5. Pharmacokinetics3 Distrubution and Elimination
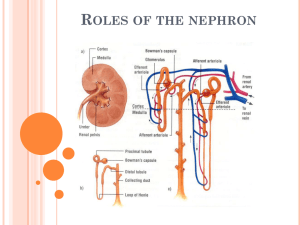
advertisement
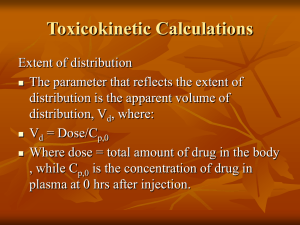
Pharmacokinetics: ASMAH NASSER, M.D. What Happens After Drug Administration? Absorption Distribution Metabolism Elimination /Excretion Volume of Distribution The measure of the space available in the body to contain the drug. Drugs that attaches to tissues has a high Vd Drugs that are highly protein bound has a low Vd Vd = Amount of drug concentration in the body Plasma drug concentration level Plasma Protein Binding of drugs Drugs attaches to PP and stay in an inactive form. They serve as reservoirs and unbound to maintain equilibrium. Acidic drugs binds to Albumin Basic drugs binds to α–acid glycprotein Drugs that are highly PPB (>70%): Sulfas, Phenytoin, Warfarin Question 68 year old woman with PMH of recurrent DVTs placed on lifelong Warfarin developed a urinary tract infection. She was placed on Bactrim (trimethoprimcotrimoxazole- a type of sulfa drug). Shortly after, she develops easy bruising and bleeding. What is the cause for this? Pharmacokinetics ELIMINATION Elimination Most drugs undergo First order kinetics. Rate of elimination is directly proportional to plasma concentration of the drug Few drugs undergo Zero order kinetics Rate of elimination is independent of plasma concentration of the drug i.e. Alcohol First order kinetics Rate of elimination is related to the plasma concentration. A certain portion of the concentration of the drug is eliminated throughout a period of time. A constant fraction (instead of amount) of a drug is being eliminated per unit time • Example : 64 mg, 32 mg, 16 mg, 8 mg, 4 mg, 2 mg, 1 mg, 0.5 mg, 0.25 mg, 0.125 mg, 0.0625 mg, etc. Plasma half life (T ½) Also known as the Elimination half life. Time required to reduce the plasma concentration of a drug dose to half. A half life is a constant that follows first order kinetics. Purpose of Plasma half life (T ½) Useful in estimating: The duration of action of a single dose time to reach steady state concentration.. (Css) of drug (chronic dosing),Usually 4-5 T1/2 Ultimately decides the dosing interval Plasma Concentration time plot of a drug eliminated by first order kinetics after a I.V. Injection 1 t1/2 =50% drug eliminated 2 t1/2 =75% drug eliminated 3 t1/2 =87.5% drug eliminated 4 t1/2 =93.75% drug eliminated Half life (T ½) t1/2 =0.7xVd/CL Vd = Volume of distribution Cl = clearance OR k = 0.693/T1/2 t1/2 =0.693/k Elimination The pharmacokinetic parameter which gives a quantitative measure of drug elimination is named….. Clearance Definition of Clearance The Clearance (Cl) of a drug is defined as the volume of a biological fluid (generally plasma) from which that drug is removed ("cleared") in the unit of time (min). Stated in another way, Clearance is the rate of elimination of a drug by all routes, relative to the concentration of that drug in any biological fluid. Clearance Clearance of a drug is the factor that predicts the rate of elimination in relation to the drug concentration CL = Rate of elimination plasma conc expressed as ml/minute It is the volume of the plasma (blood) cleared of the drug in unit time OR CL=VdxKd Why is clearance important? Clearance determines: Maintenance dose Loading dose Peak onset of action Duration of action of drug Drug in Plasma ………………… ………………… ………………… ………………… ………………… 10µg/ml ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… . Organs of drug elimination ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… ………………… <. 10µg/ml CL = 500µg/min 10µg/ml 500µg per min = 50ml/min Steady state concentration… Css On continuous steady administration of a drug, plasma concentration will rise fast at first, then more slowly and reach a plateau, where rate of administration = rate of elimination i.e steady state is reached Steady state (Css) is the situation at which the rate of drug administration is equal to the rate of drug elimination so that the amount of drug remains constant Steady state concentration… Css On continuous steady administration of a drug, plasma concentration will rise fast at first, then more slowly and reach a plateau, where rate of administration = rate of elimination i.e steady state is reached Steady state (Css) is the situation at which the rate of drug administration is equal to the rate of drug elimination so that the amount of drug remains constant Loading dose Repeated dosing or one large dose/bolus to initiate a target plasma drug level rapidly. Clearance determines the drug concentration at steady state during continuous administration Because elimination is occurring to some extent all the time, if we just administer the maintenance dose, it will take some time to reach steady state Therefore, we can give a loading dose to “fill up” the system, so that steady state is achieved more quickly Loading dose Loading dose = Vd x Target Concentration bioavailability (rememeber!) Vd = Amt of drug in body/Plasma drug concentration Maintainance Dose In most clinical situations, drugs are administered in such a way as to maintain a steady state of drug in the body, ie, just enough drug is given in each dose to replace the drug eliminated since the preceding dose. Thus, calculation of the appropriate maintenance dose is a primary goal. Maintainance dose = clearance x plasma conc bioavailability What is the half life? Time After Aminoglycoside Plasma Concentration Dosing Stopped (h) (mg/mL) 7.0 0.0 6.4 0.5 5.8 1.0 4.6 2.0 3.7 3.0 3.0 4.0 2.4 5.0 1.9 6.0 1.3 8.0 Pharmacokinetics EXCRETION Drug Elimination Drugs are eliminated from the body by two different processes: 1) Biotransformation (the biotransformed drug is no longer present as such in the body) 2) Excretion (the drug is transported outside the body via the kidney and other organs) Renal Excretion Depends on following factors Glomerular Filtration Tubular reabsorption Tubular secretion Reabsorption filtration secretion secretion Filtration • Filtration ……. free drug only, not protein bound • Reabsorption….passive, lipid soluble form only (pH) • Secretion ……. active, acids and bases Glomerular Filtration All protein unbound drug is filtered Doesn’t depend upon lipid solubility of the drug Depends on protein binding and renal blood flow Tubular reabsorption Depends on ionization and lipid solubility Depends on pH of urine Lipid soluble drugs are reabsorbed back Ionized drugs cannot be reabsorbed (Think of the same concept we’ve spoken back in the Absorption lecture) REMEMBER! Acidic drugs are better Absorbed in Acidic medium (low pH) ….AAA… eg: Aspirin better absorbed in stomach Basic drugs Better absorbed in Basic medium (high pH)……BBB Eg: Amphetamine better absorbed in Intestine Absorption is better if drug is non-ionized (Uncharged, lipid soluble, unpolarised) because it can cross the cell membrane Excretion is better if the drug is more ionized (Charged, Lipid insoluble , Polarised , Water soluble) because it cannot cross the cell membrane Tubular secretion Independent of plasma protein binding of drug Independent of lipid solubility of the drug Takes place mainly at proximal convoluted tubule by carrier mediated transport processes .Transport systems are bidirectional. Competitve Question Probenecid is moved into the urine by the same transport pump that moves many antibiotics. Why is probenecid sometimes given as an adjunct to antibiotic therapy? Examples of drugs that are activeily secreted Penicillins Cephalosporins Salicylic acid Probenecid Ethacrinic acid Probenecid and Penicillin Probenecid decreases the active secretion of penicillin, therefore inreasing the duration of action of penicillin Similarly….. Probenecid, also competes with Uric acid for reabsorption in renal tubule. So uric acid reabsorption is reduced and more has to be excreted in urine….. Probenecid is therefore used as a treatment for? pH of urine Acidic drugs are more ionized and not reabsorbed in alkaline urine Basic drugs are more ionized and not reabsorbed in acidic urine Acidification and alkalinization of urine will facilitate the renal excretion of basic and acidic drugs respectively Alkalinize urine in Barbiturate and Aspirin poiseninig. Acidify urine in Morphine,Amphetamine poisoning How to treat Drug poisening by renal secretion Acidification of urine (in basic drug poisoning) Give Ammonium chloride i.e. Morphine, Amphetamine overdose Alkalinization of urine(in acidic drug poisoning) Give Sodium bicarbonate i.e. Aspirinoverdose Summary of Excretion Acidification of urine (in basic drug poisoning) Give Ammonium chloride or Vitamin C or Canberry juice Urine acidified in Morphine, Amphetamine poisoning Alkalinization of urine(in acidic drug poisoning) Give Sodium bicarbonate or Acetazolamide Urine alkalinized in Barbiturate,Aspirin Probenecid is combined with penicillin to increase penicillin's duration of action Probencid is used in Gout!!!! Promotes excretion of uric acid Question A patient has overdosed on phenobartital. Phenobarbital is an acid. How to increase renal secretion of this drug? Question A patient who experiences migraines has accidentally overdosed with methysergide, a weak base of pKa=6.5. If urinary pH in this patient is 5.5, which of the following statements regarding elimination of methysergide from the body is accurate? A. Increase in urinary pH will increase excretion rate. B. Urinary excretion is already maximal, and changes in pH will have no effect. C. Attempts should be made to acidify the urine to at least 4 units below drug pKa. D. At urinary pH of 5.5, methysergide is 99% ionized. E. None of the above