skin tumour
advertisement

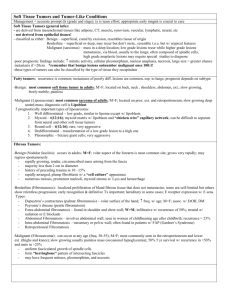
Skin Tumors Introduction The great majority of cutaneous tumors are of little consequence and may never attract the attention of the patient or his physician Genetic and environmental factors play an important role Many skin tumors (e.g. actinic keratoses, basal cell carcinomas, squamous cell carcinomas and malignant melanomas) would all become less common if fair skinned people protected themselves adequately against sunlight. Accurate diagnosis is a must for proper management of skin tumors. Biopsy as and when in dilemma is a must. Classification Tumors of skin are broadly classified as Benign, Premalignant and Malignant They may also be classified according to their origin as: ◦ Epidermal ◦ Appendageal - Pilar(hair), sebaceous and sweat gland ◦ Melanocytic ◦ Mesodermal origin (vascular and connective tissue) Tumors arising from epidermis Benign Premalignant Seborrheic keratoses Leukoplakia Epidermal nevi Cutaneous horn Epithelial cyst Bowen’s disease Steatocystoma multiplex Paget’s disease Keratoacanthoma Actinic keratoses Malignant Squamous cell carcinoma Tumors of epidermal appendages Benign Malignant Trichoepithelioma Basal cell carcinoma Syringoma Adnexal carcinoma Cylindroma Tumors arising from Melanocyte Malignant melanoma Tumors of mesodermal origin Connective Tissue Vascular Tumors Dermatofibroma Hemangioma Acrochordon (skin tag) Angiokeratoma Keloid Glomus tumor Neurofibroma Kaposi’s sarcoma Other Cutaneous tumors Cutaneous Metastasis Breast, lungs, colon, kidney, ovary, metastatic melanoma Lymphomas and Leukemias Cutaneous T- cell Lymphomas: Mycosis fungoides, Sezary syndrome Seborrheic keratoses Common, benign, persistent, epidermal lesion appearing as macule or papule, brownish to grey or black in colour Greasy surface with plugged horns and a classical ‘stuck on’ appearance Seen mainly on the face, trunk and extremities in adults over 30 years of age, often bilaterally symmetrical and along skin cleavage lines Dermatosis papulosa nigra: a variant seen as heavily pigmented papules on face in Indian skin Contd… Seborrheic keratoses Stucco keratoses: White lesions with a rough surface and ‘stuck-on’ appearance on the ankles of elderly; easily lifted off the skin with a finger nail without causing bleeding Diagnosis is clinical and biopsy in suspect cases to rule out malignancy Treatment Curettage Electrodessication Cryotherapy with liquid nitrogen Shaving Chemical peeling with Trichloroacetic acid(TCA) Acrochordons (skin tags) Common benign and fleshy papular overgrowths occurring in skin folds of obese middle aged women Skin-colored or brown, pedunculated or sessile most often seen in axillae, groins and on neck and eyelids Usually asymptomatic, but maybe tender if irritated by friction, jewellery or clothing Treatment Scissors excision with/ without local anesthesia gives the best cosmetic result Electrocautery or cryosurgery are other options Sebaceous cyst Firm, subcutaneous, keratin-filled cyst originating from a hair follicle Arises spontaneously after puberty; usually single, on the trunk, neck and post auricular area Fixed to overlying skin by a punctum representing the follicle May get infected, rupture and trigger a foreign body reaction leading to scarring Can recur post drainage if cyst wall persists Treatment Elective surgical excision with the cyst wall to prevent recurrence and scarring Inflamed cysts need to be incised and drained just like an abscess Recurrent cysts that have previously ruptured and scarred are best excised with the surrounding scar after the inflammation subsides Keloids Benign, cutaneous lesions produced by overgrowth of dense fibrous tissue Uncontrolled synthesis and deposition of dermal collagen May extend to surrounding skin beyond the site of injury Common in young patients, rare in infancy and old age. Females more predisposed than males. Trigger factors unknown May occur de novo but generally occur after injury, burns, surgery, laser therapy or acne Contd… Keloids Most frequently on upper back and chest, neck, shoulders, jaw, ear lobes and legs These areas exert high tension on healing wounds Hereditary predilection (autosomal dominant and recessive factors) known Clinical course Early stage : Soft and pink resembling a hypertrophic scar Late stage : Firm and white, protuberant and more extensive than original trauma, with irregular borders having claw like extensions Keloids attain a steady state size by gradual growth and are unlikely to regress on their own Treatment Intra-lesional steroid (ILS) injections : Triamcinolone acetonide 10-40 mg/ml in varying dilutions injected every 3-6 weeks till lesion flattens Combination of ILS + Hyaluronidase or 5Flurouracil for faster regression of keloids Surgical excision followed by ILS Intralesional bleomycin Cryotherapy with liquid nitrogen + ILS Constant pressure on the keloid with pressure garments or silicone elastomer pads for extensive lesions on extremities Lasers: CO2 ,Nd: Yag Neurofibromas Solitary tumor occurs occasionally, multiple neurofibromas are more common Seen as part of an autosomal dominant inherited condition - Neurofibromatosis (von Recklinghausen’s disease) Neurofibromas are pink or skin colored, soft, sessile or pedunculated papules or nodules Plexiform neurofibromas occur along the course of peripheral nerves creating irregular masses or tender nodules Button-hole sign: tumor compressible through a deficient dermis May feel ‘knotty’ or ‘wormy Neurofibromas Solitary tumor occurs occasionally, multiple neurofibromas are more common Seen as part of an autosomal dominant inherited condition - Neurofibromatosis (von Recklinghausen’s disease) Neurofibromas are pink or skin colored, soft, sessile or pedunculated papules or nodules Plexiform neurofibromas occur along the course of peripheral nerves creating irregular masses or tender nodules Button-hole sign: tumor compressible through a deficient dermis May feel ‘knotty’ or ‘wormy Treatment Excision advised in cases of : Cosmetically unacceptable or painful lesions Lesions on vital structures Lesions suspected of undergoing malignant change Hemangiomas Benign red, purple or blue vascular neoplasms occurring within the first year of life; seen in 1-3% of newborns and 10% of 1 year olds They exhibit endothelial cell hyperplasia More likely to be seen in girls and premature infants; predilection for the head and neck Can appear at any site including the oral or genital mucosa Multiple cutaneous hemangiomas may be associated with visceral hemangiomas Contd… Hemangiomas Lesions may ulcerate, bleed and get infected Hemangiomas near eyes, ears, mouth or viscera can threaten the function of these organs Hemangiomas and Portwine stain - common vascular malformation Hemangioma (hamartoma) Portwine stain (vascular esctasia) Clinical course Early hemangiomas may appear flat and pale white with few telangiectasia and dilated blood vessels In growth phase, they are bright red(superficial) and purple(deep) and feel firm and rubbery Involuting hemangiomas are slate-gray and begin to soften Treatment Benign and self- limiting; therefore no treatment is required in most cases Parents need to be reassured about the course of the growth and its subsidence in 5-7 years Recurrent bleeding, infection, ulceration or pressure on vital structures need active treatment Treatment options: Steroids, sclerotherapy, embolisation, compression, laser therapy Actinic keratoses Common, persistent keratotic lesions with malignant potential Predisposing factors: Cumulative sun exposure, fair skin (type I and II) Affect the middle aged and elderly in temperate climates but younger people in the tropics Clinical features Pink or gray rough scaling macules or papules in the sun exposed areas; roughness better felt than seen 10-20% of lesions progress to squamous cell carcinoma Diagnosis is clinical but biopsy is warranted where malignancy is suspected Treatment Cryotherapy with liquid nitrogen or CO2 snow is simple and effective Electrodesiccation and curettage for larger lesions 5- flurouracil (5%) cream and imiquimod (5%) cream for multiple lesions Photodynamic therapy CO2, Er:YAG lasers, dermabrasion Cutaneous horn Hard, yellowish brown, horny outgrowth, often curved with circumferential ridges Surrounded by acanthotic collarette Inflammation and induration beneath indicates malignant change Seen on exposed areas specially upper part of face and ears Squamous Cell Carcinoma (SCC) Invasive, primary skin malignancy arising from keratinocytes of skin or mucosa Can be fatal by local spread or metastasis if left untreated Sites: Most commonly seen on head, neck or hands of elderly patients. Mucosae and mucocutaneous junction more common in Indians; sun exposed areas commonly in whites Predisposing factors Skin types I - III, UV exposure, radiation, arsenic and hydrocarbon, chronic inflammation, burns( Marjolin’s ulcer) Spices, spirits, smoking (and chewing tobacco), syphilis, sharp tooth predispose to oral SCC Human papilloma virus (HPV) infection is risk factor for cervical and genito-anal SCCs May arise de novo or from precursor skin lesions Precursor skin lesions Lupus vulgaris Hypertrophic lichen planus Stasis ulcers Discoid lupus erythematosus Sinuses as in chronic osteomyelitis, pilonidal sinus, hidradenitis suppurativa Post burns or vaccination scars Actinic keratosis Bowen’s disease Clinical features De novo: sharply defined, smooth, dull red, firm, dome shaped nodule with crusted centre. Removal of crust shows foul smelling keratin debris. Surrounding skin shows signs of photodamage such as wrinkling and telangiectasia From prior skin lesions: irregular borders, induration; bleeding heralds the onset of malignancy Regional lymph node enlargement and metastases to other organs known if left untreated Treatment Wide local excision with histologic confirmation of margins Regional lymph node dissection if involved Mohs’ micrographic surgery Radiation therapy or chemotherapy in inoperable cases SCCs on lip, scalp and ear - more aggressive and more likely to metastasize Ensure regular follow-up to look for recurrence Basal Cell Carcinoma (BCC) Synonym : Basalioma, Rodent ulcer Most common cutaneous malignancy Locally invasive and destructive; usually slow growing, rarely metastasizes Fair skin, sun exposure, ionizing radiation and age > 40 years are risk factors Seen mainly on sun-exposed areas like face, scalp, ears and neck, less often on trunk and extremities Clinical course Nodulo-ulcerative type begins as a flesh coloured waxy nodule with telangiectasia → enlarges → central ulceration → deepens → rolled out, beaded edges → destroys structures locally as deep as bone or cartilage → aptly named ‘rodent ulcer’ Rare metastasis (about 10%) but recurrence known after inadequate treatment Treatment Simple excision with a margin of 2-5 mm is the treatment of choice. Mohs’ micrographic surgery for recurrent BCCs Curettage and cautery, cryotherapy for small lesions Radiation therapy, photodynamic therapy and topical immunomodulators for localised, well defined growths or for patients refusing surgery 5 year cure rates are almost 90% for primary and 83% for recurrent BCCs Malignant melanoma Increasingly common malignancy of melanocytes, most often arising in the skin Potentially curable with early diagnosis and treatment; late diagnosis carries poor prognosis Predisposing factors Fair skin (Type I & II) Personal / family history of atypical nevi or melanoma Presence of congenital nevi (number is proportional to risk) History of frequent sunburn Clinical course 30% of melanomas arise in pre-existing nevi whereas 70% arise de novo Begins as irregularly pigmented macule or plaque → change in color, shape and size Nodular variant → dermal involvement → high risk of metastasis → poor prognosis Prognostic factors ABCDE of melanoma Asymmetry Border irregularity Color variability Diameter > 1 cm Evolutionary change Management Diagnosis : Biopsy is the most definitive diagnostic tool. Excision biopsy preferred Treatment : Complete excision of the lesion with a free margin of at least 1cm is the only reliable therapy For local, regional or distant metastasis, options include wide excision, lymph node resection, chemotherapy and immunotherapy Thank you