Dosering av trombocytt- og erytrocyttkonsentrater
Dosering av trombocytt- og erytrocyttkonsentrater- tid for nytenkning ?
Tor Hervig
Avdeling for immunologi og transfusjonsmedisin, Haukeland universitetssykehus
Disposisjon
1. Innledning
2. Dosering av trombocyttkonsentrater
3. Dosering av erytrocyttkonsentrater
4. Oppsummering
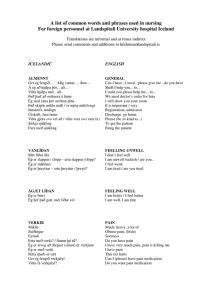
(Ola var fra Sandefjord: “Det gikk på engelsk og norsk, engelsk og norsk)
Vi vil hjelpe pasientene!
• Hva er et trombocyttkonsentrat?
• Hva er et erytrocyttkonsentrat?
• Hva er en pasient?
• Til barn: Dosering ml/kg, men en enhet
SAG-erytrocyttkonsentrat kan ha 40-70g hemoglobin
Hva trenger pasientene ?
• Erytrocyttkonsentrat
Oksygen til vevene
Celler til å presse trombocyttene mot karveggen
Hva er ønsket hb etter transfusjon?
• Trombocyttkonsentrat
Stoppe blødning
Forhindre blødning
Trombocyttransfusjoner
• Profylaktisk transfusjon?
• “On demand” transfusjon?
To store randomiserte studier pågår
Andreas Greinacher, personlig meddelelse
A randomized controlled trial comparing standard- and low-dose strategies for transfusion of platelets (SToP) to patients with thrombocytopenia
Nancy M. Heddle, Richard J. Cook, Alan Tinmouth, C. Tom Kouroukis, Tor
Hervig, Ellen Klapper, Joseph M. Brandwein, Zbigniew M. Szczepiorkowski,
James P. AuBuchon, Rebecca L. Barty, and Ker-Ai Lee, for the SToP Study investigators of the BEST Collaborative
Blood, 2009
• Lav: 2,4 x 10 11
Platedose
• Middels/standard: 4,8 x 10 11
• Høy: 7,2 x 10 11
WHO blødningsskala
• Grad 1: Hudblødning, kortvarig neseblødning
• Grad 2: Hematom, langvarig neseblødning, melena, hematemese, blødning fra stikksted (trenger ikke transfusjon)
• Grad 3: Som grad 2, men trenger transfusjon
• Grad 4: Livstruende/dødelig blødning
Mye større, amerikansk, trearmet studie
• Sherril Sclichter et al: Foreløpige data:
Ingen significant forskjell mellom blødningsfrekvens hos pasienter i de tre armene
Foreløpig konklusjon
• Ikke grunnlag for å endre norsk praksis
• Transfusjon ved blødning???
OPTIMIZING STANDARDS FOR
TRANSFUSION OF RED BLOOD CELL
CONCENTRATE
Håkon Reikvam and Tor Hervig
Haukeland University hospital and University of
Bergen, Norway
Chris Prowse, Products and Components R&D
Group, National Science Laboratory, SNBTS,
Edinburgh, UK
Nancy M. Heddle, Department of Medicine,
McMaster University, Hamilton, ON, Canada
OPTIMIZING STANDARDS FOR
TRANSFUSION OF RED BLOOD CELL
CONCENTRATE
• An important approach to the goal of reducing number of transfusions, is to give each patient the most exact hemoglobin
(Hb) dosage which is needed to achieve the wanted post-transfusion Hb.
• The rule of thumb used in the clinical practice:
• 1 unit of red blood cells transfused to an adult increases hemoglobin concentration with 1 g/dl
• Unfortunately, the Hb content of the units does not represent a homogeneity.
• The blood volumes of the patients vary significantly
Today situation
Figure 1 A
12.5
11.5
10.5
9.5
8.5
7.5
Hb before Hb after
Ideal situation
Figure 1 B
12.5
11.5
10.5
9.5
8.5
7.5
Hb before Hb after
Methods
• Two different concepts are proposed to overcome this challenges:
1)Standardize the units.
2)Adjust the Hb dose according to the patient’s blood volume; Hemoglobin dosing.
STANDARIZATION OF THE UNITS
• The term “unit” is derived from the time when “one unit of whole blood” referred to the source, i.e. a whole blood donation
Standardization of the red cell product
• The advantage of a standardized red cell product lies in the greater degree of predictability of clinical outcome for any predefined recipient.
• This could result in an alteration in physician’s prescribing practices, avoiding over-transfusion, especially in low volume recipients.
• The current situation where red cell products are prescribed in non-standard 'units' is outdated and unscientific.
Sweeney JD: Standardization of the red cell product .
Transfus Apher Sci 2006, 34 (2):213-218.
Hemoglobin dosing
• As high as a 50-percent difference in Hb content can be encountered between two units (40-60g)
• Indicating that RBC transfusions should be based on Hb content of the products instead of units.
• Gorlin J, Cable R: What is a unit? Transfusion 2000, 40 :263-265.
• Matching the Hb dose to the individual needs of the patients reduced the total usage of red cell concentrates by approximately 30 % in a study from Turkey.
• Calculating the patients’ total need of Hb to achieve the targeted Hb made this possibly.
• The total amount of transfused RBCc was reduced to 72 from the original 104 units required (ca 30%).
• The success rate was closely linked to patients’ weight; increased weight correlated with failure to comply with the goal.
Arslan O, Toprak S, Arat M, Kayalak Y: Hb content-based transfusion policy successfully reduces the number of RBC units transfused . Transfusion 2004,
44 (4):485-488.
Pilot study
• Bergen, Norway
• Hamilton, Canada
• Edinburgh, UK
Pilot study
• Hemodynamically stable patients needing
“pop-up” transfusions
• Measure hemoglobin content in red cell concentrates
• Measure height and weight of patients -> calculate blood volume
• Record pre- and post transfusion hemoglobin concentration
Goals
• To evaluate feasibility (practicability) of such procedures
• To evaluate if there is correlation between hemoglobin transfused and hemoglobin increment in patients – per litre of estimated blood volume
Body surface (BSA)
• Body surface was calculated by method described by DuBois
• BSA (m2) = Weight (kg)0.425 x Height
(cm)0.725 x 0.007184
Blood volume – alternative (BV)
• Males
• BSA x3.29-1.229
• Females
• BSA x3.47-1.954
• 50 patients were included in the study
• Total number of 52 transfusions episodes: -27 for women, 25 for men
Height, cm
Weight, kg
Body surface area, m
2
Blood volume, l
Number of units, n
Haemoglobin transfused, g
Pretransfusion
Hb, g/dl
Postransfusion
Hb, g/dl
Hb increment, g/dl
Total haemoglobin/ estimated blood volume, g/l
Mean
168.3
73.4
1.82
4.55
2.19
109.8
8.32
9.94
1.62
25.0
SD
10.97
17.6
0.23
0.91
0.44
26.75
1.05
1.17
0.73
1.03
Min
148.0
42.0
1.39
2.88
2
81.9
6.7
7.6
0.6
15.7
Max
192.0
129.0
2.34
6.40
4
204.0
10.6
12.8
4.6
49.6
61
58
55
52
49
46
43
40
37
70
67
64
114 units
Hb content in the unit
Resultater
• Videre resultater kan ikke legges ut pga rettigheter til artikkel under vurdering.
• Det var signifikant samnmenheng mellom hb dose gitt og hb stigning korrigert for kroppsvolum. Dette gir grunnlag for videre arbeid.
Discussion
• Feasibility
• Hemoglobin measurements were not causing a lot of extra work
• In the laboratory: Sterile docking of sample bag; transfer to test tube, hemoglobin measurement
Simplification
• By just measuring the weight of each unit, correlation and calculation of the actually
Hb content in each unit can easily be done.
•Allow the blood banks to use high-Hb-content units rationally by using an in-house blood-banking software.
•Adopting a policy of transfusing RBC in single-unit, instead of the standard two units.
•Alter the physicians prescribing practice and stimulate to increased cooperation with the blood bank.
•Avoiding potential both over-transfusion (in low weight patient) and under-transfusion (in high weight patient).
•Potential of reducing iron overload for patients depending on multiple transfusions.
• By just measuring the weight of each unit, correlation and calculation of the actually
Hb content in each unit can easily be done.
How to go on?
• Planning a large randomized study on hemoglobin increment after red cell transfusion in Bergen (NORWAY?)
• Using the method of :
• Targeting hemoglobin concentration after transfusion.
• Measuring the weight of each unit
That about qualitative aspects?
Koch CG, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J
Med. 2008;358:1229-1239.
Take home message
• Hemoglobin content in the units show great variability
• Blood volume in patients vary as well
• A hemoglobin increment lower than expectant does not necessary indicate active loss (bleeding, hemolytic reaction, etc.)
• Future aspects of more standardized procedures.
Hva skal vi gjøre?
• Tenke oss om
• Samtale med kliniske leger (og pasienter?)
• Gjennomføre en større studie med samme design?
• Ny, randomisert studie: Tilfeldige SAG mot utvalgte SAG?
• Hvem vil være med?
Oppsummering
• Platedose har neppe betydning for utfall hos pasienten
• Vi venter i spenning på kunnskap om forebyggende versus terapeutiske trombocyttransfusjoner
• Erytrocyttransfusjoner basert på “enhetstanken” gir vilkårlige konsekvenser for pasientene, på en eller annen måte må vi forbedre praksis: Til beste for pasient og blodbeholdning