Comparisons of two inotropes
advertisement

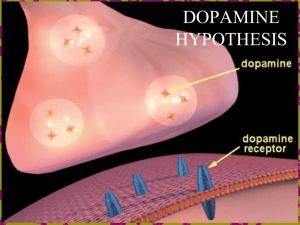
Treating Hypotension and Shock in the Newborn Keith J Barrington CHU Sainte Justine, Montreal Disclosure I have no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider(s) of commercial services discussed in this CME activity. None of the medications that I will discuss are labelled for neonatal use. Hypotension in Preterm Infants Common practice in the NICU, to treat preterm infants with a mean arterial blood pressure in mmHg < gestational age in weeks, regardless of clinical signs, Many receive a fluid bolus (or 2 or 3 or 4) and then dopamine. If the blood pressure remains « low » then dobutamine is added, and/or hydrocortisone. Other hemodynamic interventions Infants with asphyxia Infants with PPHN Babies with septic shock – Often receive multiple interventions to support the circulation. Violette day 1 Cardiovascular function in the newborn Ultrastructural: Cellular: Metabolic: Functional: Vascular: Factors are different in the neonate Ultrastructure Adult & Neonatal myocyte from the rabbit. Far fewer contractile elements. More mitochondria. Increased non contractile elements in cells. Disorganised orientation of myofibrils. Altered shape of cells….relatively short and round. Characteristic banding not clearly apparent. Decreased sarcoplasmic reticulum. Relationship of SR to sarcomere not developed. T-tubules not fully developed. Ventricular compliance in the newborn Cellular mechanisms Excitation/contraction coupling is normally triggered by an influx of Ca into the cells. Ca initially enters across the sarcolemmal membrane and then causes a secondary release of Ca from SR. (Ca induced Ca release). SR in the newborn is decreased in concentration and functionally immature. In the newborn the lack of SR means that all the calcium crosses the sarcolemma. Ca induced Ca release is absent at birth. Metabolic Neonatal myocardium utilises glucose as a substrate in preference to fatty acids. Adult myocardium uses fatty acids, in particular palmitic acid. – Change from neonatal to adult pattern of substrate utilisation occurs during first week. Greater resting myocardial blood flows and oxygen consumption. Less depression of contractility during acidosis. Functional Despite all these limitations, neonatal hearts generate high cardiac outputs and have extraordinary performance. Newborn lambs for example generate 400 ml/kg/min, and stroke volumes of 2 ml/kg cf adult sheep who have Q of 100 ml/kg/min and SV of 1 ml/kg. Functional Neonatal hearts are functionally immature and are operating at such a relatively high performance that: – There is little contractile reserve. – Frank Starling curve is flatter in newborns. – Newborns normally operate near flat portion of the curve. – Neonatal hearts are intolerant of afterload. – The right ventricle is more markedly affected by increased afterload, but the left doesn’t do very well either. Effect of afterload: neonatal lamb Catecholamine receptors The catecholamines stimulate a variety of receptors which are usually categorized as a1, a2 , b1 , b2 , DA1 and DA2. Traditionally, dopamine is said to stimulate DA receptors at low concentrations, b receptors at moderate concentrations, and a receptors at high concentrations. In reality: Dopamine has virtually no effect at the b2 receptor, and very little at the b1 receptor Enormous variation in serum concentrations are obtained by the same administered dose of drug, as much as 100 fold variations may be seen. Sympathetic innervation Cardiac sympathetic innervation is incomplete at birth. The various adrenoceptors appear at differing periods of ontogenesis. The pattern of their appearance is not well defined. b receptors increase in density in late gestation. High cardiac output at birth may partly be mediated by the presence of many functional b receptors. Further stimulation of these receptors in early life, e.g. with isoproterenol, does not much increase cardiac function. a1 receptors may appear prior to the b receptor. Myocardial adrenoceptors Dopamine receptors are present in the mature coronary circulation but not in myocardium. Frequently stated that dopamine’s inotropic effects are due to release of endogenous norepinephrine from sympathetic nerve endings (tyramine-like effect). Dopamine therefore may have indirect a and b effects on the myocardium. – Rapid tachyphylaxis The incomplete innervation of the neonatal heart means that this effect is of little importance in the newborn. Newborn hearts are not small adult Hearts! Vascular catecholamine receptors There is much less information regarding the rates of appearance and maturation of vascular adrenoceptors. a1 receptors are present in neonatal peripheral circulation and respond to a1 stimulants such as phenylephrine. a1 receptors appear to be relatively lacking in the pulmonary circulation of the lamb. Vascular b receptors are next to appear. DA receptors probably largely become active during postnatal life. Immature subjects react differently Topics PPHN Septic Shock Cardiogenic Shock Hypotension in the ELGAN What is PPHN Many infants with hypoxia and PHN do not have detectable R-L shunts at either the foramen ovale or ductus arteriosus1. The most severely hypoxic infants are more likely to have such shunts, Documented R-L shunts not required for PHN diagnosis in any of the iNO studies. – In 1 study PHN= Echo estimated peak systolic PA pressure > 35 mmHg – Abnormal, but will it cause left to right shunting? What is PPHN? If no detectable extrapulmonary shunt then what causes hypoxia? Hypoxia in infants without extrapulmonary shunt is due to ventilation perfusion mismatch. i.e. underventilated areas of perfused lung. Hypoxic respiratory failure Under-ventilated perfused areas of lung are sometimes referred to as ‘intrapulmonary shunts’, (literally true when atelectatic areas of lung are perfused) Intrapulmonary shunting does not require suprasystemic PA pressures. Majority of infants with “PPHN” and abnormal chest x-ray have moderate elevations of PA pressure, problems in oxygenation are commonly due to major ventilation perfusion mismatch Why does this matter? If R-L ductal shunting is prominent, then interventions to selectively elevate systemic pressures may decrease shunting (although they may not improve systemic O2 delivery!) If oxygenation problems are due to VQ mismatch, then pushing up the systemic pressures with vasoconstrictors is likely to only decrease systemic O2 delivery. Goals of treatment Intact survival (obviously!) Maintain or Improve oxygen delivery to vital organs – Improve systemic perfusion – Improve VQ matching • Elevate systemic pressures Interrupt process of PHN – Dilate pulmonary circulation – Specific interventions Minimize iatrogenic injury Oxygen delivery Volume of blood ejected from left ventricle Oxygen content of that blood Net shunting across the ductus – Net left to right shunting will DECREASE O2 delivery – Net right to left shunting will INCREASE O2 delivery Intracardiac shunts Foraminal shunting depends on inter-atrial pressure gradients Atrial pressures largely dependent on ventricular end-diastolic pressures Therefore depend on ventricular function (compliance, preload, contractility) Improving right ventricular function will decrease right to left inter-atrial shunting So What works? For what therapies are there good data, from prospective trials, demonstrating improved clinically important outcomes: – iNO Inhaled Nitric Oxide Improves survival without ECMO for term infants with respiratory failure and an OI greater than 25 True whether or not an echocardiogram has confirmed PHN Why would it work if there is not definite PHN? Improves VQ matching Decreases RV afterload My research assistants Inhaled NO 3 day old piglets with meconium aspiration with a closed duct Rapid increase in systemic PO2 after iNO – Improved VQ match • Barrington KJ et al Pediatric Pulmonology 1995. Inhaled NO Piglets with infusion of killed GBS Remained normoxic, but developed severe pulmonary hypertension (which never exceeds systemic pressure!) Majority die within 6 hours Progressive reduction in cardiac index With inhaled NO treatment, PA pressures fall, cardiac index maintained for 6 hours No effect on oxygenation Piglets survive Best uncontrolled data Steinhorn et al: prospective cohort study of clinical responses and pharmacokinetics of intravenous sildenafil in 36 term neonates with OI > 15 Other uncontrolled data Case Series and case reports • Prostanoids – Iloprost – epoprostanol • Endothelin antagonists – Bosentan • Magnesium • Adenosine Where are we now? What probably doesn’t work Systemic tolazoline Hyperventilation Bicarbonate infusion Paralysis – deafness Adverse effects of Hyperventilation Hyperventilated piglets with or without added CO2 – Isolate effects of respiratory alkalosis from mechanical effects Progressive systemic hypotension, increase in the PVR/SVR ratio Exaggerated increase in the PVR/SVR ratio after 4 hours of respiratory alkalosis Jundi et al 2000 In the hyperventilated normocarbic group: no changes Adverse effects of hyperventilation Decreases cerebral perfusion Associated with hearing loss and neurologic injury in follow-up studies of infants who survived Induces hypocalcemia, and myocardial dysfunction Adverse effects of Bicarbonate Worsens intracellular acidosis No evidence of beneficial effect Multi-center observational study demonstrated: marked variation in use of bicarbonate between centers, Centers that used more bicarbonate had more infants progress to needing ECMO Cardiovascular support What improves oxygen delivery? What affects PVR? What affects SVR? In human neonates with PPHN, very difficult to answer Cardiovascular Support Prospective comparative trials – Clinically important outcomes • None – Short term physiologic outcomes • None Before and after trials of individual agents – A few! Observational studies Animal data Dopamine, animal data Stimulates α1, α2 and β1-receptors and specific dopaminergic receptors, Generally, dopamine elevates both systemic and pulmonary artery pressures Because neonatal myocardium is very sensitive to increased afterload, cardiac output often falls Extremely high dopamine doses may increase SVR more than PVR, but are probably dangerous No renal vasodilatory effect – Coronary vasoconstriction Little evidence of increased oxygen delivery with dopamine No evidence of improved clinical outcomes % change in blood pressure Jirsch DW, Cheung PY. Dopaminergic receptor-mediated effects in the mesenteric vasculature and renal vasculature of the chronically instrumented newborn piglet. Crit Care Med 1996 Oct;24(10):1706-12. % change in renal artery flow Pearson RJ, Barrington KJ, 20 10 0 -10 -20 -30 -40 -50 % change in renal vascular resistance Dopamine and renal perfusion: chronic piglet model 40 30 20 10 0 -10 -20 100 80 60 40 20 0 -20 -40 2 4 8 16 32 Dopamine dosage (g/kg.min) The Pituitary and the blood brain barrier. The pituitary and the anterior hypothalamus are outside of the barrier Dopamine is an important neurotransmitter with endocrine effects Effects of stopping dopamine Dopamine and thyroid suppression in the newborn Filippi L, Cecchi A, Tronchin M, Dani C, Pezzati M, Seminara S, et al. Dopamine infusion and hypothyroxinaemia in very low birth weight preterm infants. Eur J Pediatr 2004 Jan;163(1):7-13. Low dose dopamine = Pituitary dose dopamine Epinephrine, animal data Stimulates α1, α2, β1 and β2 receptors Some evidence that Systemic pressure increase more than pulmonary In standard doses, beta effects predominate (up to 0.2 mcg/kg/min?), high doses will cause vasoconstriction Improves renal perfusion in hypoxic animals Norepinephrine Largely α effects : little β activity(some β1) Seems to cause an NO mediated vasodilatation in certain models of neonatal pulmonary hypertension Pre/Post study in 18 newborns with hypoxic respiratory failure, increased saturations, systemic flow and blood pressure, and increased LPA flow • Pierre Tourneux et al, Pulmonary Circulatory Effects of Norepinephrine in Newborn Infants with Persistent Pulmonary Hypertension J Pediatrics 2008. Dobutamine, animal data Little effect on baseline PA pressures Some evidence of pulmonary vasodilatation (and systemic) if baseline is elevated At high doses PA pressures may increase in hypoxic piglets Cardiac Index (mL/kg.min) Dobutamine response BP only increased at 50 * * * * Systemic blood pressure mean, (mmHg) Baseline 5 Systemic vascular resistance index (mmHg/mL/kg.min) g/kg.min (Cheung and Barrington 1998) Cardiac output increased at 5 g/kg.min and above. Vasodilatation seen at 5 g/kg.min and above. 300 280 260 240 220 200 180 160 140 120 10 20 50 100 95 90 85 80 75 70 65 * Baseline 5 10 20 50 0.6 0.5 * * * * 0.4 0.3 0.2 Baseline 5 10 20 50 Dobutamine dose (g/kg.min) Milrinone, neonatal animal data Specific phosphodiesterase III inhibitor Increases contractility and vasodilates in mature models Effects in neonatal animal models variable, may decrease, have no effect, or slightly increase contractility. Immature subjects react differently Oxygen may be toxic at term also! Lakshminrusimha, 2008, normal lambs Lambs with PPHN (antenatal DA ligation), resuscitated with 100%, 50% or 21% O2 Pulmonary vascular responsiveness examined afterward Initial PVR dropped faster during those ventilated with 100% O2 Pulmonary vasculature was more reactive to hypoxia, and less responsive to NO after O2 resuscitation Human Data? There is no relevant data from human studies to determine whether maintaining higher than normal systemic or alveolar oxygenation is beneficial or harmful Based on the available physiologic data the best approach is to give enough oxygen to achieve systemic normoxia Aiming for higher than normal values risks pulmonary oxygen toxicity, risks impeding pulmonay vasorelaxation Still with me? Summary Oxygen to achieve normoxia Respiratory support to optimize lung volume, ventilation, surfactant... Avoid hyperventilation, bicarbonate, paralysis Cardiovascular support with epinephrine (or norepinephrine? VERY LIMITED DATA) Nitric oxide to reduce RV afterload, improve VQ matching Sedation if required, ? Fentanyl Research to determine whether any of this is true! And to evaluate sildenafil and other therapies Generally: Most babies with PPHN will eventually improve and survive Therefore any uncontrolled study will seem to show benefit EVEN IF THE STUDIED INTERVENTION IS INEFFECTIVE It is vitally important to have controlled trials Why are there so few? The NO studies showed that we are capable of performing such studies A Plea! Controlled prospective studies in PPHN are possible They are essential if we are to progress beyond our current state of knowledge What are the hemodynamic changes in Septic Shock in the newborn? Probably different between G +ve and G-ve infections May not be much different to older children, with vasodilatation in the G-ve, but vasoconstriction and early cardiac dysfunction in the G+ve What is ‘functional hypovolemia’ and how should we treat it? Do all babies with septic shock require large volumes of fluid? – Recent RCT showed worse outcomes with volume administration in children with early septic shock Which inotrope/vasopressor for septic shock? In adults, norepinephrine gives best hemodynamic profile, – little evidence of any difference in clinical outcomes. A ‘one size fits all’ approach is probably inappropriate Individualization of the treatment makes more sense. Septic Shock 30 newborn infants with refractory septic shock Substantial improvement in blood pressure, urine output and pH within 2 hours of starting norepinephrine 2 deaths during acute phase Long term outcomes poor Septic Shock Late onset sepsis – more often G-ve, vasodilatation, hypotension – Consider norepinephrine, ?hydrocortisone Early onset sepsis – Variably G+ve, or –ve – Consider epinephrine, ?hydrocortisone Current Canadian Practice: Hypotension in the ELGAN 120 questionnaires to neonatologists 79% final response – Respondents: 77% from units with > 50 VLBWs pa/ 43% with > 100 VLBWs pa. Criteria for diagnosing hypotension: – 74% use both BP<GA (or another criterion) and clinical signs to define hypotension. – 26% use BP alone, (most common, BP<GA) Responses to Questionnaire: Therapeutic Options Volume 1st-- 97% Dopamine is 1st drug --92% Three main patterns of treatment – volume, dopamine, steroid (37%) – volume, dopamine, dobutamine(28%) – volume, dopamine, epinephrine (16%) 14% have protocols in place Inotropes Dopamine: starting dose range 2.5-10 g/kg/min – maximum dose 10-30 • The maximum dose for 7 respondents is the initial starting dose for 17 others. Dobutamine: starting dose range 2-10 g/kg/min – maximum dose 10-20 Epinephrine: starting dose 0.01-0.1 g/kg/min – maximum dose 0.3-4.0 Steroid usage for BP Usual corticosteroid administered is hydrocortisone (98%). Initial doses varied 0.1–5 mg/kg/dose Total daily doses range from 0.4-15 mg/kg/day. IVH frequency among VLBW infants, Synnes et al 2001 Factors known to be associated with IVH Prematurity Respiratory Support Hypocarbia Illness severity (SNAP-PE) Outborn Not receiving antenatal steroids Adjusted Odds Ratios Synnes et al 2001 Data of the CNN Objective: Compare frequency of diagnosis of hypotension, using 4 different criteria, and the effects of that on relation between hypotension and IVH. Methods: The highest and lowest BP are prospectively recorded for database, n= 16,007 1735 of the infants < 28 wks had head ultrasound data. Results: 14.7% < 28 wks had severe IVH (Gd 3 or 4). Elevated BP- no apparent relationship with IVH. BP<Gestational age Frequently used rule for hypotension, BP (mmHg) < GA (wk), defined 48% of <28wk as hypotensive at some time during day 1. 15.9% of the infants (<28 wk) with lowest recorded mean BP on day 1 < gestational age had a severe IVH. 13.3% of the infants not hypotensive by this rule had severe IVH. Statistically significant (p < 0.05): not very useful! Multivariate analysis, including use of inotropes and SNAP-PE score → no relation between “hypotension” and IVH: OR 1.19, p=NS. Watkins charts Using Watkins charts (10%les) 42,5% of the infants <28 wk classified as being hypotensive – Why not 10%? Cross sectional not longitudinal data, rapidly changing variable More strongly associated with severe IVH (16.5% vs 11.4%): – Association disappeared after correction for use of inotropes. Normotensive infants who received inotropes, (n=150) more severe IVH (17.9%) than hypotensive infants who did not receive inotropes (5.9%). The effects of hypotension Are the adverse outcome effects of hypotension really the adverse effects of its treatment? Alternative explanations: – SNAP does not represent all of the increased risk of IVH? – Other factors associated with both IVH and inotrope use? The association between inotrope usage and IVH appears fairly robust. Mean BP of preterm infants. Watkins et al 1989. 40 38 10 %ile of mean BP 36 500g 600g 700g 800g 900g 1000g 1100g 1200g 1300g 1400g 1500g 34 32 30 28 26 24 22 20 3 12 24 36 48 60 Age (hrs) 72 84 96 Is hypotension related to survival or long term outcomes? Systematic review of the literature, examining 100’s of references, found 16 studies that looked carefully at this issue The answer… Maybe! The majority of studies have shown some correlation between lower BP and poor outcomes BUT Systematic biases in many of them: – For example: same BP used as threshold for all infants (MiallAllen et al 30 mmHg) – If you use the same threshold for everyone, the more immature babies will be more likely hypotensive, and they have the worse outcomes Does treatment of hypotension improve outcomes? Fluid Boluses compared to no intervention Cochrane review – Various fluids: including saline, albumin, plasma substitutes or blood. – 5 studies compared volume to no treatment in patients without cardiovascular compromise. – No controlled trials comparing the use of fluid boluses to no fluid boluses in preterm infants with cardiovascular compromise, specifically hypotension. – Therefore there is no level 1 or 2 evidence to support the use of volume for treatment of hypotension in the premature newborn with hypotension. ?Benefits of fluid boluses 1 short term physiologic study (abstract only) 10 mL/kg 5% albumin to hypotensive preterms, ↑BP 2.7 mmHg LVO↑ ± 20% no effect on RVO – I.E. ductal shunting increased, but no effect on systemic blood flow. Another uncontrolled study: 20 mL/kg of 10% albumin ↑ BP 4 mHg. ↑ LVO, (RVO not measured), left atrial and ventricular distension (but not right) after bolus, – also suggests that ductal shunting increased. Osborn measured SVC flow and RVO in infants with low blood flow, (not necessarily hypotensive, mean BP 26 vs 30). With saline bolus 22% ↑ RVO – Infants all immediately started on an inotrope so duration of effect unclear. Importance of measuring both LVO and RVO LVO & RVO ?Harms of fluid boluses Potential for pulmonary, cardiovascular and CNS complications. – The volume of fluid administered during the first few days of life in the preterm correlates with subsequent development of BPD. This correlation has been confirmed by a prospective controlled trial which demonstrated improved survival and decreased bronchopulmonary dysplasia rates in preterm that were randomized to low fluid intakes versus those given a more liberal fluid intake. – In this study sodium intake was also different between groups Goldberg found an increase in the incidence of IVH in preterm infants receiving rapid volume expansion. ?Harms of fluid boluses Greenough reported adverse neuro. outcomes in patients who received colloid infusion. Multiple fluid boluses associated with increased mortality in the preterm infant. The amount of sodium contained in a single fluid bolus is within the range shown in 2 randomized trials to increase BPD ?Benefits of Inotropes There are 4 trials of dopamine use in the preterm with untreated controls, in none were clinically important outcomes reported, and in none was hypotension required as an entry criterion. Cuevas investigated routine use of low-dose dopamine in ventilated preterm infants, and showed no significant effect on renal function. Systematic review concluded: No evidence that low dose dopamine has favourable effects on renal function, including urine flow and creatinine clearance, or clinical outcomes. 3 studies, investigating effects of dopamine on renal dysfunction due to indomethacin therapy, subject of a Cochrane Systematic Review, no evidence of renal protection from dopamine during indomethacin therapy. Hmmmm ?Harms of inotropes: dopamine Other catecholamines in therapeutic use have no action at the dopamine receptor. Dopamine also stimulates the same receptors in the carotid body leading to a decrease in ventilation and respiratory drive. Dopamine impairs T-cell function. Dopamine increases energy expenditure and lipolysis. ?Harms of inotropes: dobutamine Few toxic effects described Infants may become excessively tachycardic during dobutamine therapy, reduction in dose is usually all that is required. Dobutamine has metabolic effects, – study in lambs showed that any potential benefit of increased oxygen delivery to the tissues was offset by an increase in tissue metabolic rate which “utilized” most of the increased amounts of oxygen delivered to the tissues. No studies of this in the newborn human. ?Harms of inotropes: epinephrine Epinephrine directly impacts lactate metabolism – ↑ in lactate production and ↓ in lactate metabolism, leads to ↑ in serum lactate during epinephrine treatment. At higher doses there may be an impairment of bowel blood flow and oxygen delivery to the gut, this has been seen in some studies of septic adults. Also occurred in acutely instrumented piglets during both normoxia and hypoxia, dose of 3.2 g/kg.min. – Presumably a mediated effect, may not occur at lower doses. Milrinone Phosphodiesterase III inhibitors increase intracellular cAMP: inotropic effects and vasodilatation. In neonatal models PDE III inhibitors have minimal effects, no effect, or even negative inotropic effects. – developmental imbalance between class III and class IV Phosphodiesterase in neonatal sarcoplasmic reticulum. Negative inotropic effects in neonatal puppies become positive in 1st few days after birth. The effects on preterm human myocardium are unknown Milrinone Vasodilatation may occur in newborn mammals (limited studies). In dogs treatment with milrinone at 1 mg/kg produced lesions in the left ventricle and the right atrium. Similar lesions noted with other inotropes; may occur whenever myocardial workload is increased, as this may exceed any increases in myocardial oxygen and substrate supply. Benefits of glucocorticoids Probably increase blood pressure: Gaisssmaier et al compared dexamethasone versus placebo in hypotensive infants starting on an epinephrine infusion. Both groups (total n=17) significant increase in BP at 4 hours: duration of epinephrine use significantly shorter in the steroid treated group. Benefits of glucocorticoids Two studies (abstracts) compared hydrocortisone versus placebo. – 1st randomized 26 “hypotensive” LBW neonates (all on dopamine at 20 g/kg/min) to receive 5mg/kg/day of hydrocortisone in 4 doses: those who received hydrocortisone had a more rapid increase in BP: placebo babies also had a sustained increase in BP. There was no difference in the incidence of IVH. – 2nd randomized 24 neonates <1250 grams “hypotensive” on 1st day of life to hydrocortisone 20mg/kg/day in 4 doses or placebo. There was a statistically significant reduction in the amount of inotrope required. No difference noted in IVH rate, and no long-term data presented. More recent study: randomized preterm infants with mean BP < GA, all receiving ≥ 10 g/kg/min of dopamine after ≥30 mL/kg of normal saline, to 3 mg/kg/d of hydrocortisone for 5 days. Hydrocortisone infants had slightly faster increase in BP, but no clinical differences in outcomes Harms of glucocorticoids Too many slides needed! Short term • Hyperglcemia • GI perforation • GI bleeding Medium term • • • • Decreased growth Decreased brain growth Cardiac hypertrophy Increased sepsis, bacterial and fungal Long term • Impaired neurodevelopment, especially motor function Treatment of Hypotension So why do people treat? « Hypotension impairs cerebral perfusion » « CBF is pressure passive… » Of course if you go to your family Doc for a checkup you aren’t likely to be at significant risk of brain injury with life long consequences! (But you are at risk of complications from intervention) Are any treatments of hypotension better than others? Comparisons of two fluids Comparisons of 2 different fluids have been performed in 4 trials. – 1 compared FFP to albumin in patients with systolic BP < 40 mmHg: no difference in the increase in systolic BP 1 and 4 hours post infusion, no clinically important outcomes were presented. – No long-term data were presented. Three other trials have compared 5% albumin to normal saline. – One found no difference in treatment failure or P/IVH or mortality. – Another found that the blood pressure increase was greater with colloid than crystalloid, but no clinical outcomes were reported. – The third found no difference between fluids but no data on morbidity and mortality were presented. Comparisons of two inotropes 5 studies compare the effects of dopamine versus dobutamine in hypotensive babies Cochrane review concludes dopamine more likely to increase BP than dobutamine but no evidence of a differential effect on clinical outcomes. – 3 had data on mortality, 3 had data on PVL and 2 had data on severe IVH, none of which were significantly different between the two drugs. Comparisons of two inotropes Further study compared dopamine to dobutamine in cases of low systemic flow during 1st twelve h. 42 patients initially received a 10ml/kg normal saline bolus followed by one inotrope or the other. Dopamine increased BP whereas dobutamine increased SVC flow. There was no difference in mortality or other clinically important outcomes In 4 studies comparing dopamine to other inotropes blood flows have been measured. – All 4 showed when dopamine given in sufficient doses to increase BP LVO decreased, by about 20%. In contrast dobutamine increased LVO in two of these studies and SVC flow in the other and epinephrine increased LVO and RVO. – Only Roze et al reported clinically important outcomes, not different between groups. Comparisons of 2 treatment modalities. Cochrane review comparing early volume bolus with dopamine use. Two small randomized unblinded studies: both used albumin. Conclusion: dopamine was more successful than albumin at correcting low BP, but no data on clinically important outcomes. – Lundstrom only enrolled preterm babies with a mean BP 29 to 40 mmHg. – Measured LVO (Doppler) and CBF (intravenous xenon clearance). Blood pressure was increased 20% by dopamine, LVO was increased by 16% and cerebral blood flow was not significantly affected. – I.E. systemic and cerebral vascular resistances were increased by dopamine, RVO not measured, therefore effects on systemic perfusion uncertain. 1 trial compared dopamine with hydrocortisone in hypotensive preterms. No significant difference in improvements in hypotension, no clinically important differences in the short term. Why are preterm babies « hypotensive » Most babies with BP lower than average have acceptable SVC flows Some babies with « normal »BP have low flow Most babies with BP<20 mmHg have low flow. Most « hypotensive » babies have normal flow, but low resistance: do they need any treatment? Figure 3 Scatter plot of mean blood pressure (BP) against superior vena cava (SVC) flow for all observations. Reference lines represent SVC flow of 41 ml/kg/min and mean BP of 30 mm Hg. Osborn, D A et al. Arch. Dis. Child. Fetal Neonatal Ed. 2004;89:F168-F173 Copyright ©2004 BMJ Publishing Group Ltd. Where are we now? Blood Pressure Hypotension or shock? DO2/VO2 Results of retrospective cohort study 118 patients were admitted 2000-2003. BP data were available on 107, 53% of patients had BP < GA. 17/118 ELBW infants received treatment for Hypotension: – 11 received only an epinephrine infusion, – 4 had only a single fluid bolus (saline 10 ml/kg), and – 2 had a fluid bolus followed by epinephrine infusion. 4 other Hypotensive infants received only a blood transfusion, over 2 hr, as therapy. Normotensive Permissive hypotension Treated Hypotension Hypotensive, transfusion only Number 52 34 18 4 Necrotizing enterocolitis, n (%) 4 (8%) 3 (9%) 2 (11%) 2 (50%) Surgical NEC, n 1 1 1 0 Isolated GI perforation, n 2 0 1 0 IVH 3 or 4, n 2 4 5 2 Cystic PVL, n 1 0 0 0 Mortality, n 10 4 13* 2 Survival without severe IVH, cystic PVL, surgical NEC, or GI perforation, n (%) 40 (77%) 26 (76%) 4* (22%) 1 (25%) Results Overall survival of ELBW was 73% 6% of the ELBW infants received a fluid bolus 9% of the ELBW infants received inotropes Results Recent publication shows: – Up to 98% of ELGA infants receive fluid boluses, often multiple times – Up to 78% of ELGA infants receive inotrope infusions, often dopamine – Many ELGA infants are receiving steroids to elevate blood pressure. Our data suggest that most of those babies would do well without intervention. Hypotension without shock Infants who are hypotensive but clinically well-perfused probably have adequate tissue oxygen delivery They have good clinical outcomes They probably do not need any intervention Shock Infants with poor perfusion have poor outcomes May benefit from intervention, but very little data to guide therapy If BP is adequate a vasodilator that supports cardiac function might be the best idea – Dobutamine, low dose epinephrine If BP is low then cardiac support and BP support both may be needed – Moderate dose epinephrine, ?combinations Fluid boluses and stress-dose glucocorticoids might have a role in the presence of shock, especially when due to sepsis, but supportive data entirely based on adult studies – Bacteriology, Hemodynamics, complications completely different Conclusion Very little good data to support evidence based guidelines Hypotensive babies who are well perfused may not need any treatment – As they are treated so frequently in some centers we need good prospective trials to prove whether or not there is a benefit. Babies with poor perfusion do badly, individualizing the interventions, by measurements of relevant physiologic endpoints such as blood flow, serum lactate etc. may help us to improve care.