Vital Signs - Fog.ccsf.edu
advertisement

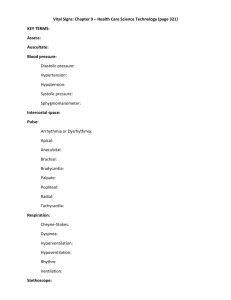
Vital Signs OBJECTIVES State the basic components of vital signs. List factors that can cause variations in vital signs. Define terminology related to vital signs. Identify the normal ranges of vital signs. Describe the protocol for reporting and recording vital signs. State the procedure for measuring height and weight in an adult. Vital Signs Temperature (T) Pulse (P) Respiration (R) Blood pressure (BP) Pain (often called the fifth vital sign) Factors which Causes Changes in Vital Signs 1. Temperature 2. Physical Exertion 3. Effect of Illness Factors effecting pulse/respirations/blood pressure Body build Blood pressure Drugs Exercise Foods Temperature Disease processes Pain Age Occasions for Measuring V/S Screenings at health fairs and clinics Upon admission to a healthcare setting When certain medications are given Before and after diagnostic and surgical procedures Before and after certain nursing interventions In emergency situations Hospital routine Changes in general condition Nonspecific symptoms of physical distress and stress. Body Temperature Definition: the heat of the body measured in degrees The difference between production of heat and loss of heat Normal temperature: 97.0ºF (36.0ºC) to 99.5ºF (37.5ºC) Process: heat is generated by metabolic processes in the core tissues of the body, transferred to the skin surface by the circulating blood, and dissipated to the environment Factors which Cause Variations in Body Temperature 1. Age 2. Exercise 3. Hormonal Influences 4. Diurnal Variations 5. Stress 6. Environment 7. Ingestion of hot/cold liquids Sites for Measurement of Temperatures Core temperatures Tympanic and rectal Esophagus and pulmonary (invasive monitoring devices) Surface body temperatures Oral (sublingual) Axillary Temporal Inserting Tympanic Thermometer into Patient’s Ear Contraindications to Temperature Measurement sites Oral: impaired cognitive functioning, inability to close lips around thermometer, diseases of the oral cavity, and oral or nasal surgery Rectal: newborns, small children, patients who have had rectal surgery, or have diarrhea or disease of the rectum, and certain heart conditions Tympanic: earache, ear drainage, and scarred tympanic membrane Overhead Radiant Warmers Used for infants exposed to stressors or chilling Used for infants with underlying conditions that interfere with thermoregulation Minimizes the oxygen and calories that the infant would expend to maintain body temperature Minimizing the effects of body temperature changes on metabolic activity Cooling Blanket/Hypothermia Pad Conducts a cooled solution, usually distilled water, through coils in a plastic blanket or pad Helps to lower or maintain body temperature Characteristics of the Pulse Pulse rate Measured in beats per minute Pulse quality (amplitude) The quality of the pulse in terms of its fullness Pulse rhythm Pattern of the pulsations and the pauses between them Normally regular Methods of Assessing the Pulse Palpating the peripheral arteries Auscultating the apical pulse with a stethoscope Using a portable Doppler ultrasound Common Pulse Sites Temporal Carotid Brachial Radial Femoral Popliteal Posterior tibial Dorsalis pedis Palpating the Radial Pulse Assessing an Apical Pulse Indications Patient is receiving medications that alter heart rate and rhythm A peripheral pulse is difficult to assess accurately because it is irregular, feeble, or extremely rapid Method Count the apical rate 1 full minute by listening with a stethoscope over the apex of the heart Most reliable method for infants and small children; can be palpated with fingertips Assessing Respirations (Normal Findings) Rate Adults: 12 to 20 times per minute Infants and children breathe more rapidly Depth Varies from shallow to deep Rhythm Regular: each inhalation/exhalation and the pauses between occur at regular intervals Assessing Respiratory Rate, Depth, and Rhythm Method Inspection (observing and listening) Listening with the stethoscope Counting the number of breaths per minute Considerations If respirations are very shallow and difficult to detect visually, observe sternal notch Patients should be unaware of the respiratory assessment to prevent altered breathing patterns Factors Affecting Respirations Exercise Medications Smoking Chronic illness or conditions Neurologic injury Pain Anxiety Respiratory patterns Dyspnea Tachypnea Shallow Cheyne-stokes Hyperventilation Kussmaul's respirations Signs of Respiratory Distress Retractions Nasal flaring Grunting Orthopnea (breathing more easily in an upright position) Tachypnea (rapid respirations) Sample Nursing Diagnoses Related to Respiratory Status Ineffective Breathing Pattern Impaired Gas Exchange Risk for Activity Intolerance Ineffective Airway Clearance Excess Fluid Volume Ineffective Tissue Perfusion Blood Pressure Definition The force of the blood against arterial walls Systolic pressure The highest point of pressure on arterial walls when the ventricles contract Diastolic pressure The lowest pressure present on arterial walls during diastole (Taylor, 2007). Measuring Blood Pressure Blood pressure is measured in millimeters of mercury (mm Hg) Blood pressure is recorded as a fraction The numerator is the systolic pressure The denominator is the diastolic pressure Pulse pressure The difference between the systolic and diastolic pressure Blood Pressure Assessment (Methods) Using a stethoscope and sphygmomanometer Using a Doppler ultrasound Estimating by palpation Assessing with electronic or automated devices Measuring Blood Pressure Ensuring an Accurate Blood Pressure Reading Use a cuff that is the correct size for the patient Ensure correct limb placement Use recommended deflation rate Correctly interpret the sounds heard Factors Affecting Blood Pressure Reading Age Exercise Position Weight Fluid balance Smoking Medications Pain Acute pain is of short duration, usually the result of an injury, surgery or illness. This type of pain includes acute injuries, post-operative pain and post-trauma pain. Chronic pain is an ongoing condition, such as back and neck pain, headaches Pain Nociceptive pain is caused by stimulation of peripheral nerve fibers that respond only to stimuli approaching or exceeding harmful intensity (nociceptors) The most common categories being "thermal" (heat or cold), "mechanical" (crushing, tearing, etc.) and "chemical" (iodine in a cut, chili powder in the eyes). Neuropathic pain is caused by damage or disease affecting any part of the nervous system involved in bodily feelings . Peripheral neuropathic pain is often described as “burning,” “tingling,” “electrical,” “stabbing,” or “pins and needles.” Pain Phantom pain is pain from a part of the body that has been lost or from which the brain no longer receives signals. It is a type of neuropathic pain. Numerical Pain Scale – 0-10 scale Oxygen Saturation Oxygen saturation is an indicator of the percentage of hemoglobin saturated with oxygen at the time of the measurement. P U R P O S E: Pulse oximetry is a noninvasive monitoring technique used to estimate the measurement of arterial oxygen saturation (SaO2) of hemoglobin. Normal oxygen saturation values are 97% to 99% in the healthy individual. An oxygen saturation value of 95% is clinically accepted in a patient with a normal hemoglobin level.