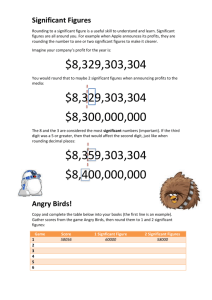
Intentional Rounding: Therapeutic Observations in Healthcare
advertisement
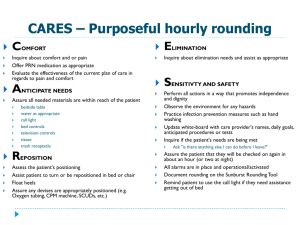
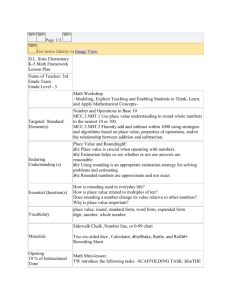
Intentional rounding with general therapeutic observations Michele Streatfield Lead Nurse, OPMHN & Specialist Services What is intentional rounding? It has also been called ‘comfort rounds’ or ‘care rounds’. It is where nurses ensure that the patient’s needs are met by observing and talking to them and asking if there is anything else they can do for the patient before moving away from them. It has been heavily promoted by David Cameron and the Nursing and Care Quality Forum from 2012, and is being implemented in nearly all hospitals. However…… or Cons This can be perceived as another top down exercise not relevant for mental health settings Not enough research in this area Focuses more on general hospital settings i.e. call bells, non ambulant patients Rounding is based in part on a study of 14 hospitals in the United States, it may not be applicable to UK hospitals because staffing levels here tend to be lower Pros Enables staff to focus general observations in a more structured way Not just a ‘head count’ A DoH spokesperson said rounding has reduced the number of patient complaints and significantly improved patient satisfaction levels Looks at the service user as a whole person Encourages interaction Promotes positive engagement and is more therapeutic General observations General observation is the minimum acceptable level of observation for all in-patients. The primary aim of observation should be to engage positively with the service user. This involves a two-way relationship, established between a service user and a staff member, which is meaningful, grounded in trust, and therapeutic for the service user. Nice (2005) General observations meets intentional rounding Implementation in practice Within the 1 hour time period, staff should introduce themselves and are advised to use the acronym ‘DONE’ as a prompt to positively engage with and assess each patient, which stands for: • Distress – How is the patient feeling? How is their mental state? Are there changes to risk? • Observations – How responsive are they? Are they socially isolating themselves? • Need – Are they hungry or thirsty? Are they comfortable? If relevant - Do they need assistance with toileting or repositioning if impaired mobility? Do they need a little reassurance? • Environment - Do they feel safe? Are there environmental risks? Do they want to leave? Adapted from Aneurin Bevan Health Board (2012) And finally….. The use of forms to capture this vital information An updated form was produced by some Ward Managers and their teams Discussed at the Modern Matron’s Forum Reviewing the policy using the PDSA cycle References • Snelling P (2013) Intentional rounding: a critique of the evidence. Nursing Times; 109: 20, 19-21 • National Institute for Clinical Excellence (NICE) (2005) “Violence: The short-term management of disturbed/violent behaviour in in-patient psychiatric settings and emergency departments”. London • Aneurin Bevan Health Board Newsletter (2012) • Kent and Medway NHS & Social Care Partnership Trust (2013) Therapeutic observation of patients policy