Arterial Blood Gas Interpretation–power point
advertisement

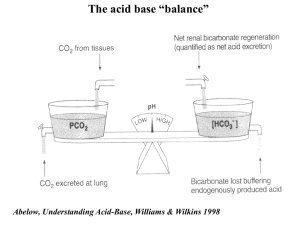
ABG Interpretation Normal Arterial Blood Gas Values PH 7.35-7.45 PaCo2 35-45 mm Hg PaO2 70-100 mm Hg (depends on age) SaO2 93-98% HCo3- 22-26 mEq/L %MetHg <2% %COHb <2% Base Excess -2.0-2.0 mEq/L CaO2 16-22 ml O2/dl The Keys to Understanding Arterial Blood Gases The determinants of PaCo2 (PaCo2 equation) The determinants of the PAo2 and Pao2 (Alveolar gas equation) Acid Base Balance (Henderson Hasselbalch equation) Determinants of Hypercapnia PaCo2 is based on the production of Co2 (VCo2) and on alveolar Ventilation (VA) Alveolar Ventilation (VA) is defined as minute ventilation (VE) minus dead space ventilation (VD) PaCo2 = VCo2 x 0.86 or VCo2 x 0.86 VA VE VD Determinants of Hypercapnia PaCo2 increases with increased production of Co2 Hypermetabolism, malignant hypothermia, high carbohydrate diet The decrease in (VA) may be due to a decrease in minute ventilation (VE) or an increase in dead space ventilation (VD) since VA = VE-VD Determinants of Hypercapnia Clinical examples of an inadequate minute ventilation VE leading to hypercapnia include Sedative Drug Overdose Respiratory muscle paralysis Central hypoventilation Examples of increased dead space ventilation (VD) leading to hypercapnia include COPD Severe restrictive lung disease with rapid shallow breathing Dangers of Hypercapnia An elevated PaCo2 will lower the PaO2 An elevated PaCo2 will lower the PH and cause acidemia The Higher the baseline PaCo2 the greater it will rise for a given decrease in Alveolar Ventilation (VA) Alveolar Gas Equation (Oxygenation) The partial pressure of oxygen in the alveolus PAo2 is based on: Inspired Fio2 Pb ( barometric pressure ) (760 mm hg at sea level) The water vapor pressure (47mm hg at normal body temperature) PACo2 ( equal to the PaCo2/RQ or PaCo2/0.8) Thus the PAo2 = Fio2 * (Pb-47mmHg)-PaCo2 / 0.8 In a pt breathing RA PAo2 = 150 – PaCo2/ 0.8 Alveolar Gas Equation (Oxygenation) PAo2 = Fio2 * (Pb – 47) – PaCo2 / 0.8 The PAo2 decreases with: Decreased inspired Fi02 Decreased Barometric Pressure (altitude) Increased PACo2 or PaCo2 P(A-a) O2 The partial pressure difference between Alveolar and arterial O2 is commonly referred to as the A-a gradient A normal A-a gradient is between 5-25 mm Hg and it increases with age. Part of this is due to normal shunting via the thesbian circulation (Age/4) + 4 estimates the normal A-a gradient for a given age An elevated A-a gradient indicates that oxygen is not adequately transferred from the alveoli to the pulmonary capillaries This usually signifies a lung problem or a cardiac shunt Causes of a Low PaO2 Non Respiratory Causes Cardiac R to L Shunt ( increased A-a gradient, does not respond to increased Fio2) Decreased inspired Fio2 or decreased barometric pressure (normal A-a gradient) Low mixed venous O2 saturation ( due to increased extraction of O2, not usually significant unless there is also a VQ mismatch or diffusion barrier) Respiratory Causes Pulmonary R to L Shunt (Increased A-a gradient) VQ mismatch (Increased A-a gradient) Diffusion barrier (Increased A-a gradient) Hypoventilation (Increased PaCo2 with a normal A-a Acid Base Balance Henderson-Hasselbalch Equation PH = pK + Log [HCo3-] .03 [PaCo2] The 2 determinants of PH are the [HCo3-] and the [PaCo2] Acid Base Balance The first step in proper ABG interpretation involves obtaining an accurate history and physical exam. This will often provide clues to the prevailing acid-base disorder and can aid in narrowing the differential diagnosis A given set of acid base parameters is never in and of itself diagnostic This is especially true for pts with drug ingestion, vomiting, diarrhea, and diabetes mellitus. Verifying the Accuracy of the Data The components of the Hco3-Co2 system should always be in equilibrium in the blood The PH, PaCo2 and serum HCo3 must be consistent with the Henderson-Hasselbalch equation. The HCo3 from the ABG is a calculated HCo3 ABG and chemistries should be drawn at the same time If the measurements do not fit reasonably well into these equations an error in one or more of the values has likely occurred and a repeat ABG and serum Hco3 should be obtained Henderson Equation The first step in ABG interpretation is determining internal consistency [H+] = 24 * PaCo2 [HCo3-] A [H+] of 40 is equal to a PH of 7.40 For every 1 mmol/L change in the [H+] the PH inversely changes by .01 Values for PH and corresponding [H+] PH 7.55 7.50 7.45 7.40 7.35 7.30 7.25 [H+] (mEq/L) 28 32 35 40 45 50 56 Determining the Serum Anion Gap The anion gap is the difference between the unmeasured anions (negatively charged molecules) and the unmeasured cations (positively charged molecules) in the serum The Concentration of all anions and cations in the serum must balance Therefore: Na + UC = [Cl + HCo3] + UA Rearranged UA – UC = Na – [Cl + HCo3] Normal in most labs is 10 + or - 2 Hypoalbuminemia, hyponatremia, and increased [k], [mg],[ca] and [NH4] may all lower the anion gap. A decrease of the serum albumin by 50% can decrease the anion gap by 5 meq/l. Determinants of the Anion Gap Unmeasured Anions Unmeasure Cations Proteins (15 meq/L) Organic Acids (5 meq/L) meq/L) Phosphates (2 meq/L) Sulfates (1meq/L) ____________________ __________________ UA = 23 meq/L Calcium (5 meq/L) Potassium (4.5 Anion gap = UA – UC = 12 meq/L Mg (1.5 meq/L) UC = 11 meq/L Determining the Delta Gap If a serum anion gap is present a Delta gap should be calculated to evaluate for an additional metabolic derangement The Delta gap can be calculated by the following equation (calculated AG – normal AG) – (Normal HCo3 – Measured HCo3) Or (Calculated AG – 12) – (24 – measured HCo3) Interpreting the Delta Gap A normal Delta gap is 0 indicating that the anion gap metabolic acidosis is the only metabolic derangement. A postive delta gap may indicate the presence of an additional metabolic alkalosis or a respiratory acidosis with metabolic compensation Conversely a negative delta gap may indicate an additional metabolic acidosis or a respiratory alkalosis with metabolic compensation Determining the Osmolar Gap The Osmolal gap is used to detect the presence of ingested toxins such as ethylene glycol, methanol or isopropyl alcohol These Toxins often cause an increased AG acidosis. The Osmolal gap is the difference between the measured osmolality and the calculated osmolality The calculated osmolality is determined by 2*[Na] + Serum Glucose/18 + BUN/2.8 +Ethanol/4.5 An Osmolal gap >10mOsm suggests the presence of an ingested toxin as a contributor to the anion gap acidosis Simple Acid Base Abnormalities The term simple acid-base disorder denotes the presence of a single abnormality associated with an expected compensatory response The Four simple acid base disorders are metabolic acidosis, metabolic alkalosis, respiratory acidosis (both acute and chronic) and respiratory alkalosis (acute and chronic) Simple Acid Base Disorders Metabolic Acidosis – primary disturbance is a decrease in HCo3 with compensatory hyperventilation and a decreased PaCo2. The Predicted PaCo2 is determined using the Winter’s equation PaCo2 = (1.5 x HCo3) + 8 + or – 2 Any significant deviation from the predicted PaCo2 signifies an additional respiratory disorder A PaCo2 higher than predicted signifies an additional Respiratory Acidosis A PaCo2 lower than predicted signifies an additional Respiratory Alkalosis Simple Acid Base Disorders Metabolic Alkalosis – Primary disturbance is an increase in HCo3 with compensatory hypoventilation and an increased PaCo2 Predicted PaCo2 = (0.7 x HCo3) + 21 + or – 1.5 Any significant deviation from the predicted PaCo2 signifies an additional Respiratory disorder Simple Acid Base Disorders Respiratory Acidosis – primary derangement is an increased PaCo2 with a compensatory increase in HCo3. In acute resp acidosis for every increase of 10 mm Hg of PaCo2 the PH should drop by .08. In Chronic resp acidosis for every 10 mm Hg rise of the PaCo2 the PH should drop by .03 as compensation but not correction Increase in [HCo3] = change PaCo2/10 + or - 3 Increase in [HCo3] = 3.5 x change Paco2/10 Changes greater than those predicted signify an additional metabolic disorder Simple Acid Base Disorders Respiratory Alkalosis – primary derangement is a decreased PaCo2 with a compensatory decrease in the HCo3 For every 10 mm Hg decrease in the PaCo2 the PH should increase by .08 in an acute disorder For every 10 mm Hg decrease in the PaCo2 the PH should increase by .03 in a chronic disorder Decrease in [HCo3] = 2x change in PaCo2/10 Decrese in [HCo3] = 5 x change in the PaCo2/10 Changes greater than those predicted signify an additional metabolic disorder Complex Acid Base Disorders Framework for Metabolic Acidosis First as always take a thorough Hx and perform a physical examination Next determine the internal consistency of the ABG Look at the PH. If it is less than 7.35 there is a primary acidosis. If the HCo3 and PaCo2 are both low it is a primary metabolic acidosis Calculate the predicted PaCo2 using the Winters equation [PaCo2= (1.5 x Hco3) +8 + or – 2]. If the PaCo2 is lower than predicted there is an additional respiratory alkalosis. If the PaCo2 is higher than predicted there is an additional respiratory acidosis Calculate the AG. If there is an AG present calculate the Delta gap. If the Delta gap is 0 there is no additional metabolic derangement. If there is a + delta gap there may be an additional metabolic alkalosis. If it is negative there may be an additional non ag metabolic acidosis Lastly if there is an AG present with no obvious etiology calculate the osmolal gap looking for toxic ingestion. Classification of Metabolic Acidosis Increased Anion gap Lactic Acidosis Ketoacidosis (Diabetes, Alcohol, Starvation) Renal Failure Toxic Ingestion Normal anion gap (Hyperchloremic metabolic Acidosis) Salicylates, Methanol, Ethylene Glycol, Paraldehyde, INH GI loss of HCo3 Renal Loss of HCo3 Renal Tubular Disease Pharmacological ( Ammonium Chloride, Dilutional, Hyperalimentation) Urine Anion gap may be used to differentiate GI vs Renal causes of a non ag metabolic Acidosis Urine AG = UA – UC = Na – [K + Cl] A negative value usually indicates a GI loss of HCo3. A value of zero or a positive value signifies a renal cause Metabolic Acidosis Clinical Signs and Symptoms Kussmaul’s Respirations – deep and rapid breathing Arrhythmias Suppressed myocardial contractility R shift of the oxyhemoglobin dissociation curve Hyperkalemia Increased protein catabolism Insulin resistence Metabolic Alkalosis The primary disturbance in metabolic alkalosis is an increase in HCo3 or the loss of acid. The compensatory respiratory response is a rise in PaCo2. Calculate the predicted PaCo2 using the following equation: PaCo2= (0.7 x HCo3) +21 + or – 1.5. If the PaCo2 is less than predicted there is an additional respiratory alkalosis. If the PaCo2 is higher than predicted there is an additional respiratory acidosis. Metabolic Alkalosis may be Hypovolemic Cldepleted or hypervolemic Cl- expanded Metabolic Alkalosis The etiology of the hypovolemic Cl - depleted form includes: The etiology of the hypervolemic Cl-expanded form includes: GI loss of H+ Vomiting, Gastric suctioning, Cl- rich diarrhea Renal loss of H+ Diuretics Post hypercapnia High dose carbenicillin Primary hyperaldosteronism, hypercortisolism ACTH excess, Hydrocortisone and mineralicorticoid excess Renin secreting tumor Hypokalemia, milk-alkali syndrome, Massive blood transfusion History and Urine Chloride can be helpful in differentiating the two Urine Chloride is usually less than 20 in the chloride depleted form and greater than 20 in the chloride expanded form Metabolic Alkalosis Clinical Signs and Symptoms Tachycardia Arrhythmias Obtunted mental Status Increased risk of seizures Decreased cerebral blood flow Hypocalcemia hypokalemia Respiratory Acidosis The major disturbance in respiratory acidosis is ineffective ventilation and or increased production of Co2. In acute disorders for every increase of 10 mm Hg in the PaCo2 the PH decreases by .08. If there is a further decrease in the PH there is an additional metabolic acidosis. Likewise if the PH is higher than predicted there is likely a metabolic alkalosis. In chronic respiratory acidosis for every 10 mm Hg increase of the PaCo2 the PH decreases by .03. Further changes signify additional metabolic derangements The Maximum Renal compensation for chronic respiratory acidosis is a HCo3 of 45. If the serum HCo3 is greater than 45 there must be an additional metabolic alkalosis Respiratory Acidosis Causes, Clinical Signs and Symptoms Causes Airway obstruction, depression of the respiratory center ( brain injury drugs ) Increased Co2 production ( hyperthermia, hypermetabolism, high carbohydrate diet ) Neuromuscular diseases Pulmonary disorders ( obstructive, restrictive, ARDS/ALI, OHS, Flail chest Clinical Signs and Symptoms Confusion, HA Asterixis Hypertension Arrhythmias and peripheral vasodilitation Respiratory Alkalosis The primary derangement in respiratory alkalosis is hyperventilation The compensatory responses are the same numerically as they are in respiratory acidosis although in the opposite directions for both acute and chronic disorders Common causes of respiratory alkalosis are: Hypoxia, acute or chronic pulmonary disease Overstimulation of the respiratory center (sepsis, pregnancy, liver disease, progesterone, salicylates, pain, and organic brain disease) Respiratory Alkalosis Clinical Signs and Symptoms Confusion Seizures Parasthesias Arrhythmias Muscle cramps Hypokalemia Hypophosphatemia hypocalcemia Examples # 1 A 28 y/o male presents with 1 day hx of acute SOB and Diarrhea ABG 7.32/24/104/12/99% Serum HCo3 23 What is the Acid base disorder? Example # 1 First step in ABG interpretation is checking the internal consistency using the henderson equation [H] = 24 x [PaCo2] / [HCo3] [H] = 24 x (24/23) = 25 The expected PH for a [H] of 25 = 7.55 The ABG and serum HCo3 are not internally consistent. An ABG and serum HCo3 need to be repeated simultaneously Example #2 A 72 y/o m with a Pmhx of COPD presents with sob and AMS. He is intubated in the ED on arrival and placed on mechanical ventilation. ABG 1 hr after intubation reveals PH 7.5 PCo2 50. What must The serum HCo3 be in order for the PH to be internally consistent? What is the predominant acid base disorder Example #2 PH 7.5 is equal to a [H] of 30 30 = 24 x 50/x X = 40, so the serum HCo3 must be 40 The predominant acid base disorder is a post hypercapnic metabolic alkalosis due to overventilation in a pt with chronic Co2 retention Example #3 A physically fit 23 y/o f goes jogging. After 20 minutes of running her RR has doubled. If an ABG was performed at that time what would you expect it to show A) normal PCo2 and PH B)Low PCo2 and high PH C)High PCo2 and low PH D)Low PCo2 and low PH Example # 3 Answer. Normal PCo2 and normal PH. During exercise Co2 production increases. In a physically fit person alveolar ventilation increases accordingly keeping PaCo2 and PH in the normal range Remember PaCo2 = VCO2/ VE - VD Example # 4 A 26 y/o homeless male is admitted to the ICU with AMS and persitent vomiting ABG 7.4 / 38 / 90 / 99% Na 149 K 3.8 Cl 100 HCo3 24 BuN 110 Cr 8.7 What is ( are ) the acid base disorder(s) Example #4 Upon cursory review there appears to be no acid base disorder However there is an AG of 25 upon closer inspection. 149 – [100 + 24] = 25 The Delta gap [25 – 12] – [24-24] is also + with a value of 13. Therefore there is an ag metabolic acidosis and a metabolic alkalosis This is likely secondary to uremia + vomiting Given Ams and renal failure an osmolal gap should also be calculated Example #5 A mountain climber ascends from sea level to 18 K feet over a 2 day period. Supplemental O2 is not used. Which of the following will not change A) Fio2 B) barometric pressure C) PaO2 D) PaCo2 E) PH Example # 6 Since the early 1980’s mountain climbers have climbed Mt Everest without supplemental O2. How is this possible? Barometric Pressure at the summit is 253 mm Hg. Assume a PaCo2 of 40 PAo2 = Fi02 * ( 253 – 47 ) – 40/0.8 PA02 = .21 (206) – 50 = -6.7 ?? If we take into account a nml A-a gradient of 5 the PaO2 is –11.7?? Example # 6 In Fact these climbers profoundly hyperventilate and have PaCo2 usually < 10 mm Hg. If we plug this into the Alveolar gas equation we get a PAo2 of about 35 mm Hg. Although this is profoudly low a physically fit person can survive this, although they develop dizziness, confusion and SOB The END