Health Plan Services - Healthcare Financial Management
advertisement

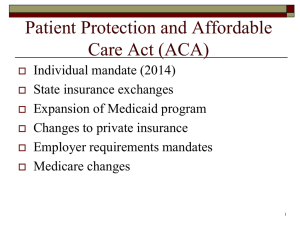
This presentation is only a high level summary of the Patient Protection and Affordable Care Act (ACA). Information contained in this presentation is subject to change as regulations are issued and interpretation evolves. This presentation should not be considered to be legal guidance regarding ACA or its potential impact. 1 Kelly McGivern Sr. Director, Government Affairs December 14, 2012 This presentation is only a high level summary of the Patient Protection and Affordable Care Act (ACA). Information contained in this presentation is subject to change as regulations are issued and interpretation evolves. This presentation should not be considered to be legal guidance regarding ACA or its potential impact. 2014 Health Care Landscape 2 Healthcare Reform Timeline Benefit coverage changes − Preventive Care at 100% in network – Dependents < age 26 – No pre-ex < age 19 – Prohibits rescissions except fraud – No lifetime limits/ annual limits on essential benefits – Patient protections – Grievance and appeals updates Temporary high-risk pool Uniform MLR definition (NAIC) HHS Web Portal 2010 2011 Guaranteed issue Individual coverage mandate Individual subsidy State individual and small group exchanges operational Rating rule changes 2012 2013 Minimum MLR requirements Medical device fee Exchange coverage notice Patient Centered Outcomes Research fee Medicare Advantage plans begin to have payments frozen MLR reporting goes “live” Medicare Advantage cost sharing Administrative limits effective Simplification begins to phase in Pharmaceutical fee Uniform summary of Rate review implementation coverage Insurer taxes Employer “Pay or Play” Mandate Essential health benefits Medicaid expansion Source: Patient Protection and Affordable Care Act FSA Cap Tax deduction for Medicare Part D subsidy eliminated 2014 90-Day maximum waiting period Auto-Enrollment Annual reporting of employee coverage Definition of full-time employees Wellness incentives 2015-2019 Increased penalties on individual mandate Increased insurer taxes States must allow groups with <100 employees into exchanges (2016) “Cadillac tax” (2018) 3 Prominent ACA Provisions in 2014 Key ACA provisions, which will become effective in 2014, will have a significant impact on the health insurance marketplace. Prohibits health plans from denying coverage or rating applicants based on their health status Creates government regulated Individual and Small Group health insurance marketplaces Guaranteed Issue (GI) and Rating Changes Risk Management Mechanisms Insurance Exchanges Institutes penalties for employers who fail to offer affordable comprehensive coverage Levels the playing field between health plans and mitigates the impact of Guaranteed Issue and pricing uncertainty in the short term Employer Mandate Taxes and Fees Levies against health insurers and other groups to fund subsidies and risk management mechanisms Key ACA provisions effective in 2014 Individual Mandate Institutes penalties for failing to purchase health insurance Tax Credits and Subsidies Lowers the cost of coverage for the low and middle income populations in the Individual market 4 Key 2014 Provision: Insurance Exchanges States have a considerable amount of flexibility in deciding how to structure their Public Individual and Small Group Exchanges. Individual Exchange Small Business Health Options Program (SHOP Exchange) Private Exchange Exchange Eligibility: Exchange Eligibility: Description: US citizen or legal alien Full-time employees of small businesses from 1 to 100 employees May allow health plans to target employers that are potentially interested in defined contribution for their employees State option to limit to businesses of 50 or less until 2017 Potentially more health plan flexibility as plans may not need to meet QHP (Qualified Health Plan) standards Not incarcerated Resident of the state in which Exchange is based Access to Premium Tax Credits and Cost Sharing Subsidies: Between 133% and 400% FPL Not offered affordable coverage through an employer States will decide on the degree of choice offered to employees through the small business Exchange and how employers can provide contributions toward employee coverage Beginning in 2017, states will have the option to open the Exchanges to large employers Regulatory issues to be considered include state insurance law, rating, anti-selection, risk management, and antitrust requirements Access to Premium Tax Credits and Cost Sharing Subsidies: No access to tax credits and subsidies 5 Exchange Implementation Timeline Health plans currently await additional Exchange guidance from Health and Human Services and States. Low 2010 Higher Degree of Clarity on Exchange Regulations from HHS and States 2011 Award Funding and Publish Legislation 2012 2013 Build Exchange Certify Exchange Health Plan Implementation Milestones Q1 – Determine Exchange technology solutions Q2 – Finalize Exchange go-to-market strategy – Begin technology build Q4 – Networks configured – Products developed and filed 2014 …2017 IVL/SG LG Exchange Coverage Exchange Exchange Effective Effective Effective Summer States notify HHS of intent to operate Exchange 6 Exchange Implementation Timeline Health plans currently await additional Exchange guidance from Health and Human Services and States. Low 2010 Higher Degree of Clarity on Exchange Regulations from HHS and States 2011 Award Funding and Publish Legislation 2012 2013 Build Exchange Certify Exchange Health Plan Implementation Milestones Q1 – Rates filed for 2014 Q2 – Submit applications to States for qualified health plans Q3 – Ready to quote / enroll Q4 – Ready to service 2014 …2017 IVL/SG LG Exchange Coverage Exchange Exchange Effective Effective Effective January HHS decides on Fallback Exchanges Fall Exchanges finalize available options Initial enrollment 7 Exchange Implementation Timeline Health plans currently await additional Exchange guidance from Health and Human Services and States. Low 2010 Higher Degree of Clarity on Exchange Regulations from HHS and States 2011 Award Funding and Publish Legislation Health Plan Implementation Milestone Q1 – Fully operational on the Exchange 2012 2013 Build Exchange Certify Exchange 2014 …2017 IVL/SG LG Exchange Coverage Exchange Exchange Effective Effective Effective January Exchange coverage becomes effective 8 Exchange Implementation Timeline Health plans currently await additional Exchange guidance from Health and Human Services and States. Low 2010 Higher Degree of Clarity on Exchange Regulations from HHS and States 2011 Award Funding and Publish Legislation 2012 2013 Build Exchange Certify Exchange 2014 …2017 IVL/SG LG Exchange Coverage Exchange Exchange Effective Effective Effective January States may permit large employers in Exchange 9 Value-Based Contracting Michelle Mathieu Daniels Vice President Network Management December 14, 2012 10 Aetna Works with Providers to Create Incremental Value Population-Based Management ACO’s Accountable Care Organizations Narrow Networks Medical Homes Narrow Networks Bundled Payments Pay for Performance Provider Alignment Transparency Tools IOEs/IOQs/Steerage Quality & Cost Transparency Utilization Management Site of Service Managing Medical Costs Discounts/Unit Cost 11 What is Value? “Value” is the patient health outcome achieved per healthcare dollar spent. Our strategy is to provide improved value through population health management, which is built on the foundation of the Triple Aim: 1) Improve patient experience/engagement; 2) Improve population health; 3) Reduce aggregate cost of care. Member/Patient Experience Provider Experience Plan Sponsor Experience * Improves system-wide patient experience and improves member/patient ownership of care. * Value is achieved if improvement in aggregate health is achieved. * Reducing disparity in cost/procedure, utilization, key to reducing cost of care. * Provider's role: Develop a strong member/provider relationship. * Network participants are rated on overall management of their population of members. * With focus on outcomes, high unit costs and utilization are no longer advantageous. * Hospital's role: Offer an optimized environment for health improvement. * Doctors' and hospitals' role: focus attention on prevention and treatment of most serious needs (i.e., chronic conditions). * Providers' and hospitals' role: Reduce cost, volume of care in partnership with payers. * Expected Outcome: Member has improved access to care, exhibits a willingness to actively engage and be better-informed to manage their own health. * Expected Outcome: Focus on PHM means aggregate gains in overall population health status, access to aggregated clinical and claims-based data to inform clinical decision-making. * Expected Outcome: Lower aggregate medical costs, improved population health, a more productive work force and healthier employees and dependents. Definition of “value” from: Porter ME. What is value in health care? N Engl J Med 2010; 363:2477-81. (10.1056/NEJMp1011024). http://www.nejm.org/doi/suppl/10.1056/NEJMp1011024/suppl_file/nejmp1011024_appendix1.pdf. “Triple Aim” from: “Triple Aim Initiative.” IHI. http://www.ihi.org/offerings/Initiatives/TripleAim/Pages/default.aspx. 12 Charting the Payment Reform Path Continuum of Payment Models Episodic Cost Accountability Traditional Fee-forService Minimal Pay-forPerformance Total Cost Accountability Bundled Payments Shared Savings Savings Potential Partial Capitation Full Capitation Substantial Source: The Advisory Board Company: Accountable Care Forum-Briefing for Health Plan Executives 13 Medicare Collaboration • Our objective is to align resources and incentives to improve outcomes • National and local focus 14 The Building Blocks of Collaboration Collaborative Care Management • Nurse Case Manager in the Participating Provider’s Group Practice • Care Managers work in collaboration with physicians to • Develop care plans • Monitor ongoing symptoms • Coach patients to manage their conditions • Continuity of care • Performance Based Compensation • Provide enhanced payment opportunities for achieving defined performance measured focus on quality, recognition and management of chronic conditions and reductions in avoidable hospital admissions and readmissions 15 The Building Blocks of Collaboration • Medicare Data Analysis • Sharing actionable information to improve recognition of chronic conditions for risk scores and achievement of quality measures • Collaboration Results • Overall Aetna MA inpatient utilization results are 31% - 34% better than FFS Medicare 16 Creating Alignment with PatientCentered Medical Homes Aetna supports the development of Patient Centered Medical Homes through pilots in eight states --- the early returns are promising Features: •Three levels of PCMH certification from the National Committee on Quality Assurance •Emphasis: Coordinated team-based primary care focused on the needs of members, populations •Standards: Access, continuity, self-care, population mgt, treatment goals, performance improvement Aligning Incentives: Per member per month coordination-of-care fee to support practice infrastructure Members are “attributed to the practice using standard attribution logic Gain sharing model so practices can benefit from incremental efficiency and clinical improvements Sample Clinical Measures: Sample Efficiency Measures: • Diabetic: A lipid management: LDL-C control <100 • Diabetes: medical attention for nephropathy • Diabetic: hemoglobin A1c management • 30-day readmissions rate • Bed days per thousand (excluding trauma/maternity) • Inpatient cost savings PMPM • ER visits per thousand 17 Aetna’s PCMH Models • Multi-Payor Collaboratives, CMS, and Comprehensive Primary Care Initiative (CPCI) • Direct Contractual Relationship • Region specific contracting pipeline • Care Coordination Fee and Shared Savings • Efficiency and Clinical Performance Monitoring • PCMH Recognition Model • Market based program • Care Coordination Fee • Efficiency and Clinical Performance Monitoring 18 More PCMH Proof Points State Cost Improvement Quality Improvement Florida 40% fewer inpatient days 37% lower ER visits 18% lower total costs Increased primary care visits by 250% Michigan 10% lower adult ER visits 17% lower ambulatory care sensitive inpatient admissions 60% better access to care Minnesota 39% lower ER visits 24% lower inpatient admissions Reduced appointment wait time from 26 days to 1 day New Jersey Reduced PMPM costs by 10% 26% lower ER visits 21% lower inpatient admissions 31% increase in ability to self-manage blood sugar 24% increase in LDL screening North Carolina 52% fewer visits to specialists 70% fewer visits to ER Medicaid saved $900 million in 3 years Medicaid: 21% increase in asthma staging 112% increase in flu innoculations Ohio 34% decrease in ER visits 22% decrease in patients with uncontrolled blood pressure Rhode Island 17-33% lower costs among PCMH members 44% increase in quality scores for family/children’s health 35% increase for women’s care Texas 23% lower readmission rates $1.2 million in estimated cost savings Results compiled by the Patient-Centered Primary Care Collaborative at: “Benefits of Implementing the Primary Care Patient-Centered Medical Home.” PCPCC. 2012. http://www.pcpcc.net/files/benefits_of_implementing_the_primary_care_pcmh.pdf. 19 Definition of Bundled Payments Bundled Payments can be defined as payments that reimburse providers on the basis of expected costs for clinically-defined episodes of care. They are a mid-point on the road to payment reform. Where Bundled Payments Have Succeeded Medicare Participating Heart Bypass Center Demo CMS (HCFA) spending declined by 15.5% in the first 2 years. CMS Acute Care Episode demonstration 20% reduction in supply costs at Hillcrest Savings of $4 million in device/supply costs at Baptist Health. Congressional Budget Office Only 1 demonstration program saved a (CBO) Study of 34 significant amount of money – using Demonstration Programs Bundled Payments. RAND Health study of payment reform options Bundling had the most to offer – the potential for a 5.4% reduction in prices. 20 Aetna and Bundled Payments With Bundled Payments, Aetna aims to support the “Triple Aim” of improved population health, improved patient experience and reduced cost of care. First Procedures for Bundled Payments Knee Replacement Hip Replacement Bariatric Surgery Infertility Services CABG Surgery Angioplasty First Principles for Bundled Payments In designing our Bundled Payment program, Aetna principles include: • • In pursuing bundles, or any payment innovation, Aetna aims to improve quality of care while reducing costs. Aetna puts a premium on quality measurement in bundles and sees the opportunity to align incentives to ensure quality care as a key advantage of bundled payments. Yet, it’s also true that: • • When it comes to Bundled Payment contracts, one size doesn’t fit all. It is important to meet providers where they are (on risk and integration). 21 Pay-for-Performance – Payment Reform’s Underpinnings Pay-for-Performance (P4P) can mean a stand-alone program, but there are P4P components to any payment mechanism that ties payment to achievement of quality metrics, including most programs whose results are on these slides. Aetna Uses P4P Principles In: ACO Bundled Payments PCMH Standalone P4P Programs Aetna’s Hospital and Specialty P4P programs offer hospitals and providers scorecards that assess their proficiency at improving outcomes and following evidence-based processes of care. They also reward facilities and providers that publicly report on the quality of the care they offer. Aetna’s goals for the program include: • Ensure quality care for the money hospitals receive. • Ensure hospitals operate efficiently. • Closing the gap between low-and-high performers. 22 Pay-for-Performance – Payment Reform’s Underpinnings P4P Details Hospital P4P # of Measures Types of Measures 39 across 3 types 15-20 Outcomes, Processes, Quality Reporting Quality, Clinical Efficiency 2%-3% of Projected Costs Reductions in ALOS, 30-Day Readmissions, alignment with Sample Improvement in Quality hospitals Voluntary, transitioning to Approach to P4P in Contracting Mandatory Expected Reduction in Spend Specialty P4P 2%-3% of Projected Costs Improved outcomes, cost containment, alignment with physicians Voluntary, transitioning to Mandatory 23 Aetna’s Way Forward 2013 PCMH Hospital P4P Specialty P4P 2014 2015 Continue implementation of national PCMH contracting strategy Nearly all eligible PCMH Primary Care Physicians in PCMH model by end of 2015 Begin implementing performancebased contracting methodology for top 30 2013 non-ACO contract renewals Hospital P4P a component of nearly all contracts by end of 2015 Begin strategically implementing performance-based payment with top contract renewals in the specialties of orthopedics, cardiology, endocrinology and OB/GYN Specialty P4P a component of nearly all contracts by end of 2015 Bundled Payments Implement Bundled payment methodologies for 14 cardiac & orthopedic Institutes of Quality around the country General Continue reporting to physicians and plan sponsors on progress on and performance of valuebased contracting strategies. 24 Quality health plans & benefits Healthier living Financial well-being Intelligent solutions Accountable Care Margaret Anson, SVP Strategy and Operations Accountable Care Solutions December 14, 2012 25 We see Accountable Care as a Broad, Transformational Commercial Model Aetna Perspective All patient model – Medicare, Medicaid, Commercial All payor model – not limited to Aetna members Committed to quality and total cost management Symmetrical risk sharing CMS Model Medicare only Defined network Shared savings Quality measures and reporting Aetna’s Accountable Care Solutions offering is a sustainable long-term model for change 26 Accountable Care Benefits All Stakeholders Lower cost, higher quality, enhanced member experience Consultants/Brokers Employers • Cost savings • Sustainable solution • Improved quality • Enhanced wellness and care management • Improved employee productivity Members • Quality-based, coordinated care • Lower out-of-pocket costs • Enhanced member experience • Tools to support a healthy lifestyle Aetna and Health System Partner • Innovative client cost savings solution • Increased growth through opportunity to differentiate • Quality indicator reports Care Providers • Infrastructure to manage populations and risk • Payment aligned with quality and outcomes • Improved compensation 27 This Is How It Works ACOs allow providers to counter significant profitability reductions via a sustainable business model Growth Performance Gap (e.g., Rate Pressure, Competitive Market Forces) Shared Savings Current Performance Future Performance Without Defensible Strategy Clinical Integration Steerage Operating Cost (Commercial, Improvement Medicare, Medicaid) Invest in New ACO Capability Clinical Efficiency and Enhanced Care Management/HIT 28 Three models of collaboration Model Clinical Integration Support All Payers Build Population Specific Models Private Label Health Plan Description Governance Network Development Business, Payment and Clinical Model Development Workflow Redesign, Clinical, IT, Care Management Infrastructure Development Change management Role and Responsibility Definition Medicare: Pioneer, Medicare Shared Savings Program, Medicare Advantage Medicaid System Employees Commercial Fully Insured Large, self funded customers Federal Employees Use of Aetna insurance license and expertise (e.g., actuarial) to enable private label or co-branded health plan offering and manage risk Leverage Aetna scale/operations – claims processing, customer service, call center, & care management (e.g., staff, programs, technology) 29 A la Carte and Turn-Key Solutions Payment Payment & Incentive Reform Models Provider Branded Health Plan Any Payer, Any Insurance Segment Strategy Development and Consulting Change Management Care Management HIT/HIE • • • • • • Telephonic CM Embedded / Embedded Telephonic CM UM, DM, CM, BH, MM DM, UM, CM Training, Staff & Programs Wellness and Lifestyle Senior Programs Clinical / IT Platform Implementation Services Physicians Hospitals CT Suite Team Suite • Care • HIE • CDS Pt PortalPortal • PHR / Patient • Analytics & Reporting • Implementation Services Out Patient Facilities Pharmacy Health Plan Services • • • • • • License Claims Member Services Sales and Marketing Actuarial / Underwriting Implementation Services Staff Home Health 30 We are better prepared this time around ACOs are not HMOs by another name THEN … … NOW Limited transparency and access to information; Absence of public policy to drive systematic change 1980s HMO Gatekeeper Model Policy and cost pressures are forcing change; Technology is available to enable transparency and collaboration with providers through aligned incentives 2000s Advent of the PPO 2012 Consumer Directed Health Plans TODAY Cost-shifting to members Care coordination through UM functions as barrier Broad networks with out-of-network moderates utilization HIT to care benefits increase cost Insufficient data to Aligned incentives Insufficient data to change consumer between payers and support care coordination Disjointed care delivery behavior and coordinate providers Limited payer/provider FFS reimbursement care Cost savings and collaboration encourages volume FFS reimbursement sustainable solutions over value encourages volume over value 31 31 Diverse Suite of Unique Tools and Services Hospital Employee Benefit Plan Administration • Dedicated service model • Clinically Integrated Delivery Model that has the ability to drive improved performance • Clinical coordination with on site programs • Business model that Rewards both partners • Population-based clinical intelligence, decision support and alerts Powered by • Creation of meaningful Payment and incentives for triple aim improvement on a defined population(s) • Custom network administration • Reporting/Data analytics • Decision support tools • Leading consumer mobile app • Symptom-to-Provider pathway • Care Management, communication and workflow technology • Navigation, access, appointments, registration • Clinical Data Integration • Provider interface • Secure Data Exchange • Cloud-based applications • Rapid / viral distribution 32 Our Strategies Deliver Benefits to all Stakeholders Consumers • Improved access, quality, affordability, and convenience • Flexible and customizable Providers Employers • Payment aligned with quality and outcomes • More affordable benefits • Infrastructure to manage populations and risk • Increased and improved engagement • Workforce productivity and human capital 33 What is Your ACO Readiness? Do you have a population based care management program? How strong is your commitment to the triple aim of better care, better health, reduced costs? Have you embraced the PCMH philosophy? Can you embrace payer discipline? Are you ready to share risk with payers or the government? Do you have an organizational commitment to transformation? How are you perceived by your community (do employers see you as a partner in helping manage their benefit costs)? Does your existing “owned” or “clinically integrated” provider network provide adequate geographic coverage for your targeted population or do you need more partners? Does your technology plan support population health management? 34 Questions? 35 Thank you 36