Preoperative care
advertisement

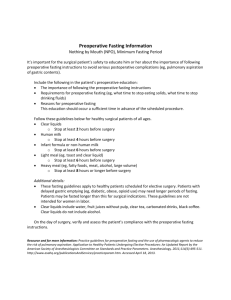
Dr Edward Sang, Fellow, Gynaecologic Oncology Definitions Preoperative care: the patient management period during which time gynaecologic pathology, defects and injury are assessed and diagnosed; an accurate decision is made for a surgical intervention; the patient is appropriately appraised of the problem and need for surgery as well as options available; and necessary preoperative evaluation and preparation is accomplished Definitions Assessment Diagnosis Correct decision for surgery Patient appraisal: options Pre-op evaluation and preparation Definitions Preoperative evaluation: the assessment of a patient before surgery to detect factors that could affect surgical outcome and may include physical examination, laboratory testing, imaging and consultations Introduction The preoperative care and management of women has proven to be a critical factor in achieving successful outcomes of both emergent and scheduled gynaecological surgical procedures Important aspects History and physical examination Important aspects Lab tests and imaging Avoid routine tests Consultations Introduction Minimal preoperative testing for the uncomplicated patient and specific testing and imaging for the complicated case Each patient must be considered as an individual Importance of preoperative care Successful surgical outcomes in operative gynaecological procedures occur as a result of several factors which include: Appropriate preoperative evaluation Appropriate patient selection Appropriate discussion with the patient regarding benefits and risks of the surgery Costs/ medical aid Purpose of preoperative evaluation Decrease surgical morbidity Minimize expensive delays and cancellations on the day of surgery Evaluate and optimize patient health status Facilitate the planning of anaesthesia and perioperative care Reduce patient anxiety through education Obtain informed consent Important questions Is the patient in optimal health? Can, or should, the patient’s physical or mental condition be improved before surgery? Does the patient have health problems or use any medications that could unexpectedly influence perioperative events? History History best taken by the surgeon To determine best procedure and timing Avoids unnecessary surgery Pre-printed forms or computer templates may be used. They help avoid omissions but may not be applicable to every case Gynaecological history The menstrual history must be accurate and detailed Pregnancy may need to be confirmed or excluded Accurate date of menopause Pregnancy and its complications Urologic history Gastrointestinal history: symptoms may mimic gynae problems Endocrine and metabolic diseases Orthopaedic and neurologic history Physical examination Start with complete physical examination Breast examination Abdominalexamination Pelvic and rectal examination Laboratory assessment/tests FBC Uec Glucose ECG Preop preparation Ovarian suppression with GnRHa 2-3m before hysteroscopic resection of submucous fibroids Vaginal oestrogen cream 4-6w before surgery to thicken vaginal mucosa Regulation of meds eg Insulin, warfarin When to admit: usually day of surgery Food intake: no evening meal on day before surgery ? Bowel prep. Recent evidence advises avoid Preop preparation A good nights’ rest. Consider mild sedative Preop antibiotics Pubic or abdominal hair clipping Catheterization EUA Perineum and vaginal cleansing Abdominal preparation-povidone iodine