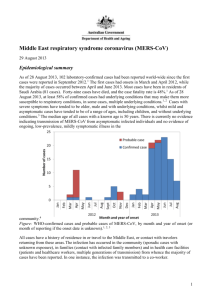
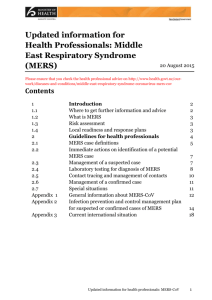
MERS-CoV: the disease Republic of Lebanon Ministry of Public Health Epidemiological Surveillance Program May 2014 Sources • WHO: www.who.int • CDC: www.cdc.gov • ECDC: www.ecdc.europa.eu Outline • • • • • • • Appellation First cases Reservoir Modes of transmission Incubation period Clinical presentation Case management Appellation • Scientific appellation: The Middle East Respiratory Syndrome Coronavirus (MERS-CoV) • By the Coronavirus Study Group of the International Committee on Taxonomy of Viruses • Reference: De Groot RJ, et al. Middle East Respiratory Syndrome Coronavirus (MERS-CoV): Announcement of the Coronavirus Study Group. J Virol. Published ahead of print 15 May 2013. doi:10.1128/JVI.01244-13. Classical coronavirus • Coronaviruses – Large family of viruses that cause a range of illnesses in humans – Viruses also cause a number of animal diseases – In Humans: • Usually: common cold • Rarely, severe diseases as: –Severe Acute Respiratory Syndrome (SARS) –MERS-CoV First cases • On 22 September 2012, the UK informed WHO of a case of acute respiratory syndrome with renal failure with travel history to Saudi Arabia and Qatar. • The case: previously healthy, 49 year-old male, Qatari, with travel history to Saudi Arabia, – On 3 September: presented symptoms – On 7 September: admission to ICU in Doha, Qatar – On 11 September: transfer to UK (by air ambulance). The Health Protection Agency of the UK (HPA) confirmed the presence of a novel coronavirus • The HPA compared the clinical sample with a virus sequenced previously by the Erasmus University Medical Centre, Netherlands: – Isolate obtained from lung tissue of a fatal case earlier this year in a 60 year-old Saudi national – This comparison indicated 99.5% identity, with one nucleotide mismatch over the regions compared. Jordan cluster • On 30 November 2012: two cases from Jordan were added. • The fatal cases occurred in April 2012. At that time, a number of severe pneumonia cases occurred in the country – cluster in hospital setting. • On 24 April 2012: samples had tested negative for known coronaviruses and other respiratory viruses. • In October 2012: stored samples from the cluster of April 2012 were sent by MOH Jordan to NAMRU-3. • In November 2012: NAMRU-3 confirmed two cases of infection with the novel coronavirus. Reservoir • The full picture on the source is not yet clear. – Camels: • Camels are a likely source of infection in humans. • Strains of MERS‐CoV in camels across Africa and the Middle East. • Human and camel genetic sequence data demonstrate a close link between the virus found in camels and that found in people. – Other reservoirs may exist. Modes of transmission Different modes of transmission are occurring Zoonotic transmission from animals, camels, to humans Thus far: primary cases have steadily been reported since April 2013 with recent increase in March and April 2014 Human-to-human transmission: • Very little human-to-human transmission is occurring among family members in household settings • Nosocomial transmission is occurring health care workers and between patients resulting in large health care setting outbreaks Transmission via environmental or fomite contamination Experimental studies of virus persistence on surfaces and at different environmental conditions show that MERS-CoV can be transmitted via contact or fomite Source: WHO Incubation period • Usually 5 days • Range: 2-14 days Source: Hospital Outbreak of Middle East Respiratory SyndromeCoronavirus - n engl j med 369;5 nejm.org august 1, 2013 Symptoms • A typical case of MERS consists of – Acute respiratory infection: • • • • Fever Cough Shortness of breath / Dyspnea Pneumonia is a common finding on examination – Gastrointestinal symptoms: diarrhoea may be reported – Severe illness: • Respiratory failure requiring mechanical ventilation and support in intensive‐care unit. • Organ failure: renal failure, septic shock. – Approximately 27% of patients with MERS have died. – More severe disease is observed in people with weakened immune systems, older people, and those with such chronic diseases as diabetes, cancer, and chronic lung disease. Symptoms Source: Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Abdullah Assiri MD,Jaffar A Al-Tawfiq FACP,Abdullah A AlRabeeah FRCS,Fahad A Al-Rabiah MD,Sami Al-Hajjar MD,Ali Al-Barrak MD,Hesham Flemban MD,Wafa N Al-Nassir MD,Hanan H Balkhy MD,Rafat F Al-Hakeem MD,Hatem Q Makhdoom PhD,Prof Alimuddin I Zumla FRCP,Prof Ziad A Memish FRCP. The Lancet Infectious Diseases - 1 September 2013 ( Vol. 13, Issue 9, Pages 752-761 ). DOI: 10.1016/S1473-3099(13)70204-4 Para-clinical tests Source: Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Abdullah Assiri MD,Jaffar A Al-Tawfiq FACP,Abdullah A AlRabeeah FRCS,Fahad A Al-Rabiah MD,Sami Al-Hajjar MD,Ali Al-Barrak MD,Hesham Flemban MD,Wafa N Al-Nassir MD,Hanan H Balkhy MD,Rafat F Al-Hakeem MD,Hatem Q Makhdoom PhD,Prof Alimuddin I Zumla FRCP,Prof Ziad A Memish FRCP. The Lancet Infectious Diseases - 1 September 2013 ( Vol. 13, Issue 9, Pages 752-761 ). DOI: 10.1016/S1473-3099(13)70204-4 Underlying medical conditions Source: Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Abdullah Assiri MD,Jaffar A Al-Tawfiq FACP,Abdullah A AlRabeeah FRCS,Fahad A Al-Rabiah MD,Sami Al-Hajjar MD,Ali Al-Barrak MD,Hesham Flemban MD,Wafa N Al-Nassir MD,Hanan H Balkhy MD,Rafat F Al-Hakeem MD,Hatem Q Makhdoom PhD,Prof Alimuddin I Zumla FRCP,Prof Ziad A Memish FRCP. The Lancet Infectious Diseases - 1 September 2013 ( Vol. 13, Issue 9, Pages 752-761 ). DOI: 10.1016/S1473-3099(13)70204-4 Pulmonary picture Source: Family Cluster of Middle East Respiratory Syndrome Coronavirus Infections. Ziad A. Memish, M.D., Alimuddin I. Zumla, M.D., Ph.D., Rafat F. Al-Hakeem, M.D., Abdullah A. Al-Rabeeah, M.D., and Gwen M. Stephens, M.D. Example of case Source: Family Cluster of Middle East Respiratory Syndrome Coronavirus Infections. Ziad A. Memish, M.D., Alimuddin I. Zumla, M.D., Ph.D., Rafat F. Al-Hakeem, M.D., Abdullah A. Al-Rabeeah, M.D., and Gwen M. Stephens. n engl j med 368;26 nejm.org june 27, 2013 Example of case Source: Family Cluster of Middle East Respiratory Syndrome Coronavirus Infections. Ziad A. Memish, M.D., Alimuddin I. Zumla, M.D., Ph.D., Rafat F. Al-Hakeem, M.D., Abdullah A. Al-Rabeeah, M.D., and Gwen M. Stephens. n engl j med 368;26 nejm.org june 27, 2013 Case management: Early recognition and management 1. Recognize severe manifestations of acute respiratory infections 2. Initiate infection prevention and control measures 3. Give supplemental oxygen therapy to patients with SARI 4. Collect respiratory and other specimens for laboratory testing 5. Give empiric antimicrobials to treat suspected pathogens, including community-acquired pathogens 6. Use conservative fluid management in patients with SARI when there is no evidence of shock 7. Closely monitor patients with SARI for signs of clinical deterioration, such as severe respiratory distress/respiratory failure or tissue hypoperfusion/shock, and apply supportive care interventions Source: WHO Case management: Management of severe respiratory distress, hypoxemia and ARDS 1. 2. 3. 4. 5. 6. 7. Recognize severe cases, when severe respiratory distress may not be sufficiently treated by oxygen alone, even when administered at high flow rates Wherever available, and when staff members are trained, mechanical ventilation should be instituted early in patients with increased work of breathing or hypoxemia that persists despite high-flow oxygen therapy Consider NIV if local expertise is available, when immunosuppression is also present, or in cases of mild ARDS without impaired consciousness or cardiovascular failure If equipment is available and staff are trained, proceed with endotracheal intubation to deliver invasive mechanical ventilation Use a lung-protective ventilation strategy (LPV) for patients with ARDS In patients with severe ARDS, consider adjunctive therapeutics early, especially if failing to reach LPV targets Use a conservative fluid management strategy for ARDS patients who are not in shock to shorten the duration of mechanical ventilation (18) Source: WHO Case management: infection control Standard Apply routinely in all health-care settings for all patients. precautions Standard precautions include: - hand hygiene - and use of personal protective equipment (PPE) to avoid direct contact with patients’ blood, body fluids, secretions (including respiratory secretions) and non-intact skin. When providing care in close contact with a patient with respiratory symptoms (e.g. coughing or sneezing): use eye protection, because sprays of secretions may occur. Standard precautions include: - prevention of needle-stick or sharps injury; - safe waste management; - cleaning and disinfection of equipment; - and cleaning of the environment. Source: WHO Case management: infection control Droplet precautions Use a medical mask if working within 1 meter of the patient. Place patients in single rooms, or group together those with the same etiological diagnosis. If an etiological diagnosis is not possible, group patients with similar clinical diagnosis and based on epidemiological risk factors, with a spatial separation of at least 1 meter. Limit patient movement and ensure that patients wear medical masks when outside their rooms. Source: WHO Case management: infection control Airborne precautions Ensure that healthcare workers performing aerosolgenerating procedures use PPE, including: - gloves, long-sleeved gowns, - eye protection - and particulate respirators (N95 or equivalent). Whenever possible, use adequately ventilated single rooms when performing aerosol-generating procedures. Source: WHO