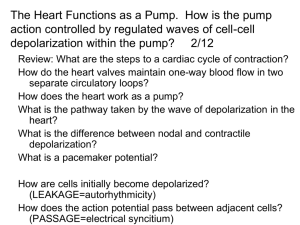
Phases of Action Potential
advertisement

Cardiovascular System • Heart – cardiac muscle physiology –Cardiac conduction system –Heart structures • Vessels- arteries and veins • Blood – WBC, RBC and Platelets, =Formed elements plus the plasma (the fluid) Types of Cardiac Cells • Auto-rhythmic cells = pacemaker cells (depolarize spontaneously) • Contractile cells – myofibrils –connected well together to form “functional Syncitium” for myocardium contraction Ease of movement between cells (conductivity) Mechanical and Electrical • Critical to remember that there is mechanical aspects to heart function=myofibrils and electrical aspect – Pacemaker cells and – Resulting AP from these cells to working muscle cells causes depolarization and repolarization C onduction S ystem of H eart C oordinates contraction of heart m uscle. 2 0 -1 Conduction System of Heart Autorhythmic Cells Cells fire spontaneously, act as pacemaker and form conduction system for the heart • SA node – cluster of cells in wall of Rt. Atria – begins heart activity that spreads to both atria – excitation spreads to AV node • AV node – in atrial septum, transmits signal to bundle of His • AV bundle of His – the connection between atria and ventricles • Bundle branches – To right and left side of heart along ventricular septum • Purkinje fibers, – large diameter fibers that conduct signals quickly in ventricles Rhythm of Conduction System • SA node fires spontaneously 80-100 times per minute • AV node fires at 40-60 times per minute • If both nodes are suppressed fibers in ventricles by themselves fire only 20-40 times per minute • Artificial pacemaker needed if pace is too slow • Extra beats forming at other sites are called ectopic pacemakers – caffeine & nicotine increase activity How does these cells automatically fire?? Timing of Atrial & Ventricular Excitation • SA node setting pace since is the fastest • In 50 msec excitation spreads through both atria and down to AV node • 100 msec delay at AV node due to smaller diameter fibers- allows atria to fully contract filling ventricles before ventricles contract • In 50 msec excitation spreads through both ventricles simultaneously Cardiac Muscle Cells-Myofibrils Physiology of Contraction • Depolarization, plateau, repolarization Important Electrolytes • Sodium – major extracellular ion • Potassium - major intracellular ion • Chloride - negative ion • Calcium - very important for muscle contraction Normal Resting Membrane Protein Channels • Special channels allow cations to go through membrane Will cause membrane charge to rise towards 0mV Action Potential Origin •Channel proteins •Voltage gated ion channels •potassium •sodium Sodium & Potassium Channels • Responds to concentration gradients • “depolarization” = movement away from resting potential towards or above 0 mV • “repolarization” = return to resting potential -90 mV • Necessity of channels Overview of Ion Movement Depolarization • Action potential movement = ion exchange • Sodium moves into cell • Potassium moves out of cell •0 Membrane potential rises -70 •this picture shows a neuron • the principle is the same in a cardiac cell Gap Junctions Depolarization Fast and Slow Channels • Sodium and Potassium ions utilize both fast and slow channels – Sodium enters cells via slow channels until “threshold” is reached – Mass of sodium then enters cell via the fast channels during contraction Repolarization • Bringing the membrane back to its resting state • Active pump moves ions against the gradients • Sodium/Potassium Pump Sodium/Potassium Pump • Maintains concentration • ~ 80% of metabolic energy consumed by pump • “Leaky membrane” – Sodium leaks in – Potassium leaks out Phases of the Action Potential • Specific sequence of events • Phases 0 through 4 • Important to know what happens in each phase – Comprehension of pathology and pharmacotherapy Phases of Action Potential • Phase 0 = Na+ channels open slow then fast • Phase 1 = K+ channels open slow Phases of Action Potential • Phase 2 = Ca+ channels open • Phase 3 = K+ channels open Phases of Action Potential • Phase 4 - Na/K pump returns membrane to rest • Na+ leaks = • Slow phase 4 rise = • automaticity The Condensed Version • Maintenance of membranes resting potential • External force (stimulus) • Slow rise brings it to threshold at - 70 mV • Ion exchange begins • Na+, then Ca+ into cell • K+ out of cell Depolarization & Repolarization • Depolarization – Cardiac cell resting membrane potential is -90mv – excitation spreads through gap junctions – fast Na+ channels open for rapid depolarization • Plateau phase – 250 msec (only 1msec in neuron) – slow Ca+2 channels open, let Ca +2 enter from outside cell and from storage in sarcoplasmic reticulum, while K+ channels close – Ca +2 binds to troponin to allow for actin-myosin cross-bridge formation & tension development • Repolarization – Ca+2 channels close and K+ channels open & -90mv is restored as potassium entering the cell • Refractory period – very long so heart can fill with blood Action Potential in Cardiac Muscle Changes in cell membrane permeability. Electrocardiogram---ECG or EKG • EKG – Action potentials of all active cells can be detected and recorded • P wave – atrial depolarization • P to R interval – conduction time from atrial to ventricular excitation • QRS complex – ventricular depolarization • T wave – ventricular repolarization One Cardiac Cycle • At 75 beats/min, one cycle requires 0.8 sec. – systole (contraction) and diastole (relaxation) of both atria, plus the systole and diastole of both ventricles • Stroke volume (SV) – the volume ejected per beat from each ventricle, about 70ml MEDIC Point: What would the normal amount of blood pumped out of the Left ventricle be in 1 minute? Phases of Cardiac Cycle • Isovolumetric relaxation – brief period when volume in ventricles does not change--as ventricles relax, pressure drops and AV valves open • Ventricular filling – rapid ventricular filling:as blood flows from full atria – diastasis: as blood flows from atria in smaller volume – atrial systole pushes final 20-25 ml blood into ventricle • Ventricular systole – ventricular systole – isovolumetric contraction • brief period, AV valves close before SL valves open – ventricular ejection: as SL valves open and blood is ejected Ventricular Pressures • Blood pressure in aorta is 120mm Hg • Blood pressure in pulmonary trunk is 30mm Hg • Differences in ventricle wall thickness allows heart to push the same amount of blood with more force from the left ventricle • The volume of blood ejected from each ventricle is 70ml (stroke volume) • Why do both stroke volumes need to be same?


![Cardio Review 4 Quince [CAPT],Joan,Juliet](http://s2.studylib.net/store/data/005719604_1-e21fbd83f7c61c5668353826e4debbb3-300x300.png)