Chapter 26b
Reproduction
and Development
Male Reproductive Structures
• External genitalia
• Penis and scrotum
• Common passageway
• Urethra
• Accessory glands and ducts
• Prostate gland
• Seminal vesicle
• Bulbourethral gland
Male Reproductive Structures - Overview
Figure 26-8 (1 of 2)
Male Reproductive Structures - Erectile Tissues
Figure 26-8 (2 of 2)
Male Reproductive Structures
• Testes (sperm production)
• Seminiferous tubules
• Epididymis (sperm maturation)
• Vas deferens (aka “ductus deferens”, a
passageway into abdomen and delivery to
the urethra)
Male Reproductive Structures - Sagittal View
ANATOMY SUMMARY
THE MALE REPRODUCTIVE SYSTEM
Ureter
Urinary
bladder
Seminal
vesicle
Rectum
Prostate
gland
Bulbourethral
gland
Pubic
symphysis
Vas deferens
Ejaculatory
duct
Urethra
Penis
Epididymis
Testis
Scrotum
(a)
Figure 26-9a
Male Reproductive Structures - Scrotal Structures
ANATOMY SUMMARY
THE MALE REPRODUCTIVE SYSTEM
Head of
epididymis
Seminiferous
tubule
Epididymis
Vas deferens
(b)
Scrotal cavity
Figure 26-9b
Seminiferous Tubule - Cross-Section
ANATOMY SUMMARY
THE MALE REPRODUCTIVE SYSTEM
Capillary
Sertoli cell
Leydig cell
Spermatogonium
(c)
Figure 26-9c
Spermatogenesis in the Testes
• Seminiferous tubules
• Sertoli cells surround and support developing
sperm
• Spermatogonia divide and produce all sperm
cells
• Primary and secondary spermatocytes
• Spermatids
• Spermatozoa
• Interstitial tissues support spermatogenesis
• Leydig cells testosterone
• Capillaries deliver nutrients and remove wastes
Seminiferous Tubule - Detail
ANATOMY SUMMARY
THE MALE REPRODUCTIVE SYSTEM
Lumen of
seminiferous tubule
Spermatids
Secondary spermatocyte
Primary spermatocyte
Spermatogonium
Tight junction
between Sertoli cells
Fibroblast
(d)
Spermatozoa
Sertoli cells
Basal
lamina
Capillary
Leydig
cells
Figure 26-9d
Spermatozoa Structure
Head
Acrosome
contains
enzymes
Mid piece
Nucleus
Centrioles
Mitochondrial
spiral
Tail
(flagellum)
Microtubules
Figure 26-10
Regulation of Spermatogenesis
• Hormones control the production of sperm
• GnRH stimulates the release of LH and FSH
• LH Leydig cells testosterone
• FSH Sertoli cells cell products
Regulation of Spermatogenesis
GnRH
Hypothalamus
Anterior
pituitary
FSH
LH
Leydig
cells
Spermatogonium
Inhibin
Testes
Sertoli
cell
Testosterone (T)
Spermatocyte
Second
messenger
Sertoli
cell
To body
for secondary
effects
Cell
products
Androgen-binding
protein (ABP)
ABP
T
Figure 26-11
Accessory Glands Contribute to Semen
• Accessory glands contribute 99% of semen
volume, as well as the following
• Seminal vesicles – fructose, vitamin C,
prostaglandins
• Prostate gland – buffers, citric acid, enzymes
• Bulbourethral gland – mucus, buffers
Accessory Glands Contribute to Semen
Table 26-3
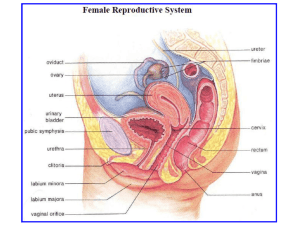
Female Reproductive System
• Female reproduction is a cyclic process
• Hormones from the hypothalamus and
anterior pituitary stimulate the ovaries
• The ovaries release estrogen and
progesterone in varying patterns during each
cycle
• Ovulation releases a mature oocyte monthly
• Estrogen and progesterone prepare the
uterus for possible pregnancy
Female Reproductive Structures
• External genitalia (aka vulva, or pudendum)
•
•
•
•
Labia majora
Labia minora
Clitoris
Vagina
• Hymen
• Urethral opening is inside the labia minora
Female Structures - External Genitalia
ANATOMY SUMMARY
THE FEMALE REPRODUCTIVE SYSTEM
Clitoris
Labium
minora
Urethral
opening
Labium
majora
Vagina
Hymen
(stretched)
Anus
(a)
Figure 26-12a
Female Structures - Internal Organs
• Vagina
• Uterus
• Cervix
• Endometrium and myometrium
• Fallopian tube
• Fimbriae
• Ovary
Female Structures - Sagittal View
ANATOMY SUMMARY
THE FEMALE REPRODUCTIVE SYSTEM
Ovary
Fallopian tube
Uterus
Urinary
bladder
Cervix
Rectum
Urethra
Vagina
Clitoris
(b)
Labium Labium
minora majora Anus
Figure 26-12b
Ovaries: Cells and Tissues
• Follicle - structure where oocytes develop
• Granulosa cells
• Oocyte
• Thecal cells surround all follicles
• Corpus luteum
Structure of the Uterus and Ovary
Figure 26-12c–e
Structure of the Uterine Wall
Figure 26-12c, f
Phases of the Ovarian Cycle
• Follicular phase
• Proliferation of granulosa cells
• Development of antrum
• Maturation of oocyte
• Ovulation
• Ripened follicle bursts, releasing oocyte
• Luteal phase
• Ruptured follicle develops into corpus luteum
The Ovarian Cycle
Figure 26-13 (1 of 2)
Endometrial Lining: the Uterine Cycle
• Menses (occurs if pregnancy is not achieved)
• Bleeding from uterus as endometrium is shed
• Proliferative phase
• Endometrium grows in preparation for
pregnancy
• Secretory phase
• Endometrial secretions promote implantation
The Uterine Cycle
Figure 26-13 (2 of 2)
Follicular Phase and Menses
Phases of the
Ovarian Cycle
Follicular Phase
Gonadotrophic
hormone
levels
FSH
LH
Ovarian
cycle
Primary
follicle
Ovarian
hormone
levels
Theca
Estrogen
Inhibin
Progesterone
Uterine
cycle
Phases of the
Uterine Cycle
MENSES
36.7
Basal body
temperature
(–C) 36.4
DAYS
28/0
7
14
21
28/0
Figure 26-13 (1 of 4)
Follicle Maturation and the Proliferative Phase
Phases of the
Ovarian Cycle
Follicular Phase
LH
Gonadotrophic
hormone
levels
FSH
Ovarian
cycle
Primary
follicle
Ovarian
hormone
levels
Theca Antrum
Estrogen
Inhibin
Progesterone
Uterine
cycle
Phases of the
Uterine Cycle
MENSES
PROLIFERATIVE
PHASE
36.7
Basal body
temperature
(–C) 36.4
DAYS
28/0
7
14
21
28/0
Figure 26-13 (2 of 4)
Ovulation, Luteal Phase, and Secretory Phase
Phases of the
Ovarian Cycle
Follicular Phase Ovulation
Luteal Phase
LH
Gonadotrophic
hormone
levels
FSH
Ovarian
cycle
Primary
follicle
Ovarian
hormone
levels
Corpus
Theca Antrum Ovulation luteum
formation
Estrogen
Inhibin
Progesterone
Uterine
cycle
Phases of the
Uterine Cycle
MENSES
PROLIFERATIVE
PHASE
SECRETORY PHASE
36.7
Basal body
temperature
(–C) 36.4
DAYS
28/0
7
14
21
28/0
Figure 26-13 (3 of 4)
Corpus Luteum Degenerates and Ceases Hormone
Production
Phases of the
Ovarian Cycle
Follicular Phase Ovulation
Luteal Phase
LH
Gonadotrophic
hormone
levels
FSH
Ovarian
cycle
Primary
follicle
Ovarian
hormone
levels
Corpus Mature
Corpus
Theca Antrum Ovulation luteum corpus albicans
formation luteum
Progesterone
Estrogen
Inhibin
Uterine
cycle
Phases of the
Uterine Cycle
MENSES
PROLIFERATIVE
PHASE
SECRETORY PHASE
36.7
Basal body
temperature
(–C) 36.4
DAYS
28/0
7
14
21
28/0
Figure 26-13 (4 of 4)
Complex Hormonal Control of Two Cycles
• Ovarian and uterine cycles are controlled by
several hormones, which display complex
interactions
• Extra-ovarian hormones
• GnRH from the hypothalamus
• FSH and LH from the anterior pituitary
• Ovarian hormones
• Estrogen
• Progesterone
Hormonal Control of the Menstrual Cycle
LH
FSH
Ovum
Follicle
Corpus luteum
Estrogen
Inhibin
Progesterone
GnRH
GnRH
GnRH
GnRH
Hypothalamus
Pituitary
Tonic secretion
resumes
FSH
FSH
LH
LH
Follicle
Follicle
Granulosa
cells
Granulosa
cells
Thecal
cells
Androgens
Estrogens
(a) Early to mid-follicular phase
Inhibin
High estrogen
output
FSH
LH
Corpus luteum
(from ovulated
follicle)
Thecal
cells
secretes
Androgens
Estrogen
Progesterone
Inhibin
FSH
New follicles
begin to
develop
LH
Corpus
luteum
dies
Estrogen and
progesterone
Small amount of
progesterone
(b) Late follicular phase and ovulation
(c) Early to mid-luteal phase
(d) Late luteal phase
Figure 26-14
Hormonal Control of the Menstrual Cycle: Follicular
Phase
• FSH stimulates follicular development
• Maturation to secondary and tertiary follicles
• Granulosa cells produce estrogen
• Negative feedback decreases FSH and LH
secretion
• Positive feedback allows continued estrogen
production
• LH stimulates thecal cells to produce
androgens
• Aromatase converts androgens into estrogens
• Antrum fills with fluid
Hormonal Control of the Menstrual Cycle: Follicular
Phase
LH
FSH
Ovum
Follicle
Corpus luteum
Estrogen
Inhibin
Progesterone
GnRH
Hypothalamus
Pituitary
FSH
LH
Follicle
Granulosa
cells
Thecal
cells
Androgens
Estrogens
(a) Early to mid-follicular phase
Figure 26-14 (1 of 4)
Hormonal Control of the Menstrual Cycle: Late
Follicular Phase and Ovulation
• Late follicular phase
• Secretion of inhibin and progesterone begins
• Estrogen changes from negative to positive
feedback
• Enhanced secretion of LH - the LH surge
• Meiosis resumes in developing follicles
• Ovulation
•
•
•
•
Mature follicle secretes collagenase
Inflammatory reaction produces prostaglandins
Follicle ruptures releasing mature oocyte
Theca and granulosa cells change into luteal
cells
Hormonal Control of the Menstrual Cycle: Late
Follicular Phase and Ovulation
LH
FSH
Ovum
Follicle
Corpus luteum
Estrogen
Inhibin
Progesterone
GnRH
GnRH
Hypothalamus
Pituitary
FSH
FSH
LH
LH
Follicle
Follicle
Granulosa
cells
Thecal
cells
Androgens
Estrogens
(a) Early to mid-follicular phase
Granulosa
cells
Inhibin
Thecal
cells
Androgens
High estrogen Small amount of
output
progesterone
(b) Late follicular phase and ovulation
Figure 26-14 (2 of 4)
Hormonal Control of the Menstrual Cycle: Early to
Mid-Luteal Phase
• Corpus luteum develops and secretes
progesterone and estrogen
• Progesterone and estrogen exert negative
feedback on hypothalamus
• Effects of progesterone
• Endometrium develops further
• Cervical mucus thickens
Hormonal Control of the Menstrual Cycle: Early to
Mid-Luteal Phase
LH
FSH
Ovum
Follicle
Corpus luteum
Estrogen
Inhibin
Progesterone
GnRH
GnRH
GnRH
Hypothalamus
Pituitary
FSH
FSH
LH
LH
Follicle
Follicle
Granulosa
cells
Thecal
cells
Androgens
Estrogens
(a) Early to mid-follicular phase
Granulosa
cells
Inhibin
FSH
LH
Corpus luteum
(from ovulated
follicle)
Thecal
cells
secretes
Androgens
Estrogen
Progesterone
Inhibin
High estrogen Small amount of
output
progesterone
(b) Late follicular phase and ovulation
(c) Early to mid-luteal phase
Figure 26-14 (3 of 4)
Hormonal Control of the Menstrual Cycle: Late
Luteal Phase
• If no implantation
• Corpus luteum undergoes apoptosis after 12
days
• Lack of progesterone leads to death of
endometrium
• Menses = sloughing of the dead endometrium
• FSH and LH secretion resumes
• Following implantation
• hcG maintains corpus luteum
• Corpus luteum secretes progesterone and
estrogen
Hormonal Control of the Menstrual Cycle: Late
Luteal Phase
LH
FSH
Ovum
Follicle
Corpus luteum
Estrogen
Inhibin
Progesterone
GnRH
GnRH
GnRH
GnRH
Hypothalamus
Pituitary
Tonic secretion
resumes
FSH
FSH
LH
LH
Follicle
Follicle
Granulosa
cells
Thecal
cells
Androgens
Estrogens
(a) Early to mid-follicular phase
Granulosa
cells
Inhibin
FSH
LH
Corpus luteum
(from ovulated
follicle)
Thecal
cells
secretes
Androgens
Estrogen
Progesterone
Inhibin
FSH
New follicles
begin to
develop
LH
Corpus
luteum
dies
Estrogen and
progesterone
High estrogen Small amount of
output
progesterone
(b) Late follicular phase and ovulation
(c) Early to mid-luteal phase
(d) Late luteal phase
Figure 26-14 (4 of 4)
Female Secondary Sex Characteristics
• Secondary sexual characteristics are traits,
other than genitalia, that distinguish males
from females
• Characteristics controlled by estrogen
• Breast development
• Distribution of body fat
• Adrenal androgens control some female traits
• Growth of pubic and axillary hair
• Sex drive (libido)