Epilepsy and Autism-Dr. Stefanie Berry
advertisement

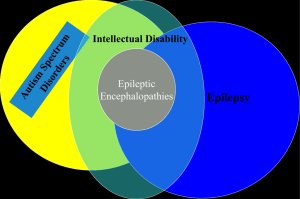
Epilepsy and Autism Stefanie Jean-Baptiste Berry, MD Pediatric Epileptologist Northeast Regional Epilepsy Group What is Autism? Impairment in social interaction Impairment in communication (verbal and nonverbal) Restricted, repetitive and stereotyped behavior, interests and activities Onset before 3 years of age Prevalence 60 in 10,000 children (0.6%) Prevalence 2-4 in 10,000 in 1970 Higher prevalence in males High genetic and metabolic contribution Possible environmental factors Concordance between monozygotic twins is about 70% 4.5% increased risk for recurrence in siblings Some genetic syndromes have a high association with autism (Angelman and Fragile X) Conditions Associated with Autism: Fragile X Tuberous Sclerosis Sotos Syndrome Mucopolysaccharidoses Toxic (Thalidomide, Alcohol, Cocaine) Natural history and outcome of autism is variable IQ less than 70 in most children with autism 1/3 with no communicative speech Most favorable outcome in those with normal/near normal intelligence and speak before age 5 Applied behavior analysis (ABA) improve chances of functioning independently Autism Spectrum Disorder Subtypes Autistic disorder Asperger’s syndrome Pervasive developmental disorder Childhood Disintegrative disorder Rett’s syndrome Classical Autistic Disorder 1. Impaired Sociability 2. Impaired verbal and non-verbal communication 3. Restricted activities and interests Asperger’s syndrome 1. Normal or near normal intelligence. 2. Language skills develop normally 3. Speech formal, peculiar voice, deviant prosody 4. Flat affect, insensitivity to social cues, and obsessively indulged interests 5. Male to female ratio 4:1 Childhood Disintegrative Disorder 1. Rare form of autism 2. Prevalence 1.7 per 100,000 2. Acquired between ages 2 and 6 after entirely normal early development 3. Profound regression over weeks to months in language, motor and social/adaptive skills Rett’s Syndrome 1. Incidence 1 in 10,000 to 15,000 2. X-linked, MeCP2 gene, majority of mutations de novo 3. Almost exclusively female 4. Postnatal brain growth affected (acquired microcephaly) Rett’s Syndrome 5. Developmental regression (normal development until 6-12 months) 6. Loss of purposeful hand movements 7. Severe mental retardation and motor deficits Pervasive Development Disorder 1. Milder communication, behavioral and social impairment 2. Later age of onset Epilepsy and Autism Prevalence of epilepsy among all children is 2-3% 5-38% frequency of epilepsy in autistic children 35-65% with EEG abnormalities Epilepsy in autism increased mortality Bimodal age distribution Peak infancy to age 5 years and adolescence Highest risk for epilepsy in those with severe mental retardation and cerebral palsy Epilepsy persists in the majority of patients into adult life (remission 16%) Autistic Disorder - Clinical epilepsy by adolescence in more than 1/3 of patients Asperger’s syndrome - Estimated 5-10% likelihood of developing epilepsy in early childhood Pervasive Developmental Disorder - Risk for epilepsy linked to underlying brain dysfunction Disintegrative Disorder - Risk for epilepsy as high as 70% Rett’s Syndrome – Risk for epilepsy is more than 90% Diagnosis complicated because seizures may be mistaken for behaviors (not responding to name) Unusual repetitive behaviors, common in autism, hard to distinguish from seizures All seizure types may be seen Prevalence of epilepsy and types of seizures vary Swedish study complex partial, atypical absence, myoclonic and tonic-clonic most common American study tonic-clonic and atypical absence most common Other studies state complex partial with centrotemporal spikes most common Some studies suggest that epileptiform discharges on EEG without seizures can cause behavioral and cognitive impairment Usually treat based on clinical seizures not just EEG findings. Should anti-epileptic medication be prescribed to children with autism, language regression and subclinical EEG abnormalities? Long-duration EEGs that include slow wave sleep more likely to show epileptiform abnormalities Long-duration EEG of children with autism spectrum disorder and regression without clinical seizures – 46% with epileptiform activity Focal spikes - Centrotemporal spikes and temporoparietal spikes Landau-Kleffner Syndrome Overlap with autistic regression Loss of language is prominent Language regression after age 3 Acquired aphasia associated with clinical seizures or an epileptiform EEG Clinical seizures not required for diagnosis No decline in sociability or repetitive behaviors EEG abnormalities (spikes, sharp waves and spike wave discharges); mainly over temporoparietal regions 25% do not have clinical seizures Loss of language attributed to clinical or subclinical epilepsy in cortical areas responsible for language Medical treatment of seizures in autism similar to treating other children with epilepsy Limited data on response of children with epileptiform EEG without clinical seizures Same strategy as LKS – reduce epileptiform activity Reports that language of LKS and those with autism improved in response to anticonvulsants Improvements have also been reported in patients treated with corticotropin, steroids, or immunoglobulins Clinical reports of the use of Depakote in children with autism with and without clinical seizures Most showed improvement in core symptoms of autism Absence of clinical trials, therefore no definite recommendations about treatment Surgical resection in children with autism and intractable epilepsy – may improve seizures +/- autistic symptoms 1 study subpial transections – language and behavior improved