X-ray Beam Composition and Collimation
advertisement

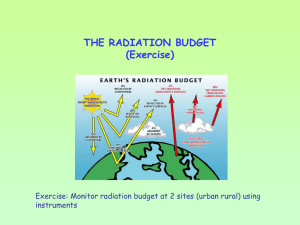
X-ray Beam Composition and Collimation By Professor Stelmark Leakage radiation is radiation generated in the x-ray tube that does not exit from the collimator opening but rather penetrates through the protective tube housing and to some degree through the sides of the collimator Protective housing covers the x-ray tube and provides the following three functions: It reduces leakage radiation to less than 100 mR/hr at 1 m. X-ray tubes are designed so that projectile electrons from the cathode interact with the target only at the focal spot. However, some of the electrons bounce off the focal spot and then land on other areas of the target, causing x-rays to be produced from outside of the focal spot. These x-rays are called off-focus radiation. This is not unlike squirting a water pistol at a concrete pavement: Some of the water splashes off the pavement and lands in a larger area. Extreme effect of off-focus radiation. You can see the image of the nose from the off-focus radiation Off focus radiation is undesirable because it extends the size of the focal spot. The additional x-ray beam area increases skin dose modestly but unnecessarily. Off focus radiation can significantly reduce image contrast. Finally, off focus radiation can image patient tissue that was intended to be excluded by the variable-aperture collimators. Examples of such undesirable images are the ears in a skull examination, the soft tissue beyond the cervical spine, and the lung beyond the borders of the thoracic spine. X-rays are carriers of manmade, electromagnetic energy. If x-rays enter a material such as human tissue, they may interact with the atoms of the biologic material in the patient or pass through without interaction. If they interact, electromagnetic energy is transferred from the x-rays to the atoms of the patient's biologic material. This transference of electromagnetic energy to the atoms of the material is called absorption Primary radiation emerges from the x-ray tube target and consists of x-ray photons of various energies. It is produced when the positively charged target is bombarded with a stream of high-speed electrons and these electrons interact with the atoms of the target. Although all photons in a diagnostic x-ray beam do not have the same energy, the most energetic photons in the beam can have no more energy than the electrons that bombard the target. The energy of the electrons inside the x-ray tube is expressed in terms of the electrical voltage applied across the tube. In diagnostic radiology, this is expressed in thousands of volts, or kilovolts (kV). Because the voltage across the tube fluctuates, it is usually expressed in kilovolt peak (kVp) The emerging x-ray photon beam is collectively referred to as primary radiation (primary signal DR) When an x-ray beam passes through a patient, it goes through a process called attenuation. Attenuation is simply the reduction in the number of primary photons in the x-ray beam through: • Absorption (a total loss of radiation energy) • Scatter (a change in direction of travel that may also involve a partial loss of radiation energy) as the beam passes through the patient in its path. Some primary x-ray photons will also traverse the patient without interacting. This may be called direct transmission. These non-interacting x-ray photons reach the radiographic image receptor (e.g., phosphor plate, digital radiography receptor or radiographic film). Other primary photons can undergo interactions and as a result may be scattered or deflected. Such photons may still traverse the patient and strike the image receptor. This process is called indirect transmission. The optimal x-ray image is formed when only direct transmission x-ray photons reach the image receptor. In clinical situations, scattered photons do reach the image receptor and degrade image quality. Before the four photons produced by the x-ray source enter human tissue, they are referred to as primary photons. Only two photons emerge from the tissue and strike the radiographic image receptor below it. They are referred to as exit or imageformation photons. The two that do not strike the image receptor are attenuated. Photon 4 seems to disappear. It has transferred all its energy to the atoms of the patient and has therefore been eliminated. Because a photon has no mass, it ceases to exist when it gives up its energy. Attenuation, then, refers to both absorption and scatter processes that prevent photons from reaching a predefined destination. Figure shows that the path of photon 2 was bent, but not so much that the photon missed its target. Because photon 2 reaches the image receptor, it is part of the exit, or image-formation, radiation, but the bending of its path represents what is called small-angle scatter. Scattered photons in this category have essentially the same energy as the incident photons. Small-angle scatter degrades the appearance of a completed radiographic image by blurring the sharp outlines of dense structures Differential absorption is the difference between the x-ray photons that are absorbed photoelectrically versus those that penetrate the body. A radiographic image is created by passing an x-ray beam through the patient and interacting with an image receptor, such as a film-screen or digital system. The variations in absorption and transmission of the exiting x-ray beam structurally represent the anatomic area of interest. When the attenuated x-ray beam leaves the patient, the remaining x-ray beam, referred to as exit radiation or remnant radiation, is composed of both transmitted and scattered radiation. The varying amounts of transmitted and absorbed radiation (differential absorption) create an image that structurally represents the anatomic area of interest. Scatter exit radiation that reaches the image receptor does not provide any diagnostic information about the anatomic area. Scatter radiation creates unwanted exposure on the image called fog. Components of Exit or Remnant Radiation • • • • • Off –focus radiation Scattered radiation Image forming radiation No-image forming radiation Directly transmitted radiation Secondary Radiation • Attenuated radiation (scattered photons) Because many billions of such scatter events occur, radiographic density of the image also increases overall, interfering with the radiologist's ability to distinguish different structures in the image. This undesirable, additional density is called radiographic fog. Reducing the amount of tissue irradiated reduces the amount of fog produced by small-angle scatter. Therefore, adequately collimating the x-ray beam is one way to reduce fog. Scatter Control Factors Affecting the Amount of Scatter Radiation The greater the volume of tissue irradiated because of part thickness or x-ray beam field size, the greater the amount of scatter radiation produced. The higher the kVp used, the greater the energy of scattered x-rays exiting the patient. Controlling the amount of scatter radiation produced in the patient and ultimately reaching the image receptor (IR) is essential in creating a diagnostic-quality image. Scatter radiation is detrimental to radiographic quality because it adds unwanted exposure (fog) to the image without adding any patient information. Digital IRs are more sensitive to lower energy levels of radiation such as scatter, which results in increased fog in the image. Additionally, scatter radiation decreases radiographic contrast for both film-screen and digital images. Increased scatter radiation either produced within the patient or higher-energy scatter exiting the patient affects the exposure to the patient and anyone within close proximity. Therefore the radiographer must act to minimize the amount of scatter radiation produced and reaching the IR. Beam Restriction It is up to each radiographer to limit the x-ray beam field size to the anatomic area of interest. Beam restriction serves two purposes: limiting patient exposure and reducing the amount of scatter radiation produced within the patient Collimation and Scatter Radiation As collimation increases, the field size decreases and the quantity of scatter radiation decreases; as collimation decreases, the field size increases and the quantity of scatter radiation increases. Collimators The most sophisticated, useful, and accepted beam-restricting device is the collimator. Collimators are considered the best beam-restricting device. A collimator has two or three sets of lead shutters. Located immediately below the tube window, the entrance shutters limit the x-ray beam much as the aperture diaphragm does. One or more sets of adjustable lead shutters are located 3 to 7 inches (8 − 18 cm) below the tube. These shutters consist of longitudinal and lateral leaves or blades, each with its own control. This makes the collimator adjustable in that it can produce projected fields of varying sizes. The field shape produced by a collimator is always rectangular or square. Automatic Collimators An automatic collimator, also called a positive beam-limiting (PBL) device, automatically limits the size and shape of the primary beam to the size and shape of the IR. For a number of years, automatic collimators were required by U.S. federal law on all new radiographic installations. This law has since been rescinded, and automatic collimators are no longer a requirement on any radiographic equipment. However, they are still widely used. Automatic collimators mechanically adjust the primary beam size and shape to that of the IR when the IR is placed in the Bucky tray, just below the tabletop. Automatic collimation makes it difficult for the radiographer to increase the size of the primary beam to a field larger than the IR, which would result in increasing the patient's radiation exposure. PBL devices were seen as a way of protecting patients from overexposure to radiation. However, it should be noted that automatic collimators have an override mechanism that allows the radiographer to disengage this feature. Restricting the Primary Beam Increased Factor Result Collimation Patient dose decreases. Scatter radiation decreases. Radiographic contrast increases. Film-screen: Radiographic density decreases. Digital: Quantum noise increases. Field Size Patient dose increases. Scatter radiation increases. Radiographic contrast decreases. Film-screen: Radiographic density increases. Digital: Quantum noise decreases. Collimation and Intensity 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR Collimation and Intensity 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR Collimation and Intensity 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR Collimation and Intensity 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR 2 mR