ACCORD
advertisement

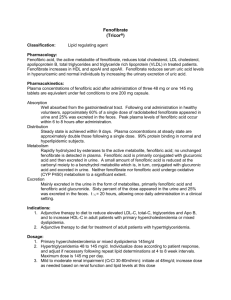
Henry C. Ginsberg, MD College of Physicians & Surgeons , Columbia University, New York For The ACCORD Study Group Dr. Ginsberg reports receiving ◦ Consulting fees from Merck, Merck Schering Plough, Bristol-Myers Squibb, AstraZeneca, Abbott, Roche, Isis/Genzyme, GlaxoSmithKline, Novartis, Pfizer, and Regeneron/ SanofiAventis. ◦ Grant support from Merck, ISIS/Genzyme, Roche, and AstraZeneca. ACCORD Study Design • Designed to independently test three medical strategies to reduce cardiovascular disease in diabetic patients • Lipid Trial question: whether combination therapy with a statin plus a fibrate would reduce cardiovascular disease compared to statin monotherapy in people with type 2 diabetes mellitus at high risk for cardiovascular disease. • Randomized, placebo-controlled, double-blind clinical trial conducted in 77 clinical sites in the U.S. and Canada ACCORD Study Design • Overall ACCORD Glycemia Trial: 10,251 participants • Lipid Trial: 5,518 in Lipid Trial • 2765 randomized to fenofibrate • 2753 randomized to placebo • Primary Outcome: First occurrence of a major cardiovascular event (nonfatal MI, nonfatal stroke, cardiovascular death) • 87% power to detect a 20% reduction in event rate, assuming placebo rate of 2.4%/yr and 5.6 yrs follow-up in participants without events. ACCORD Lipid Trial Eligibility • Stable Type 2 Diabetes >3 months • HbA1c 7.5% to 11% • High risk of CVD events = clinical or subclinical disease or 2+ risk factors • Age (limited to <80 years after Vanguard) • • ≥ 40 yrs with history of clinical CVD (secondary prevention) ≥ 55 yrs otherwise • Lipids • • • 60 < LDL-C < 180 mg/dl HDL-C < 55 mg/dl for women/Blacks; < 50 mg/dl otherwise Triglycerides < 750 mg/dl if on no therapy; < 400 mg/dl otherwise • No contraindication to either fenofibrate or simvastatin All participants on open-labeled simvastatin, 20 to 40 mg/day ◦ Simvastatin dose complied with lipid guidelines Patients randomized to double-blind placebo or fenofibrate, 54 to 160mg/day ◦ Dosing based upon eGFR level Only blinded ACCORD trial Observed Follow-up: 4 to 8 years (mean 4.7 years) Characteristic Mean or % Characteristic Mean or % Age (yrs) 62 Total Cholesterol (mg/dl) 175 Women % 31 LDL-C (mg/dl) 101 HDL-C (mg/dl) 38 162 Race / Ethnicity White % 68 Triglyceride (mg/dl)* Black % 15 Blood pressure (mm Hg) 134/74 Hispanic % 7 Serum creatinine (mg/dl) 0.9 Secondary prevent % 37 Current smoking % 15 DM duration (yrs)* 9 On a statin % 60 A1c (%) * 8.3 On another LLA % 8 BMI (kg/m2) 32 On Insulin % 33 * Median values Mean LDL-C 200 120 190 110 180 100 Feno 170 Placebo mg/dl mg/dl Mean Total Cholesterol 160 80 150 70 140 0 N = 5483 1 5180 2 3 4 5 6 7 4988 4783 5250 3377 1668 491 Feno 90 Placebo 60 Years PostRandomization 0 1 N = 5483 5180 3 4 5 6 4988 4783 5250 3377 1668 7 Years PostRandomization 491 Median Triglycerides 42 170 41 160 150 40 Feno Placebo 39 mg/dl mg/dl Mean HDL-C 2 Feno 140 Placebo 130 38 120 37 0 N = 5483 1 5180 2 3 4 5 6 4988 4783 5250 3377 1668 7 491 Years PostRandomization 110 0 N = 5432 1 2 3 4 5180 4988 4783 5250 5 3377 6 7 1668 491 Years PostRandomization Adverse Experiences During Follow-up Adverse events (no. (%)) Fenofibrate (N=2765) Placebo (N=2753) P value Out of the ordinary severe muscle aches/pains: regardless of CK plus CK > 5 X ULN plus CK > 10 X ULN 1110 (40.1%) 1115 (40.5%) 7 (0.3%) 8 (0.3%) 1 (0.04%) 2 (0.07%) 0.81 0.79 0.56 Any nonhypoglycemic SAE 54 (2.0%) 43 (1.6%) 0.27 Any Myopathy/Myositis/ Rhabdomyolysis SAE 4 (0.1%) 4 (0.1%) 1.00 Any Hepatitis SAE 3 (0.1%) 0 (0.0%) 0.18 Any SAE attributed to lipid meds 27 (1.0%) 19 (0.7%) 0.24 Lab Measures During Follow-up Fenofibrate (N=2765) Placebo (N=2753) P value ALT ever > 3X ULN 52 (1.9%) 40 (1.5%) 0.21 ALT ever > 5X ULN 16 (0.6%) 6 (0.2%) 0.03 CK ever > 5X ULN 51 (1.9%) 59 (2.2%) 0.43 CK ever > 10X ULN 10 (0.4%) 9 (0.3%) 0.83 Laboratory Measures (no. (%)) Lab Measures During Follow-up Fenofibrate (N=2765) Placebo (N=2753) P value ALT ever > 3X ULN 52 (1.9%) 40 (1.5%) 0.21 ALT ever > 5X ULN 16 (0.6%) 6 (0.2%) 0.03 CK ever > 5X ULN 51 (1.9%) 59 (2.2%) 0.43 CK ever > 10X ULN 10 (0.4%) 9 (0.3%) 0.83 235 (27.9%) 698 (36.7%) 157 (18.7%) 350 (18.5%) <0.001 <0.001 Laboratory Measures (no. (%)) Serum creatinine elevation Post-randomization incidence of microalbuminuria ( > 30 to < 300 mg/g*) 1050 (38.2%) 1137 (41.6%) 0.01 Post-randomization incidence of macroalbuminuria ( > 300 mg/g*) 289 (10.5%) 0.03 337 (12.3%) Primary Outcome Placebo (N=2753) Rate N of (%/yr) Events Primary Outcome: Major Fatal or Nonfatal Cardiovascular Event 310 2.41 Primary Outcome Fenofibrate (N=2765) Rate N of (%/yr) Events Primary Outcome: Major Fatal or Nonfatal Cardiovascular Event 291 2.24 Placebo (N=2753) Rate N of (%/yr) Events 310 2.41 Primary Outcome Fenofibrate (N=2765) Rate N of (%/yr) Events Primary Outcome: Major Fatal or Nonfatal Cardiovascular Event 291 2.24 Placebo (N=2753) Rate N of (%/yr) Events 310 2.41 HR (95% CI) P Value 0.92 0.32 (0.79 - 1.08) Prespecified Secondary Outcomes Fenofibrate (N=2765) N of Rate Events (%/yr) Placebo (N=2753) N of Rate Events (%/yr) HR (95% CI) P Value Outcome Primary + Revasc + hospitalized CHF 641 5.35 667 5.64 0.94 (0.85-1.05) 0.30 Major Coronary Event 332 2.58 353 2.79 0.92 (0.79-1.07) 0.26 Nonfatal MI 173 1.32 186 1.44 0.91 (0.74 - 1.12) 0.39 Total Stroke 51 0.38 48 0.36 1.05 (0.71 - 1.56) 0.80 Nonfatal Stroke 47 0.35 40 0.30 1.17 (0.76 - 1.78) 0.48 Total Mortality 203 1.47 221 1.61 0.91 (0.75 - 1.10) 0.33 Cardiovascular Death 99 0.72 114 0.83 0.86 (0.66 - 1.12) 0.26 Fatal/Nonfatal CHF 120 0.90 143 1.09 0.82 (0.65 - 1.05) 0.10 Primary Outcome By Treatment Group and Baseline Subgroups Primary Outcome By Treatment Group and Baseline Subgroups Trial (Drug) HHS (Gemfibrozil) BIP (Bezafibrate) FIELD (Fenofibrate) ACCORD (Fenofibrate) Primary Endpoint: Entire Cohort (P-value) -34% (0.02) Lipid Subgroup Criterion TG > 200 mg/dl LDL-C/HDL-C > 5.0 Primary Endpoint: Subgroup -71% TG > 200 mg/dl -7.3% (0.24) -11% -8% (0.16) (0.32) -39.5% TG > 204 mg/dl HDL-C < 42 mg/dl -27% TG > 204 mg/dl HDL-C < 34 mg/dl -31% Conclusion (1) • ACCORD Lipid does not support use of the combination of fenofibrate and simvastatin compared to simvastatin alone to reduce CVD events in the majority of patients with T2DM who have HDLC and TG levels that are close to the normal range Conclusion (2) • Subgroup analyses suggesting heterogeneity in response to combination therapy by gender and by the presence of significant dyslipidemia require further investigation