Carcinoma of the Vulva for undergraduate students
advertisement

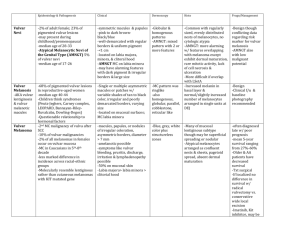
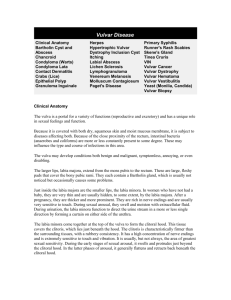
Carcinoma of the Vulva Incidence of malignant diseases the vulva: 3 - 4% of all gynecologic malignancies. - The incidence increases with age. - Recently there was a rise in the incidence, due to • • • Longevity Increased HPV infections. Increased smoking habits Risk factors for carcinoma of the vulva: 1- Human papillomavirus infection. – Genital condylomas: these are detected in 5 % of vulvar cancer. – Vulvar intraepithelial neoplasia (VIN) and also CIN. 2- Medical history of: – Vulvar dystrophy. – Chronic vulvar pruritus. 3- Patients with a history of squamous cell carcinoma of the cervix or vagina. 4- Chronic immunosuppression. 5- Smoking 2 Types / Variants (15%) (85%) (90%) (5%) (2-3%) Vulvar Cancer Stages FIGO System • Stage 0 - Carcinoma in situ, VIN 3, severe vulvar dysplasia. • Stage I - Tumor 2 cm or less, and confined to the vulva or perineum – IA - Less than 1 mm invasion below the surface layer – IB - More than 1 mm invasion below the surface layer • Stage II - Cancer is confined to the vulva and/or perineum, and larger than 2 cm. • Stage III - Cancer has spread to – the lower urethra or vagina or anus – and / or local lymph nodes on one side. • Stage IV – A - Cancer has spread to the • Upper urethra or bladder or rectum • or local lymph nodes on both sides. – B - Cancer has spread to the pelvic lymph nodes and/or sites more distant. T N M STAGING • T-0 pre-malignant change • T-1 – A a cancer less than 2.0cm in diameter and less than 1.0mm in depth of invasion – B a cancer less than 2.0cm in diameter but greater than 1.0mm in invasion • • • T-2 greater than 2.0 centimeters in diameter T-3 involves vagina, urethra or anus T-4 involves bladder, rectum or pelvic bone N-0 no lymph nodes involved • N-1 lymph node metastases to one groin N-2 lymph node metastases to both groins • M-1 any distant metastases • M-0 no distant metastases Stage I and II Stage III Stage IV Diagnosis The diagnosis often is delayed: 1- Patients do not ask early consultation. They consider the symptoms as a trivial skin condition. 2- Physicians may neglect small skin lesions. Types of complaints: • The most common complaint is a palpable vulvar lesion. Chronic pruritus vulvae. • Asymptomatic 20% of patients: the lesion is detected during examination for unrelated condition. • Later the lesion becomes necrotic cauliflower or hard ulcerated. – Bleeding, watery discharge, superinfection and pain may develop. • Melanomas: frequently appear as bluish black, pigmented, or papillary lesions. Diagnosis 1) Local examination of the relevant areas: early lesions appears as chronic vulvar dermatitis. 2) Clinical assessment of the lymph nodes is to be performed in the relevant regions. 3) Biopsy: 1- From the suspected lesions: a) Dermal punch biopsy using a local anesthetic: Lesions < 1 cm b) Excisional biopsy under general anesthesia: Lesions > 1 cm: 2- From the lymph nodes in the relevant regions when suspected for metastasis. Differential diagnosis: 1- Venereal diseases: syphilis, chancroid, lymphogranuloma venereum, granuloma inguinale. 2- VIN. An association between invasive and noninvasive lesions is a possibility. 3- Condyloma acuminatum. Prophylaxis…A high index of suspicion • • Detection and management of VIN. Proper management of all cases with pruiritus vulvae. • All vulval lesions should be diagnosed accurately especially those arising after menopause. • All pigmented vulvar lesions should be removed for biopsy. Management Modalities Surgical Treatment Radical Vulvectomy Radiotherapy Pre-operative En Block Dissection 3-in one incision Post-operative Chemotherapy Radiation Sensitizer Metastatic Conditions Treatment Options by Stage Stage Treatment Option Partial Vulvectomy excision of the tumor, with a 1 cm safe margins. No need Ia for node removal. Ib Modified radical vulvectomy with either of the following: 1) Ipsilateral groin lymph node dissection: in cases of lateralized lesion 2) Bilateral groin node dissection: in cases of centralized lesions II III Modified radical vulvectomy with bilateral groin node dissection. IV Individualized - Combined approach: 1- Preoperative external beam radiation therapy. 2- Chemotherapy (e.g. 5-fluorouracil, cisplatin). 3- Radical excision with bilateral inguinal & femoral node dissection. 4- Preoperative RT, then surgical excision of the tumor. - Pelvic exenteration. Vulvectomy: • There are several operations in which part of the vulva or all of the vulva is removed: – A skinning vulvectomy means only the top layer of skin affected by the cancer is removed. Although this is an option for treating extensive VIN3, this operation is rarely done. – Simple vulvectomy, the entire vulva is removed. – Radical vulvectomy can be complete or partial. • When part of the vulva, including the deep tissue, is removed, the operation is called a partial vulvectomy. • In a complete radical vulvectomy, the entire vulva and deep tissues, including the clitoris, are removed. – An operation to remove the lymph nodes near the vulva is called a en block dissection. It is important to remove these lymph nodes if they contain cancer. Sentinel Lymph Node Skinning / Simple Vulvectomy Radiotherapy • Malignant diseases of the vulva are not commonly managed by RT because of the intolerance of surrounding normal tissues. – Chemotherapy as radiation sensitizer can improve response of the malignant tissues. • Indications of RT in malignant diseases of the vulva: – Preoperative RT in stage III and IV: • • The lesion shrunk and it limits the need for pelvic exenteration. It also improves surgical respectability of tumors. – Postoperative RT: can reduce regional recurrences and inguinal lymph node metastases. • • • • Multiple positive groin nodes: It decreases the incidence of recurrence. Positive surgical margins as seen on microscopic examination. Multiple focal recurrences. When the tumor size is > 4 cm Malignant Tumors of the Vagina • Incidence – 1% of gynecologic malignancies. – It is the 5th in frequency of primary genital malignant diseases. – Average age at diagnosis is 65 years old. • High risk factors: – VaIN – Human papillomavirus infection of the cervix or the vulva. – Cervical or vulvar cancer. – Exposure to diethylstilbestrol (DES) in utero is associated with the development of vaginal adenosis • It might progress to clear cell adenocarcinoma of the vagina and cervix in young wome • The mean age at diagnosis of this rare malignancy is 19 year. Pathological Types: • Secondary malignant tumors of the vagina are more common than the primary tumors. – The primary lesion may be in the cervix or elsewhere in the body. • Primary malignant vaginal tumors: – Squamous cell carcinomas: 85% of primary vaginal malignancies. – Adenocarcinomas. These occur at younger age group. – Clear cell adenocarcinomas secondary to DES exposure. – Melanoma. – Sarcoma: Sarcoma botryoides (embryonal rhabdomyosarcoma) • The peak incidence is in young children at the age of 3 years. • Symptoms of malignant lesions of the vagina: – Abnormal vaginal bleeding: may be postcoital, intermenstrual, or postmenopausal. – Watery vaginal discharge. – Dyspareunia. – Vesicovaginal or rectovaginal fistulae are late manifestations of vaginal cancer. – Few patients are asymptomatic; a lesion may be discovered during a routine pelvic examination, or a Pap smear may be abnormal. • Signs of malignant lesions of the vagina:: – Local examination: the need to inspect the whole vagina entails modification from the routine speculum examination. – A polypoid lesion is the commonest macroscopic appearance. – A punch biopsy usually yields a diagnosis, but occasionally wide local excision using an anesthetic is necessary. Most lesions occur in the upper 1/3 of the vagina on the posterior wall. – Colposcopy, cystoscopy, and proctosigmoidoscopy and bone scan are needed to detect spread. Spread: • Direct spread: into the local paravaginal tissues, bladder, or rectum. • Lymphatic spread: – Lesions in the lower vagina: to the inguinal lymph nodes. – Lesions in the upper vagina: to the pelvic lymph nodes. • Hematogenous spread: late event. Reach liver, lung, bone. Staging Stage 0 Carcinoma in situ, intraepithelial neolasia Stage I Carcinoma limited to the vaginal wall Stage II Involved the subvaginal tissue but not extended to lateral pelvic wall Stage III Extended to pelvic wall Stage IV a Spread to adjacent organs or direct extension beyond the true pelvis. Stage IV b Spread to distant organs Stages I & II Stage III Treatment: • Management of stage 0: – Topical fluorouracil for stage 0: • It causes intense burning. • Long standing benefits is not proven yet • Laser therapy • Primary localized tumors: – RT: a combination of external beam and brachytherapy. – Surgery: it is an alternative treatment for early lesions. • Radical hysterectomy with upper vaginectomy. • Pelvic exenteration: in vesicovaginal or rectovaginal fistulas. Prognosis: • The 5-year survival is as follows: – Stage I 65-70% – Stage II 47 % – Stage III 30% – Stage IV 15-20%