The Impact of Cataract Surgery on Patients with Low Vision
The Impact of Cataract Surgery in Patients with Low Vision
Irene C. Kuo, MD
Clinical Research Methods
July 23, 2010
Background
• Cataract extraction with intraocular lens implantation
– 1.7 million cases done in
Medicare beneficiaries per annum
Background
• Definition of low vision
– ≤ 20/70 and not correctable
– 14 million Americans
– Age-related macular degeneration, diabetic retinopathy, glaucoma, cerebrovascular accident, albinism
Background
• Aging of population
– Increase of ≥ 5 million Americans ≥ 85 years in next 25 years
– Age-related macular degeneration and glaucoma
• Two leading causes of low vision/blindness
• Prevalence increases with age
Background
• Few publications on benefits of cataract extraction in those with underlying low vision
– Patients may be dissuaded from surgery
• ocular comorbidity
• lengthier evaluation and counseling by surgeon
• Controversy over association between cataract surgery and age-related macular degeneration
– Cataract extraction may accelerate macular degeneration
– Different study designs; may not be causal
Preliminary Data
• Uncontrolled study in Wilmer clinic of prospectively collected data from one surgeon
• 30 eyes of 20 patients with low vision
• Mean change in visual acuity was improvement of 0.25 ± 0.26 (SD) logMAR* units ( 95% CI of the mean change, 0.15 to 0.35 logMAR units; two-tailed p=0.00001)
*LogMAR = log (Snellen visual acuity)
Hypothesis
• Patients with low vision experience a mean improvement in visual acuity of 0.25 logMAR units or greater after cataract surgery compared to patients who do not have surgery.
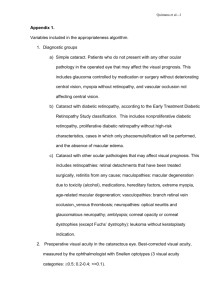
Study population
• Consecutive patients in Low Vision Clinic at Wilmer undergoing evaluation for cataract surgery will be approached to participate.
Methods
• Randomized controlled trial
– Patients will be randomized to have surgery at time 0
(surgical intervention) or 3 months later (delayed surgery)
– 3-month delay in surgery is acceptable, feasible, ethical
– Only one eye per patient will be studied
• Baseline and 3-month visual acuity in logMAR units (log
Snellen visual acuity) will be measured by staff masked to presence or absence of surgical intervention.
• Compare mean change in visual acuity between the intervention groups
Sample size calculation
n = 2 [(z
α
- z
β
) σ / μ
1
– μ
2
] 2 z
α
= 1.96 α = 0.05, β=0.2
z
β
= -0.84
σ = 0.26 logMAR
-> n = 17 patients per group
Sample size calculation
• Stratify patients by 4 major etiologies of low vision:
– age-related macular degeneration
– glaucoma
– diabetic retinopathy
– cerebrovascular accident
4 x 17 patients = 68 patients per group
136 patients total
Data analysis
• Stratification of patients by etiology of low vision
– Two-sample t-test to compare mean change in log
MAR between two intervention groups in each stratum or general linear models to examine differences in mean change for all patients but controlling for etiology
– Which patients benefit the most from surgery?
• Other outcome measures
• Activities of daily living (questionnaire)
• Contrast sensitivity
• Ability to use low vision aids
Discussion
• Natural progression of underlying disease
• Alternative study design
– Randomize each patient by eye (one eye has surgery, the other does not)
– However, activities of daily living are measured at patient (not eye) level.
Significance
• Cataract surgery is highest volume
Medicare procedure
• Aging population with increasing number of persons with low vision and cataracts
• Benefit of cataract extraction in such patients is unknown
Acknowledgements
• Shabina Ahmed, MD
• Kathryn Carson, ScM
• Charles Flexner, MD
• Judit Gordon, MD
• Aaron Horne, MD, MBA
• Ikue Nakayama, MD
• Mary Katherine Nutini, DO
• Dan Ford, MD, MPH