Epidemiology Toolkit for
Outbreak Investigation
Meirion Evans
Communicable Disease Surveillance Centre
Insert name of
presentation on
What is an outbreak?
Occurrence of more cases of disease
than expected
• Over a particular period of time
• In a given area
• Among a specific group of people
(incidents, clusters)
Key questions
What is going on?
ASSESS
Who is affected?
DESCRIBE
What is the cause?
ANALYSE
What should be done?
ACT
10 steps in outbreak investigation
1.
Confirm existence of an outbreak
2.
Corroborate diagnosis
3.
Define and identify cases
4.
Collect and collate data
5.
Characterise cases (person - place - time)
6.
Develop hypotheses
7.
Test hypotheses
8.
Verify biological coherence
9.
Communicate results and write report
10. Implement control measures
10 steps in outbreak investigation
Confirm existence of an outbreak
Descriptive
epidemiology
Corroborate
diagnosis
3.
Define and identify cases
4.
Collect and collate data
5.
Characterise cases (person - place - time)
6.
Develop hypotheses
7.
Test hypotheses
8.
Verify biological coherence
Communicate results and write report
Analytical epidemiology
Implement control measures
Descriptive epidemiology
Define & identify cases
Collect & collate data
Characterise cases
Develop hypotheses
Descriptive epidemiology
OBJECTIVES
To refine the case definition
To develop a demographic profile
To identify people at risk
To develop hypotheses about
• Potential sources of exposure
• Potential routes of transmission
Case definition
Set of criteria…
• for deciding if a person should be classified as
•
having the disease
for the purposes of that stage of the investigation
Clinical and/or laboratory criteria
Time
Place
Person
• Tiered definitions: confirmed, probable, possible
Case definition
outbreak of salmonellosis in Swansea, 2011
Confirmed case
diarrhoea
• (> 2 liquid stools per day)
Probable case
diarrhoea
• (> 2 liquid stools per day)
and/or fever > 38°C
• (for at least one day)
and
and
an isolate of S. Typhimurium
contact (same household) with a
confirmed case
in a resident of Swansea
after May 2011
in a resident of Swansea
after May 2011
Case definition
sensitivity vs. specificity
Low
Specificity
Possible
High
Sensitivity
High
Specificity
Probable
Confirmed
Low
Sensitivity
Identify &
count cases
reports from staff
laboratory data
occupational health
hospitals records
GPs, etc
Collect data
demographics
clinical details (outcome)
risk factors (exposure)
Collect data
Detailed interviews
• symptoms and date of onset
• case characteristics
• all relevant exposures in relevant period
Visit (examine) some cases
Speak with clinicians
Obtain lab confirmation
Collect data
Collate data
Line listing
Example line list
Case
No.
Name
1
2
3
4
5
6
XY
AB
CD
…
…
…
Date
of birth
Date of
onset
Date of
report
Lab
results
Line listing - principles
Constitutes a unique MASTER LIST
• avoids confusion with multiple versions
• suitable for sharing
Contains unique identifier for each record
Ensures confidentiality
Contains essential information on each case
• time, place, person, clinical, lab, etc.
Can be updated as the investigation develops
Prepares data for simple descriptive analysis
Collect data
Collate data
Characterise cases
describe in
- person
- place
- time
Characterise cases
Who are the cases?
Where do they live, work, etc.?
When did they become ill?
Classify cases by:
• Person
• Place
• Time
Characterise cases
Time
Person
25
1200
1000
800
600
400
200
0
Place
20
15
10
5
0
0-4
'5-14 '15-44 '45-64
1
'64+
2
3
4
5
6
7
8
9
Age Group
Develop hypotheses
Pathogen?
Source?
Transmission?
10
Person
WHO is getting the disease?
Sex and age group
Ethnicity
Pre-existing conditions
Medication
Invasive procedures
Surgical treatment
Person
C. difficile outbreak in peri-partum women
Place
WHERE is the disease occurring?
In the community
• Place of residence
• Place of work
In hospital
• Floor
• Ward or unit
• Operating theatre
• Outpatient departments
Place
Measles outbreak in a local community
Time
WHEN does the disease occur?
Figure
1. Reported
cases
campylobacteriosis
(n=45)
Svolvær,X,
Norway,
Figure.
Cases
of of
gastroenteritis
(n=45)
in in
Hospital
Walesby
date of onset January
and
1997.
by date
ofFebruary
onset, January
and February 2012
patientcase
case
= 11primary
10
= 11secondary
staff casehousehold case
5
22 23 24 25 26 27 28 29 30 31 1
January
2
3
4
5
6
February
7
8
9 10
Time - use of the epidemic curve
To describe the outbreak
• Start date, end date, duration
• Peak, shape, magnitude
• Outliers and atypical cases
To develop hypotheses
• Incubation period
• Aetiological agent
• Type of source and transmission
• Time of exposure
Time
C. difficile outbreak timeline
Time
Pseudomonas on a neonatal ICU
Develop hypotheses
What is the disease?
Who is at risk of becoming ill?
What is the source and the vehicle?
What is the mode of transmission?
Analytical epidemiology
Test hypotheses
Verify biological coherence
Analytical epidemiology
OBJECTIVES
To test hypotheses
• Is there an association between exposure
•
•
•
and disease?
How strong is the association?
What proportion of cases are explained by
the exposure?
Is there an increased risk of disease with
increased exposure (dose-response)?
Test hypotheses
Analytical studies
• Cohort study
• Case-control study
These must test specific hypotheses
Compare the predictions of your hypotheses
with further investigations
Testing hypothesis - comparing groups
Cohort study
- attack rate exposed group
- attack rate unexposed group
= risk ratio
Case control study
- proportion of cases exposed
- proportion of controls exposed
= odds ratio
Cohort Study
Identify a cohort
• Categorise individuals based on whether or
•
not they were exposed
Compare attack rates
exposed vs unexposed
Suitable when a cohort is easily identifiable
e.g. specific ward(s), operating theatre list(s)
Case-Control Study
Identify cases
• that meet the case definition
Select non-diseased individuals from the
same population to act as controls
Compare proportions exposed
• cases vs. controls
Suitable when a distinct group is not easily
identifiable e.g. long-term outbreak, OPD
Cohort study two-by-two table
Calculate association between exposure & disease
Ill
Well
Exposed
a
b
a+b
Unexposed
c
d
c+d
Total
Total
N
Risk ratio [RR] = a/(a+b) / c/(c+d)
CC study two-by-two table
Calculate association between disease & exposure
Case
Control
Exposed
a
b
Unexposed
c
d
Total
Total
N
Odds ratio [OR] = ad/bc
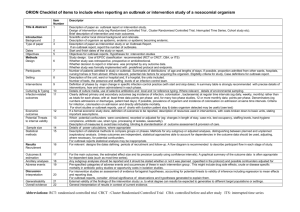
Table from a case control study
Risk factors for MRSA bacteraemia
Cases
n=42
Controls
n=90
Odds Ratio
Indwelling catheter on admission
5
3
3.9
Prior admission
35
66
1.8
Bed sore
5
1
12.0
Skin ulcer
5
5
2.3
Central line during admission
17
1
60.5
Urinary catheter during admission
22
2
48.4
Blood transfusion
15
7
6.6
Exposure
On admission
On or during admission
During admission
Verify biological coherence
Corroborative studies
• Microbiological investigation
suspected sources or vehicles of transmission
typing and molecular diagnostics
• Environmental investigation
• Traceback investigations (origin of supplies)
• Air circulation data
The reality….
time
Confirmation
Site visit
Recommendations
Case definition
Outbreak
report
Organise data
Confirm Diagnosis
Outbreak
suspected Form Outbreak
Control Team
Descriptive
Epidemiology
Line list
Analytical
Epidemiology
Control measures
Methodological issues
Keep things simple
Stick to basic principles
Get as much information as possible
Be clear what the key questions are
Design investigations to test
hypotheses appropriately