- Northent

BENIGN THYROID
DISORDERS
Regional SpR Teaching
Woo-Young Yang
ST5
CLASSIFICATION
Simple Non-Toxic
Toxic
Inflammatory
Neoplastic
Rare
CLASSIFICATION
Simple Non-Toxic
Iodine Difficiency
Multinodular Goitre
Solitary Nodule
Physiological
Toxic
Grave’s Disease
Plummer’s Disease
Inflammatory
Hashimoto’s Thyroiditis
De Quervain’s
Thyroiditis
Riedel’s Thyroiditis
Neoplastic
Follicular
Papillary
Medullary
Anaplastic
Lymphoma
Metastatic
Rare
Infective
Iatrogenic
IODINE DIFFICIENCY
Epidemiology
Commonest cause of goitre and hypothyroidism world wide
Not common in the western world
Pathophysiology
Insufficient iodination of thyroglobulin
Decrease in Thyroid Hormone
Increase in TSH
Diffuse hyperplasia(+/- multinodular appearance)
Pregnancy
Increased demand on maternal iodine
Worsening features with subsequent pregnancies
Treatment
Iodine Replacement
EUTHYROID MNG
Epidemiology
Incidence by Palpation – 10%
Incidence by Imaging – up to 50%
Aetiology
Benign
Colloid cyst
Simple cyst
Adenoma
Infection
Malignant
INVESTIGATIONS
Serological
TFT
Serum Calcitonin?
FNAC
USS
((useful in looking for malignant features such as microcalcification and capsular invasion/increased vascularity))
CT/MRI – for retrosternal component
Tc99/I123 Scintigraphy – NOT useful in MNG/SN
((BTA and ATA, incidence of cancer 10% in cold nodules))
TREATMENT
Surgery
Cosmetic
Compressive symptom
Suspicion for cancer
Radioiodine
Indicated if unfit for surgery
Regression of the goitre size
SOLITARY NODULES
Mx is broadly similar to MNG
Cystic nodules
Many resolve spontaneously
Larger cysts tend to recur
Treatment
Simple aspiration and expectant approach with small cysts(<3ml)
Surgery for the larger ones(10% cancer risk)
CLASSIFICATION
Simple Non-Toxic
Iodine Difficiency
Multinodular Goitre
Solitary Nodule
Physiological
Toxic
Grave’s Disease
Plummer’s Disease
Inflammatory
Hashimoto’s Thyroiditis
De Quervain’s
Thyroiditis
Riedel’s Thyroiditis
Neoplastic
Follicular
Papillary
Medullary
Anaplastic
Lymphoma
Rare
Infective
Iatrogenic
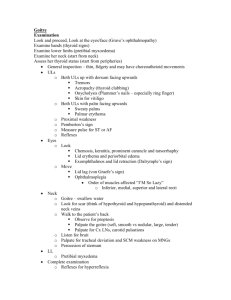
HYPERTHYROIDISM – CLINICAL
FEATURES
Cardiac
Tachycardia, AF
High output congestive heart failure
Thermoregulatory
Heat intolerance
Metabolic
Weight loss
Increased appetite
GI
Diarrhoea
Neuopsychiatric
Irritability
Anxiety
Dermatological
Hair loss and brittle nails
Hormonal
Irregular menstruation
Misc
Fine tremor
Thyroid bruit
HYPOTHYROIDISM – CLINICAL
FEATURES
Cardiac
Bradycardia
Thermoregulatory
Cold intolerance
Metabolic
Weight gain
Decreased appetite
Glucose intolerance
GI
Constipation
Neuopsychiatric
Depression
Mental impairment
Dermatological
Dry skin
Myxoedema
Hormonal
Irregular menstruation
Misc
Hoarseness
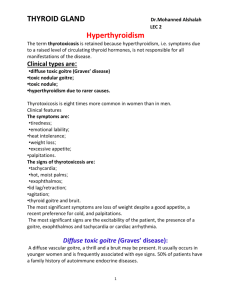
GRAVE’S DISEASE
Epidemiology
Commonest cause of hyperthyroidism(60%)
UK incidence 80/100,000
Pathophysiology
Autoantibodies against TSH receptor
Stimulation of thyroid gland hyperplasia
Autonomous production of T3 and T4
Association with other organ-specific autoimmune diseases
Pernicious anaemia, DM, Addison Disease, Myesthenia
Gravis
HLA-DR3, B8
GRAVE’S DISEASE – CLINICAL
PRESENTATION
Thyroid
Manifestations
Diffuse symmetrical goitre +/- bruits
Hyperthyroidism
Extrathyroid
Manifestations
Acropachy
Myxoedema
Grave’s ophthalmopathy
GRAVE’S OPHTHALMOPATHY
Pathophysiology
Lymphocytic infiltration and glycosaminoglycan deposition
Extraocular muscle swelling
Periorbital fat proliferation
GRAVE’S OPHTHALMOPATHY
Clinical Features
Proptosis greater than 22 mm
Lid retraction and lid lag
Conjunctival oedema and corneal ulceration
Oculomotor problem
Decreasing visual acuity
Rx options
High dose steroids
Radiotherapy
Surgical – alignment/decompression
TOXIC MULTINODULAR GOITRE
Epidemiology
Commonly found in the elderly
Pathophysiology
Jod-Baselow Phenomenon
((exact mechanism is obscure. Background iodine deficiency, followed by iodine Xs, leading to unmasking hyperthyroidism. Normal follicular architecture becomes disrupted, leading to inefficient iodine trapping))
‘T3 toxicosis’ – subclinical hyperthyroidism
((importance of
T3 measurement))
TOXIC ADENOMA
Plummer’s Disease
Epidemiology
Rare – 2 % of hyperthyroidism
Younger than Toxic MNG
Pathophysiology
Somatic, non-inherited TSH receptor mutation
Autonomous TSHR activation and
TOXIC GOITRE - INVESTIGATIONS
TFT
Thyroid Autoantibodies
TPO
((actually the most senstive marker of grave’s disease – 45% for
TSH R))
Thyroglobulin
TSH receptor
Scintigraphy
Distinction between toxic nodule and Grave’s disease
TOXIC GOITRE - TREATMENT
Difference between Grave’s disease and Toxic
MNG/Adenoma
Grave’s disease may go into remission(30%)
Toxic MNG/Adenoma does not go into remission
Treatment Options
Antithyroid Drugs
Radioiodine
Surgery
ANTITHYROID DRUGS
Thionamides
Carbimazole, Methimazole, Popylthiouracile(PTU)
Pharmacophysiology
Inhibition of the organification and oxidation of iodine
T4/T3 synthesis inhibition
? Immunomodulation effect for Grave’s disease?
Side effects
Deranged LFT - rarely drug-induced hepatitis
Agranulocytosis(1/1,000)
OTHER DRUGS
Beta-blocker
Propranolol
Anticoagulants
AF management
RADIOIODINE 131
First treatment of choice for Grave’s Disease and
MNG
PO administration
Pharmacophysiology
Beta radiation – DNA damage and apoptosis
(different from I 123, which emits gamma rays)
Dose
? Titration
400 – 600 MBq sufficient for both Grave’s and Toxic MNG
RADIOIODINE 131
Side effect
Hypothyroidism
Thyroiditis
Safety?
Outpatient treatment
Avoid contact with children
((sleep alone/no sharing utensils))
Contraindication
Pregnancy
Breast feeding
TOXIC GOITRE - SURGERY
Indications
Refractory to radioiodine
Patient’s rejection of radioiodine
Severe ophthalmopathy
Pregnancy with uncontrolled disease
Cosmetic
Pre-op Preparation
Antithyroid treatment
Potassium Iodide if antithyroid drug not tolerated
((saturates the thyroid with iodine, then the gland turns off the absorption mechanism))
TOXIC GOITRE - SURGERY
Grave’s Disease
Total thyroidectomy
Toxic Adenoma
Thyroid Lobectomy
Toxic SMG
? Subtotal thyroidectomy
HYPERTHYROIDISM IN PREGNANCY
Grave’s Disease
Thionamides are safe in pregnancy
PTU is preferred as less drug is delivered to foetus
Intra-partum – Transient Hyperthyroidism of hyperemesis gravidarum
((betaHCG and TSH share the same subunit))
Post-partum Thyroiditis
((distinction by autoAb, clinical signs, iodine uptake(postpartum)))
INFLAMMATORY GOITRES -
HASHIMOTO’S THYROIDITIS
Anti-TPO/Thyroglobulin/TSHR autoAb
Initial transient hyperthyroidism due to cellular destruction and release of the preformed thyroid hormones
Subsequent hypothyroidism
Rubbery diffuse thyroid enlargement
Treatment
Thyroid replacement
Surgery if necessary
INFAMMATORY GOITRES – DE
QUERVAIN’S SUBACUTE THYROIDITIS
Granulomatous inflammation of the thyroid gland ? 2y to viral infection
Subacute course over weeks/months
Tender symmetrical diffusely enlarged goitre
Phases
hyperthyroid – hypothyroid – euthyroid(recovery)
Treatment
Thyroid status control
NSAIDs
INFLAMMATORY GOITRES – RIEDEL’S
FIBROSING THYROIDITIS
Chronic Inflammation and Fibrosis of Thyroid
Gland
Very rare – 1.6/100,000
Uncertain Pathophysiology
? Autoimmune
? Part of systemic fibrosis
Spread of the fibrosis outside the thyroid gland – can cause RLN dysfunction/tracheal compression/hypoparathyroidism
RIEDEL’S FIBROSING THYROIDITIS
Clinical features
Extent of hypothyroidism depends on extent of fibrosis of the gland
Hard wooden goitre WITHOUT cervical lymphadenopathy
May have extra-cervical involvements – retroperitoneal fibrosis/mediastinal fibrosis
Investigation
Neither FNAC nor Imaging can reliably distinguish Riedel’s
Fibrosing Thyroiditis from malignancy
? PET-CT?
Open surgical biopsy is required by wedge resection
RIEDEL’S THYROIDITIS
Medical Treatment
Steroid
Tamoxifen
((not by oe inhibition but by grow factor level decrease therefore fibroblasts down))
Thyroid hormone replacement
Surgical Treatment
Wedge Resection
Further surgical Rx not recommended due to the extensive fibrosis
Prognosis
self-limiting, good prognosis