GRAM STAINING
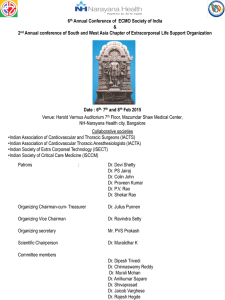
advertisement

GRAM STAINING Dr.T.V.Rao MD Dr.T.V.Rao MD 1 Hans Christian Joachim Gram Danish Bacteriologist Dr.T.V.Rao MD 2 Dyes become Stains With interest in the effects of dyes on living tissue. In 1884 the Danish microbiologist Hans Christian Gram discovered that crystal violet irreversibly stains certain bacteria but can be washed from others. The dye has been widely used ever since for the Gram stain technique, which identifies bacteria as gram-positive (the stain is retained) or gram-negative (the stain is washed). Dr.T.V.Rao MD 3 Gram staining a Important Technique A staining technique used to classify bacteria; bacteria are stained with gentian violet and then treated with Gram's solution; after being decolorized with alcohol and treated with safranine and washed in water, those that retain the gentian violet are Gram-positive and those that do not retain it are Gramnegative Dr.T.V.Rao MD 4 Gram positive Bacteria Gram positive bacteria have a thick cell wall of peptidoglycan and other polymers. Peptidoglycan consists of interleaving filaments made up of alternating acetylmuramic acid and actylglucosamine monomers. In Gram positive bacteria, there are "wall teichoic acids". As well, between the cell wall and cell membrane, there is a "membrane teichoic acid". Dr.T.V.Rao MD 5 Gram Negative Bacteria Dr.T.V.Rao MD Gram negative bacteria have an outer membrane of phospholipids and bacterial Lipopolysaccharides outside of their thin peptidoglycan layer. The space between the outer membrane and the peptidoglycan layer is called the periplasmic space. The outer membrane protects Gram negative bacteria against penicillin and lysozymes. 6 The Cell walls differ… Dr.T.V.Rao MD 7 Constituents of the Cell wall make difference Dr.T.V.Rao MD 8 Definition of Gram stain A method of staining bacteria using a violet stain. The gram staining characteristics (denoted as positive or negative). A heat fixed bacterial smear is stained with crystal violet (methyl violet), treated with 3% iodine/potassium iodide solution, washed with alcohol and counterstained. The method differentiates bacteria into two main classes, grampositive and gram-negative. Dr.T.V.Rao MD 9 Organizing the Staining Bottles Dr.T.V.Rao MD 10 Method of Picking material from Agar plates Wrong Right Dr.T.V.Rao MD 11 Prefer to pick up colonies with loop and smear on Clean glass slide Dr.T.V.Rao MD 12 Making a Smear First prepare your slide. You do this by placing bacteria on a slide in a drop of water, allowing them to dry and then heat fixing them. Heating the slide kills the bacteria and makes sure that the bacteria a stuck to the slide and wont wash away during the staining procedure Dr.T.V.Rao MD 13 Choosing a Right Smear Before choosing a field for microscopic examination, it is important to look at the smear macroscopically Note that the smear is easily visible in ordinary light Dr.T.V.Rao MD 14 Requirements for Gram staining technique Glass slides (25 by 75 mm), frosted ends desirable b. 0.85% Nacl, sterile c. Pasteur pipettes and wood applicator sticks, sterile d. Microbiological loops, inoculating needles e. Supplies for disposal of biological waste, including “sharps” f. Bunsen burner g. Immersion oil Dr.T.V.Rao MD 15 Dr.T.V.Rao MD 16 Making Multiple smears in same slide – conserve resources Making multiple smears make the optimal use of the slide. Reduces the economic costs and saves the technical time. Dr.T.V.Rao MD 17 Correct preparation Smear preparation: Proper smear preparation should produce a monolayer of organisms sufficiently dense for easy visualization but thin enough to reveal characteristic morphological characteristics. Use clean, new glass slides. NOTE: When using the same pipette or swab, always inoculate culture media first Dr.T.V.Rao MD 18 Steps in Gram Staining Procedure- Follow the Clock 1 On a rack, flood with filtered crystal violet 10 sec 2 Wash briefly in water to remove excess crystal violet 3. Flood with Gram’s iodine 10 sec 4. Wash briefly in water, do not let the section dry out. 5. Decolourise with acetone until the moving dye front has passed the lower edge of the section 6. Wash immediately in tap water 7. Note : If the section appears too blue repeat steps 6 and 7 8. Counterstain with safranin 15 seconds Dr.T.V.Rao MD 19 Proceed in organized Fashion Dr.T.V.Rao MD 20 Step 1 Dr.T.V.Rao MD 21 Step 2 Dr.T.V.Rao MD 22 Step 3 Dr.T.V.Rao MD 23 Step 4 Dr.T.V.Rao MD 24 Step 5 Dr.T.V.Rao MD 25 Step 6 Dr.T.V.Rao MD 26 Step 7 Dr.T.V.Rao MD 27 Observe the Following Under Oil Immersion lens i. Relative amounts of PMN’s, mononuclear cells, and RBC's ii. Relative amounts of squamous epithelial cells, bacteria consistent with normal micro flora, which may indicate an improperly collected specimen iii. Location and arrangements of microorganisms Note any special character sticks Dr.T.V.Rao MD 28 Microscopy: The Instruments In a compound microscope the image from the objective lens is magnified again by the ocular lens. Total magnification = objective lens ocular lens Dr.T.V.Rao MD 29 Microscopy: The Instruments Resolution is the ability of the lenses to distinguish two points. A microscope with a resolving power of 0.4 nm can distinguish between two points ≥ 0.4 nm. Shorter wavelengths of light provide greater resolution. Dr.T.V.Rao MD 30 Optimal use of Microscopy Gram stained preparations have to be observed with bright-field optics. Phase-contrast microscopy does not allow the recognition of true colours. Grampositive bacteria may be seen under phasecontrast as red cells. Using bright-field optics, Gram-positive cells are purple or blue and Gramnegative pink due to counter stain with Dr.T.V.Rao MD 31 safranin.. Use Bright field optics With bright-field optics colours can be discriminated best if the condenser iris is opened as far as possible without discomfort to the eyes Dr.T.V.Rao MD 32 Colors makes the Difference in Gram staining Bacteria that manage to keep the original purple dye have only got a cell wall - they are called Gram positive. Bacteria that lose the original purple dye and can therefore take up the second red dye have got both a cell wall and a cell membrane - they are called Gram negative. Dr.T.V.Rao MD 33 Observe with Caution to differentiate Dr.T.V.Rao MD 34 Report as follows If no microorganisms are seen in a smear of a clinical specimen, report “No microorganisms seen.” ii. If microorganisms are seen, report relative numbers and Describe morphology. Observe predominant shapes of microorganisms Dr.T.V.Rao MD 35 Gram Stain Differentiates Gram positive from Gram negative Differential Stains: Gram Stain Dr.T.V.Rao MD 36 Nature of Morphology in guides early Diagnosis in uncommon diseases Dr.T.V.Rao MD 37 Creating Library of Gram Stains Drain or gently blot excess oil For slide libraries and teaching collections that will be stored for longer periods, immersion oil can be removed with xylene solution and the slides can be cover slipped using Per mount to prevent fading. Dr.T.V.Rao MD 38 Value of Direct Smears Guide the physician on initial choice of antibiotic, pending results of culture and sensitivity. Judge specimen quality. Contribute to selection of culture media, especially with mixed flora. Provide internal quality control when direct smear results are compared to culture results. Dr.T.V.Rao MD 39 Mixed Flora of Staphylococcus and Streptococcus differentiates morphology Dr.T.V.Rao MD 40 Stains Several Fungi Dr.T.V.Rao MD 41 Gram-negative Pseudomonas aeruginosa bacteria (pink-rods). Dr.T.V.Rao MD 42 (Bacillus anthracis), Dr.T.V.Rao MD 43 Streptococcus pneumonia Dr.T.V.Rao MD 44 Streptococcus salivarius Dr.T.V.Rao MD 45 Gram stain of Neisseria gonorrhoea, Dr.T.V.Rao MD 46 Streptococcus pneumoniae in Sputum Dr.T.V.Rao MD 47 Clostridium spp as seen in Gram Stain Dr.T.V.Rao MD 48 Moraxella as seen in Gram Staining Dr.T.V.Rao MD 49 Clostridium difficile as seen by Gram staining Dr.T.V.Rao MD 50 Corynebacterium diptheria as seen in Gram staining Dr.T.V.Rao MD 51 Gram stain of Neisseria gonorrhoea, Dr.T.V.Rao MD 52 Neisseria meningitides as seen in Gram staining Dr.T.V.Rao MD 53 Nocardia spp seen in Gram Staining Dr.T.V.Rao MD 54 Gram Stained Actinomyctes spp Dr.T.V.Rao MD 55 Gram stained Listeria Monocytogenes Dr.T.V.Rao MD 56 Gram Stained Cryptococcus neoformans Dr.T.V.Rao MD 57 Artifacts in Gram Staining Gram stain reagents (Crystal Violet, Iodine, Safranin and Neutral Red Dirty glass slides Contaminated water used to rinse slides When investigating non-viable organisms seen in Gram stains it is always wise to eliminate every potential source. Dr.T.V.Rao MD 58 Gram’s method stains Artificacts too Dr.T.V.Rao MD 59 Gram stain results may not correlated with culture results Gram stain-positive, culture-negative specimens may be the result of contamination of reagents and other supplies, presence of Antimicrobial agents, or failure of organisms to grow under usual Culture conditions (media, atmosphere, etc.) Presence of anaerobic microorganism Dr.T.V.Rao MD 60 Common errors in Staining procedure Excessive heat during fixation Low concentration of crystal violet Excessive washing between steps Insufficient iodine exposure Prolonged decolourization Dr.T.V.Rao MD Excessive counterstaining 61 Correlation of Gram stain with cultures Culture results are not correlated with direct gram stain results. Select true or false 1 True ( Correct ) 2 False Dr.T.V.Rao MD 62 Gram staining not a fool proof procedure Dr.T.V.Rao MD Gram’s staining method is not without its problems. It is , complicated, and prone to operator error. The method also requires a large number of cells However, it is also central to phenotypic microbial identification techniques. 63 Gram variable observations in Gram staining The Gram staining procedure does not always give clear-cut results. Some organisms are Gram-variable and may appear either Gram-negative or Grampositive according to the conditions. With these types of organisms, Gram-positive and Gram-negative cells may be present within the same preparation Dr.T.V.Rao MD 64 Overcoming in Gram Variable Observations it is necessary that it is stained at two or three different ages (very young cultures should be used). If an organism changes from positive to negative or vice versa during its growth cycle, this change should be recorded with a statement as to the age of the culture when the change was first observed. In case a Gram-variable reaction is observed it is also good to check the purity of the culture. Dr.T.V.Rao MD 65 Why Gram Variability? Some Gram-positive bacteria appear Gram-negative when they have reached a certain age, varying from a few hours to a few days. On the other hand, some Gramnegative bacteria may become Grampositive in older cultures. For this reason it is strongly recommended to use very young cultures for the staining procedure, after growth has become just visible. Dr.T.V.Rao MD 66 Trouble shooting in Gram Staining method It is important to note that gram-positivity (the ability to retain the purple crystal violet-iodine complex) is not an all-or-nothing phenomenon but a matter of degree. There are several factors which could result in a gram-positive organism staining gram-negatively 1. The method and techniques used. Overheating during heat fixation, over decolourization with alcohol, and even too much washing with water between steps may result in gram-positive bacteria losing the crystal violet-iodine complex. Dr.T.V.Rao MD 67 Trouble shooting in Gram Staining method 2. The age of the culture. Cultures more than 24 hours old may lose their ability to retain the crystal violet-iodine complex. 3. The organism itself. Some gram-positive bacteria are more able to retain the crystal violet-iodine complex than others. One must use very precise techniques in gram staining and interpret the results with discretion Dr.T.V.Rao MD 68 Poor quality of slides Can be corrected Use of glass slides that have not been pre cleaned or degreased NOTE: Storing slides in a jar with 95% ethanol will ensure clean slides. Drain excess alcohol or flame slide before use. Dr.T.V.Rao MD 69 Modification in Gram staining methods ? Since the original procedure of Gram, many variations of the Gram staining technique have been published. Some of them have improved the method, others include some minor technical variants of no value. Bartholomew (1962) has pointed out that each variation in the Gram staining procedure has a definite limit to its acceptability. Any final result is the outcome of the interaction of all of the possible variables. All modified methods to be practised with caution should suit to the laboratory, and quality control checks. Dr.T.V.Rao MD 70 Gram staining continues to be Most Rapid test. Even new molecular methodologies typically take hours rather than minutes. Fortunately, Gram's stain, devised by a Danish pathologist in 1884, exists (see "The man behind Gram's stain, and "A revolution in staining begins," This simple staining procedure remains the most useful test performed in the microbiology lab. Results from a Gram's stain can tell volumes about an infection within 15 minutes of a specimen's arrival in the lab, while most other microbiology results require 24 hours or more. Nevertheless, Gram's stain findings can be equivocal and, therefore, must be assessed carefully in light of the clinical picture. Dr.T.V.Rao MD 71 Created for ‘e’ learning to Medical and Paramedical students in developing countreis Dr.T.V.Rao MD Email doctortvrao@gmail.com Dr.T.V.Rao MD 72