2.3 mmol/L
advertisement

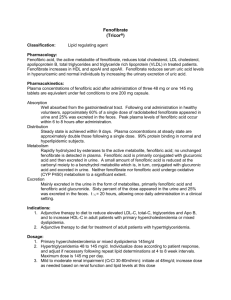
FIELD New results Aims of the FIELD eye study A. “FIELD sub-analysis”; To analyse the reasons for reduction in laser therapy in FIELD B. “Ophthalmology sub-study”; To assess the effect of fenofibrate on the progression of diabetic retinopathy in a sub-group of FIELD patients FIELD Study Investigators. The Lancet. 2007 First course of laser therapy -31% •Rapid benefits of fenofibrate were seen from eight months onward and increased throughout the study period •These benefits were additive to tight blood pressure and glycaemic control FIELD Study Investigators. The Lancet. 2007 The risk reduction was essentially due to macular oedema A significant 31% reduction due to macular oedema related laser treatment A significant 30% (p=0.015) reduction for proliferative retinopathy FIELD Study Investigators. The Lancet. 2007 Multiple courses of laser therapy Event 1 laser only Placebo Fenofibrate 121 85 95% CI P-value 0.63, 0.49-0.81, 0.0003 2-12 laser courses Hazard Ratio 37% reduction 117 70 Fenofibrate benefits patients from cumulative use of laser therapy The relative reduction seen with fenofibrate was significant in patients without prior retinopathy (49%, p=0.0002) Fenofibrate Favours fenofibrate FIELD Study Investigators. The Lancet. 2007 Summary Main study findings: -31% first laser overall p=0.0002 -31% for maculopathy p=0.002 -30% for proliferative retinopathy p=0.015 -37% total laser therapies p=0.0003 -49% all laser - primary p=0.0002 FIELD Eye Sub-study 1012 patients entered the ophthalmology sub-study 500 assigned to placebo 22 retinopathy history 478 no retinopathy history 512 assigned to fenofibrate 24 retinopathy history 488 no retinopathy history 19 deaths 16 deaths 57 sub-study followup not available 67 sub-study followup not available 3 withdrew consent 0 withdrew consent 421 assessed at end of study 429 assessed at end of study Sub-study main endpoint Development of retinopathy defined as at least a 2-step increase in the ETDRS grade after 2 or more years of follow-up for all patients. Also sub classified as: Primary prevention: 2-step progression to retinopathy in those with a baseline grade of 15 or less. Secondary prevention: 2-step progression of existing retinopathy in those with a baseline grade of 20 or greater Sub-study composite endpoint Exploratory combined outcome characterizing significant retinal pathology, composed of: 2-step progression of retinopathy grade development of macular oedema or laser therapy 2-step progression of retinopathy grade (ETDRS) and macular oedema Group Placebo Fenofibrate p value 57 46 0.19 (12.3%) (9.6%) 43 43 (11.7%) (11.4%) 14 3 (14.6%) (3.1%) 10 4 (2.2%) (0.8%) All patients No prior retinopathy Prior retinopathy* Macular oedema *79% reduction 0.87 0.004 0.09 Exploratory composite endpoint: laser therapy 2-step progression of retinopathy grade macular oedema Event Composite Endpoint* Placebo Fenofibrate 75 *34% reduction 53 Hazard Ratio 95% CI p-value 0.66 0.47-0.94 0.022 Summary Sub-study findings: -79% first laser therapy p=0.0004 -79% 2-step progression, p=0.004 (existing retinopathy) -64% macular oedema p=0.09 -34% combined end-point p=0.022 (laser, macular oedema, 2-step progression) Clinical Application - 5 years treatment with fenofibrate With pre-existing retinopathy Avoid first laser: NNT = 17 16 fewer multiple laser events per 100 Rx Without known prior eye disease Avoid first laser: NNT = 90 2.8 fewer multiple laser events per 100 Rx Conclusions In all subjects with diabetes, the use of fenofibrate could be considered for both its macro- and microvascular benefits Even for subjects on statin therapy at target LDL-C, fenofibrate could be considered as addon therapy to further attenuate residual diabetes-mediated risk and its microvascular complications (ACCORD study will provide further evidence for combination statin-fenofibrate therapy) Other tertiary outcomes Hospitalisations for angina pectoris1 Amputations2 RR = 0.82 (95% CI = 0.69-0.99) RR = 0.62 (95% CI = 0.43-0.90) p=0.038 p=0.011 Number of hospitalisations 252 200 5.1% 100 -18% 208 4.3% 100 0 Number of amputations 300 75 73 1.5% 50 -38% 45 1.0% 25 0 Placebo Fenofibrate Placebo Fenofibrate 1. FIELD study investigators. Atherosclerosis, Abstract We-S15: 2 Atherosclerosis in Supplement 2006; 7(3): 342 2. FIELD study investigators. Oral communication-AHA, 2007. Silent MI On-study myocardial infarction (9795 subjects with T2DM) None Silent Clinical Total MI = 640 = 6.5% 245 395 Clinical MI = 395 = 4.0% Silent MI = 245 = 2.5% 9155 Silent MI = 40% of all MIs Conclusions Silent MI is common in individuals with type 2 diabetes - almost 40% of all MI There were 16% fewer first silent MI events on fenofibrate (p = 0.154) Fenofibrate significantly reduced the occurrence all MI events by 20% (95% CI 631%, p=0.006) After silent MI, fenofibrate reduced the risk of further clinical CVD events (p=0.008) Dyslipidaemia CVD Event Rate Reductions for Dyslipidemia (HDL-C criteria for Metabolic Syndrome) Placebo (%) Fenofibrate (%) HR (95% CI) HR P TG 2.3 mmol/L 17.2 13.4 0.76 Low HDL-C* 15.1 13.0 0.85 0.020 13.5 0.74 0.007 0.007 Triglyceride 2.3 mmol/L plus low HDL-C 17.8 *M<1.03 mmol/L; F<1.29 mmol/L 0.5 0.6 0.7 0.8 0.9 1.0 CVD Event Rate Reductions for Dyslipidemia (HDL-C criteria for Metabolic Syndrome) Dyslipidaemic criteria Hazard Ratio (NNT) Event rate Event Rate Placebo Placebo Triglyceride criteria ( 2.3 mmol/L) 0.76 (26.3) (17.2) (13.4) Low HDL-C* 0.85 (47.6) (15.1) (13.0) TG 2.3 mmol/L plus low HDL-C 0.74 (23.3) (17.8) (13.5) *M<1.03 mmol/L; F<1.29 mmol/L CVD Event Rate Reductions for Dyslipidemia (High TG and/or low HDL-C as defined by NCEP-ATP III) Placebo (%) Fenofibrate (%) HR (95% CI) HR P Triglyceride criteria ( 2.3 mmol/L) 17.2 13.4 0.76 18.1 15.3 0.84 0.031 15.0 0.74 0.014 0.007 HDL-C < 1 mmol/L both genders Triglyceride 2.3 mmol/L plus HDL-C < 1 mmol/L 19.8 0.5 0.6 0.7 0.8 0.9 1.0 CVD Event Rate Reductions for Dyslipidemia (High TG and/or low HDL-C as defined by NCEP-ATP III) Dyslipidaemic criteria Hazard Ratio (NNT) Event rate Event Rate Placebo Placebo Triglyceride criteria ( 2.3 mmol/L) 0.76 (26.3) (17.2) (13.4) HDL-C < 1 mmol/L both genders 0.84 (37.0) (18.1) (15.3) Triglyceride 2.3 mmol/L plus HDLc < 1 mmol/L 0.74 (20.8) (19.8) (15.0) LIPANTHYL Lipanthyl snížil výskyt kardiovaskulárních příhod o 26 % u pacientů s dyslipidémii typickou pro DM typu 2 Právě pacienti s diabetem mellitem 2. typu nebo metabolickým syndromem profi tují nejvíce z léčby Lipanthylem A.. Keech: Features of Metabolic Syndrome Identify Individuals with Type 2 Diabetes Mellitus at high risk for CV events and greater benefits of fenofibrate. AHA 2007, Orlando, Abstract LIPANTHYL Mikrovaskulární efekty a úloha fenofibrátu p=0.0002 31% Retinopatie Albuminurie p=0,002 14% p=0,001 Amputace 0 5 10 15 20 25 30 38% 35 Redukce rizika (%) Lipanthyl je jediné hypolipidemikum s prokázanou účinnost na makro a zároveň mikrovaskulární komplikace DM Lancet 2007, AHA 2007 abstract