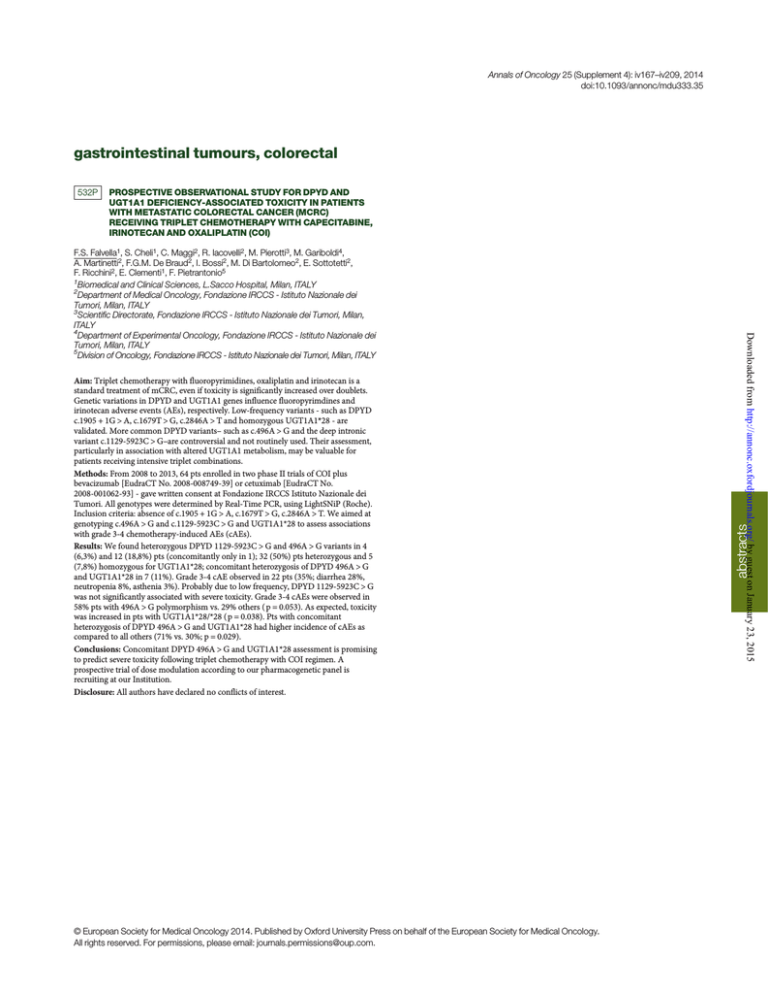
Annals of Oncology 25 (Supplement 4): iv167–iv209, 2014
doi:10.1093/annonc/mdu333.35
gastrointestinal tumours, colorectal
PROSPECTIVE OBSERVATIONAL STUDY FOR DPYD AND
UGT1A1 DEFICIENCY-ASSOCIATED TOXICITY IN PATIENTS
WITH METASTATIC COLORECTAL CANCER (MCRC)
RECEIVING TRIPLET CHEMOTHERAPY WITH CAPECITABINE,
IRINOTECAN AND OXALIPLATIN (COI)
Aim: Triplet chemotherapy with fluoropyrimidines, oxaliplatin and irinotecan is a
standard treatment of mCRC, even if toxicity is significantly increased over doublets.
Genetic variations in DPYD and UGT1A1 genes influence fluoropyrimdines and
irinotecan adverse events (AEs), respectively. Low-frequency variants - such as DPYD
c.1905 + 1G > A, c.1679T > G, c.2846A > T and homozygous UGT1A1*28 - are
validated. More common DPYD variants– such as c.496A > G and the deep intronic
variant c.1129-5923C > G–are controversial and not routinely used. Their assessment,
particularly in association with altered UGT1A1 metabolism, may be valuable for
patients receiving intensive triplet combinations.
Methods: From 2008 to 2013, 64 pts enrolled in two phase II trials of COI plus
bevacizumab [EudraCT No. 2008-008749-39] or cetuximab [EudraCT No.
2008-001062-93] - gave written consent at Fondazione IRCCS Istituto Nazionale dei
Tumori. All genotypes were determined by Real-Time PCR, using LightSNiP (Roche).
Inclusion criteria: absence of c.1905 + 1G > A, c.1679T > G, c.2846A > T. We aimed at
genotyping c.496A > G and c.1129-5923C > G and UGT1A1*28 to assess associations
with grade 3-4 chemotherapy-induced AEs (cAEs).
Results: We found heterozygous DPYD 1129-5923C > G and 496A > G variants in 4
(6,3%) and 12 (18,8%) pts (concomitantly only in 1); 32 (50%) pts heterozygous and 5
(7,8%) homozygous for UGT1A1*28; concomitant heterozygosis of DPYD 496A > G
and UGT1A1*28 in 7 (11%). Grade 3-4 cAE observed in 22 pts (35%; diarrhea 28%,
neutropenia 8%, asthenia 3%). Probably due to low frequency, DPYD 1129-5923C > G
was not significantly associated with severe toxicity. Grade 3-4 cAEs were observed in
58% pts with 496A > G polymorphism vs. 29% others ( p = 0.053). As expected, toxicity
was increased in pts with UGT1A1*28/*28 ( p = 0.038). Pts with concomitant
heterozygosis of DPYD 496A > G and UGT1A1*28 had higher incidence of cAEs as
compared to all others (71% vs. 30%; p = 0.029).
Conclusions: Concomitant DPYD 496A > G and UGT1A1*28 assessment is promising
to predict severe toxicity following triplet chemotherapy with COI regimen. A
prospective trial of dose modulation according to our pharmacogenetic panel is
recruiting at our Institution.
Disclosure: All authors have declared no conflicts of interest.
© European Society for Medical Oncology 2014. Published by Oxford University Press on behalf of the European Society for Medical Oncology.
All rights reserved. For permissions, please email: journals.permissions@oup.com.
Downloaded from http://annonc.oxfordjournals.org/ by guest on January 23, 2015
F.S. Falvella1, S. Cheli1, C. Maggi2, R. Iacovelli2, M. Pierotti3, M. Gariboldi4,
A. Martinetti2, F.G.M. De Braud2, I. Bossi2, M. Di Bartolomeo2, E. Sottotetti2,
F. Ricchini2, E. Clementi1, F. Pietrantonio5
1
Biomedical and Clinical Sciences, L.Sacco Hospital, Milan, ITALY
2
Department of Medical Oncology, Fondazione IRCCS - Istituto Nazionale dei
Tumori, Milan, ITALY
3
Scientific Directorate, Fondazione IRCCS - Istituto Nazionale dei Tumori, Milan,
ITALY
4
Department of Experimental Oncology, Fondazione IRCCS - Istituto Nazionale dei
Tumori, Milan, ITALY
5
Division of Oncology, Fondazione IRCCS - Istituto Nazionale dei Tumori, Milan, ITALY
abstracts
532P