2011 Acid base - Emory University Department of Pediatrics
advertisement
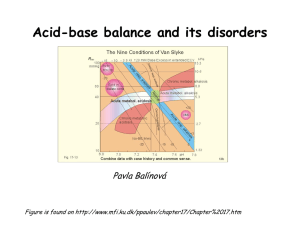
Acid-Base Analysis Pediatric Critical Care Medicine Emory University Children’s Healthcare of Atlanta Sources of acids Volatile acids H2O + dissolved CO2 H2CO3 Non-volatile acids Inorganic acid Organic acid H+ + HCO3Lactic acid Keto acid Henderson-Hasselbalch pH = pKa + log [A-] [HA] and pH = pKa + log [HCO3-] = 6.1 + log [HCO3-] s x PCO2 0.03 x PCO2 H+ + HCO3- H2CO3 CO2 + H2O Anion Gap [Na+] = [CL- + HCO3-] ~ 10-15 Acid-Base States • Acidosis: pH<7.35 – Metabolic: increased acid or decreased in bicarb – Respiratory: increased PCO2 • Alkalosis: pH>7.45 – Metabolic: increased bicarb or loss of H+ – Respiratory: decreased PCO2 Compensation • Acute: – Minutes – Respiratory: PCO2 regulation • Chronic – Hours to days – Renal: via regulation of bicarb excretion Acidosis: Respiratory • Decrease PCO2 excretion via hypoventilation – Respiratory etiology – CNS pathology – Intoxication • pH decreases 0.08 unit/10 mmHg increase in PaCO2 • Bicarb and base excess are normal Acidosis: Metabolic • Change in pH by increased in acid or decrease in bicarb • Anion Gap Acidosis: MUD PILES Methanol Paraldehyde Uremia Diabetic ketoacidosis Iron, isoniazid (INH) Lactic acid Ethanol, ethylene glycol Salicylates • Non-Anion Gap Acidosis: USEDCARP Uretorostomy Small bowel fistula Extra Chloride Diarrhea Carbonic anhydrase inhibitors (acetazolamide) Adrenal insufficiency RTA Pancreatic fistula Alkalosis: Respiratory • Decrease in PCO2 by hyperventilation • Compensate by increase renal excretion of HCO3- Alkalosis: Metabolic • Increase in H+ loss or increase in HCO3• PaCO2 increase by 0.5-1/1 mEq/L of increase in HCO3- Nomenclature Uncompensated metab acidosis Compensated metab acidosis Uncompensated metab alkalosis Compensated metab alkalosis pH pCO2 [HCO3] BE N N N N Partial Pressure Gas % Total Air at sea level Partial Pressure 760 Oxygen 20.9% 159 Nitrogen 79.0% 600 Alveolar gas at sea level CO2 Oxygen 13.3% 101 Nitrogen 75.2% 572 CO2 5.3% 40 Water 6.2% 47 pCO2 pO2 0 Atmosphere 160 40 alv 100 45 systemic circulation Capillary ~47 97 ~47 <39 <54 extravascular fluid ~5 >55 cells <1 Endothelium ECF Cells CO2 RBC 5% 30% CO2 CO2 65% Dissolved CO2 = pCO2 CO2 + Hb = HbCO2 CO2 + H2O = HCO3 + H+ CarboxyHgb Utilizes carbonic anhydrase CO2 CO2 Transport Excretion of CO2 • Metabolic rate determines how much CO2 enters blood • Lung function determines how much CO2 excreted – minute ventilation – alveolar perfusion – blood CO2 content Hgb dissociation curve % Sat 20 40 100 75 50 pO2 25 60 80 100 Dissociation curve % Sat 120 100 Shifts 80 60 40 20 0 0 20 40 60 pO2 80 100 120 Alveolar oxygen equation • Inspired oxygen = 760 x .21 = 160 torr • Ideal alveolar oxygen = PAO2 = [PB - PH2O] x FiO2 - [PaCO2/RQ] = [760 - 47] x 0.21 - [40/0.8] = [713] x 0.21 -[50] = 100 torr or 100 mmHg • If perfect equilibrium, then alveolar oxygen equals arterial oxygen. • ~5% shunt in normal lungs Normal Oxygen Levels FiO2 PaO2 0.30 >150 0.40 >200 0.50 >250 0.80 >400 1.0 >500 Predicting ‘respiratory part’ of pH • Determine difference between PaCO2 and 40 torr, then move decimal place left 2, ie: IF PCO2 76: 76 - 40 = 36 x 1/2 = 18 7.40 - 0.18 = 7.22 IF PCO2 = 18: 40 -18 = 22 7.40 + 0.22 = 7.62 Predicting metabolic component • Determine ‘predicted’ pH • Determine difference between predicted and actual pH • 2/3 of that value is the base excess/deficit Deficit examples • If pH = 7.04, PCO2 = 76 Predicted pH = 7.22 7.22 - 7.40 = 0.18 18 x 2/3 = 12 deficit • If pH = 7.47, PCO2 = 18 Predicted pH =7.62 7.62 - 7.47 = 0.15 15 x 2/3 = 10 excess Hypoxemia - etiology • Decreased PAO2 (alveolar oxygen) – Hypoventilation – Breathing FiO2 <0.21 – Unde rventilated alveoli (low V/Q) • Zero V/Q (true shunt) • Decreased mixed venous oxygen content – Increased metabolic rate – Decreased cardiac output – Decreased arterial oxygen content Blood gases • PaCO2: pH relationship – For every 20 torr increase in PaCO2, pH decreases by 0.10 – For every 10 torr decrease in PaCO2, pH increases by 0.10 • PaCO2: plasma bicarbonate relationship – PaCO2 increase of 10 torr results in bicarbonate increasing by 1 mmol/L – Acute PaCO2 decrease of 10 torr will decrease bicarb by 2 mmol/L Sources of blood acids • INFORMATION 24 Sources of blood acids • INFORMATION 25