anatomy of the skin
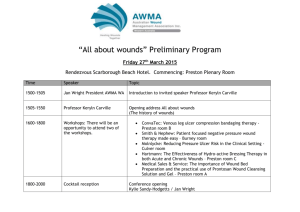
advertisement
Anatomy of the skin Aims and objectives • To understand the underlying structures of the skin • To gain a basic understanding of the process of wound healing. • To be able to identify different tissue types in areas such as the wound bed, wound edge and surrounding skin Anatomy of the skin Is it important to know the Structure and functions of the skin? • How many layers does the skin consist of? • Largest and most visible organ • Made up of two main layers: Epidermis – very thin layer and is firmly attached to the dermis at the dermo- epidermal junction. Dermis- made up of two layers comprising of fibrous proteins, collagen and elastin which give skin its strength and elasticity. Below dermis is subcutaneous layer , this provides support to the dermis and stores fat which protects the internal structures. • Does the skin vary in depth? • Thinnest over eyelids -O.1mm • Thickest over palms and soles of the feet – 1mm The skin is the largest organ of the body it weighs between 6-8 1bs It has a surface area of 20 square feet. What are the functions of the skin? • Protection of internal structures – physical barrier to microorganisms and foreign matter. • Acid PH helps to prevent infection • Sensory perceptionAllows you to feel pain, pressure heat this helps us to identify potential dangers and avoid injury • ThermoregulationBlood vessels constrict or dilate to raise or lower body temperature. Sweat production promotes cooling • Excretion – Transmits small amounts of water and body waste via sweat Helps to prevent dehydration. • Metabolism-Photochemical reaction in the skin produces Vitamin D essential for metabolism of calcium • Absorption-Some substances can be absorbed directly into blood stream • Communication Functions of the skin that declines with age. • Flattening of the dermal-epidermal junction, increased susceptibility to friction/ shearing forces resulting in blistering. • Decreased sensitivity to pain perception • Epidermis becomes thinner and flatter , uneven distribution of melanocytes leading to uneven pigmentation. • Skin becomes wrinkled due to depletion of elastic fibres. • Skin becomes dry as a result of atrophy of sebaceous glands Baraboski (2003) and Beldon (2006) How do wounds heal? Classification of wound healing • Wounds that heal by primary intention e.g. incisional wounds • Wounds that heal by secondary intention e.g. pressure ulcers • Wounds that heal by tertiary intention e.g. delayed suture 19 • Wounds characterised by whether they are acute or chronic Acute wounds Characterised by: • No underlying aetiology i.e. trauma • Short duration • Normal inflammatory phase • Heal and do not breakdown 21 Chronic wounds Characterised by: • Underlying pathology e.g. venous insufficiency • Prolonged duration • Hyperactive state • Persistent state of inflammation 22 • Wounds go through 4 distinct phases Normal Wound Healing Response Proteoglycans Neutrophils Fibroblasts Collagen remodelling Collagen Scar maturation Angiogenesis MATURATION Macrophages Platelets Lymphocytes Fibrin PROLIFERATION INFLAMMATION HAEMOSTASIS MINUTES DAYS WEEKS MONTHS / YEARS(whru) Haemostasis •Starts immediately after injury. •Blood vessel contraction (vasoconstriction) Inflammatory phase •Occurs between 0-3 days Proliferation •0-24 days Maturation •20 days – 2 years •Closure of wound and re-epithelisation. •Scar maturation What factors may affect wound healing? Factors Affecting Healing Systemic •Age •Anaemia •Nutrition • Medications e.g.: Anti inflammatory, Cytotoxic drugs, steroids •Chronic health conditions eg :Diabetes Mellitus •Systemic infection (Bowler & Davies, 1999) •Oxygenation •Smoking •Psychological factors •Temperature Factors affecting healing Local Factors •Blood supply •Denervation •Haematoma •Local Infection •Duration •Wound bed condition •Anatomical site •Size of wound • Assessment of a wound is the responsibility of the qualified member of staff • You should ensure that this has been undertaken and a treatment plan has been established. Remember The selection of dressings or bandages without accurately undertaking a wound assessment taking into account underlying factors that may delay wound healing may result in costly treatments that are inappropriate and are not successful! Clinical appearance of wound bed Colour Black Yellow Red Pink Green Physiological State Necrotic Sloughy Granulating Epithelializing Infected? Characteristics of granulation tissue Healthy tissue Unhealthy tissue Bright red Dark red Moist Dehydrated Shiny Dull Does not bleed Bleeds easily 35 Granulating (WHRU) Necrosis (WHRU) Slough Clinical appearance of surrounding skin Maceration Excoriation Erythema and oedema Eczema and dry skin Exudate • Quantity – Small , moderate copious is dressing containing exudate? • Colour – Green? serous?, haemoserrous? • Consistency – Thick?Thin, Pain • When does it occur? • How bad (intense) is it? • How does the patient describe it? • What makes it better? • If there are any changes in the wound report immediately to your nurse in charge • Any delay in a reassessment may result in inappropriate treatment