Click here to this slideshow

Cancer-Associated
Thrombosis
Guidelines for Treatment
Professor Mark Levine, MD, MSc
McMaster University
Juravinski Cancer Centre
Hamilton, Ontario, Canada
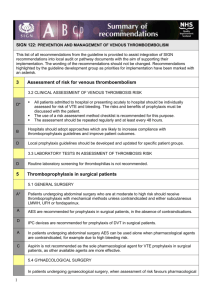
Why do we treat proximal DVT?
– To improve symptoms
– To prevent progression and recurrence
– To prevent pulmonary embolism
– To prevent post-phlebitic syndrome
Why do we treat pulmonary embolism?
– To improve symptoms
– To prevent pulmonary hypertension
– To prevent death
• Patients with pulmonary embolism diagnosed clinically .
• Randomized to heparin 10,000 units Q6H x 6 doses plus concurrent nicoumalone for 14 days
(target PT 2-3x control) or no treatment.
Adapted from Barritt and Jordan Lancet 1960.
• In the 1 st 35 patients, 0 of 16 anticoagulant patients died compared to 5 of 19 control patients, P =0.036 and 5 additional control patients had recurrent PE based on clinical diagnosis.
• 3 minor bleeds on anticoagulant therapy.
• Randomization was discontinued and then 38 additional patients were treated with anticoagulants with no adverse outcomes.
Adapted from Barritt and Jordan Lancet 1960.
Initial Therapy:
Unfractionated or Low Molecular
Weight Heparin?
Depolymerisation of UFH
UFH
Molecular weight =
16,000 Da
DEPOLYMERISATION
LMWH
Molecular weight =
4,500-5,000 Da
High affinity for AT III
Advantages of LMWH over UFH
• Binds less avidly to plasma proteins, platelets, and cells
• Dose-independent renal clearance
• Good bioavailability after sc injection
• Experimentally less bleeding
• Once-daily sc injection
• Weight-adjusted dosing
• No laboratory monitoring
• Less HIT
• Outpatient therapy
HIT = heparin-induced thrombocytopenia; sc = subcutaneous
Initial treatment of VTE LMWH vs UFH
Primary studies
Duroux (1991)
Hull (1992)
Prandoni (1992)
Lopaciuk (1992)
Simonneau (1993)
Lindmarker (1994)
Levine (1996)
Koopman (1996)
Fiessinger (1996)
Luomanmaki (1996)
Columbus (1997)
All studies (FEM)
All studies (REM)
Major bleeding
(n=3,674)
Recurrent thromboembolism
(n=3,566)
0.01
0.1
Favours
LMWH
1
Odds ratio
OR 0.57 (P=0.047)
OR 0.71 (P=0.25)
10 100
Favours
UFH
0.01
0.1
Favours
LMWH
1
Odds ratio
OR 0.85 (P=0.28)
OR 0.87 (P=0.40)
10 100
Favours
UFH
Adapted from Gould et al., Ann Intern Med 1999;130:800-9.
Initial treatment of VTE
Outpatient LMWH vs inpatient UFH
Recurrent
VTE (%)
Major bleeding (%)
UFH n=253
6.7
Levine 1
Enoxap n=247
5.3
Columbus 2 Koopman 3
UFH n=511
Reviparin n=510
UFH n=198
Nadroparin n=202
4.9
5.3
8.6
6.9
1.2
2.0
2.3
3.1
2.0
0.5
Adapted from: 1. Levine et al., N Engl J Med 1996;334:677-81. 2. The Columbus Investigators.
N Engl J Med 1997;337:657-62. 3. Koopman et al., N Engl J Med 1996;334:682-87.
Initial treatment of VTE
Outpatient LMWH vs inpatient UFH (cont’d)
Levine 1 Columbus 2 Koopman 3
UFH n=253
Enoxap n=247
UFH n=511
Hospital days
(mean)
Entirely outpatient treatment
6.5
0.0
1.1
†
49%
9.4
0.0
† Significantly fewer hospital days in LMWH group.
Reviparin n=510
UFH n=198
6.4
†
27%
8.1
0.0
Nadroparin n=202
2.7
†
36%
Adapted from 1. Levine et al., N Engl J Med 1996;334:677-81. 2. The Columbus Investigators.
N Engl J Med 1997;337:657-62. 3. Koopman et al. N Engl J Med 1996;334:682-87.
Cumulative Incidence of Recurrent VTE
During Anticoagulant Therapy
30
Hazard ratio 3.2
20
Cancer
10
No cancer
0
0 1
181
661
160
631
2 3
129
602
4 5 6 7
Time (months)
8
92
161
9
73
120
10 11 12
64
115
Cancer
No cancer
Adapted from Prandoni et al., Blood 2002;100:3484-8.
Cumulative Incidence of Clinically Important
Bleeding During Anticoagulant Therapy
30
20
Cancer
Hazard ratio 2.2
10
No cancer
0
0 1
181
661
170
636
2 3
141
615
4 5 6 7
Time (months)
8
102
170
9
81
127
10 11 12
68
124
Cancer
No cancer
Adapted from Prandoni et al., Blood 2002;100:3484-8.
Oral Anticoagulant Therapy in Cancer Patients
• Warfarin therapy is complicated:
– difficult to maintain tight therapeutic control
(anorexia, vomiting, drug interactions).
– frequent interruptions for thrombocytopenia and procedures.
– venous access difficult.
– increased risk of recurrence and bleeding.
Long-term Anticoagulant Therapy with LMWH
• Does not require laboratory monitoring
• Once- or twice-daily subcutaneous injection
• Effective in warfarin resistance
• Potentially less bleeding
CANTHANOX Trial
• Cancer patients with proximal DVT and/ or PE received initial enoxaparin 1.5 mg/kg subcu daily for at least four days.
• Randomized to continue enoxaparin at same dose or warfarin.
• Duration of therapy was three months.
Adapted from Meyer et al., Arch Intern Med 2002;162,1729.
CANTHANOX
Treatment
LMWH (n=71)
Warfarin (n=75)
P =0.09
5 bleeds in LMWH and 12 in Warfarin
Outcome (recurrent
VTE and/or major bleeding
7 (9%)
15 (20%)
CLOT Trial
Dalteparin Dalteparin
Cancer patients with acute DVT and/or PE
R
Dalteparin Oral anticoagulant
DVT, deep vein thrombosis; PE, pulmonary embolism.
Adapted from Lee et al., NEJM 2003;349:146-53.
CLOT Trial
Group
OAC
LMWH
OAC, oral anticoagulant.
Initial treatment
(5 –7 days)
Dalteparin 200 IU/kg sc once daily
Dalteparin 200 IU/kg sc once daily
Long-term therapy
(6 months)
Warfarin or acenocoumarol
(target INR 2.5)
Month 1: dalteparin 200 IU/kg
Month 2 –6: 75–80% of full dose
Adapted from Lee et al. CLOT Trial 2003
Baseline Characteristics
Female gender
Age, mean (years)
Outpatient
Qualifying VTE
DVT only
PE ± DVT
ECOG score
0
1
2
LMWH
N = 338
179
62
169
235
103
80
135
118
OAC
N = 338
169
63
156
230
108
63
150
122
Baseline Characteristics
Extent of solid tumour no evidence localised metastatic
Haematological malignancy
Cancer treatment
Central venous catheter
Previous VTE
LMWH
N = 338
298
36
39
223
40
266
46
39
OAC
N = 338
308
33
43
232
30
259
40
36
Recurrent VTE
25
20
15
10
5
0
0
Risk reduction = 52%
P=0.0017
OAC
Dalteparin
30 60 90 120 150
Days post-randomization
180 210
Adapted from Lee et al., NEJM 2003;349:146-53.
Bleeding Events
LMWH
N = 336
OAC
N = 336
P *
Major bleed 19 (5.6%) 12 (3.6%) 0.27
Any bleed 46 (13.6%) 62 (18.5%) 0.093
* Fisher’s exact test
Treatment of VTE: Long-term
• Long-term LMWH “simplifies” treatment.
• In the CLOT trial each patient who received oral anticoagulants had on average 23 INRs performed
(maximum 83).
American Society of Clinical Oncology
Guidelines: Treatment of VTE
• What is the best treatment for patients with cancer with established VTE to prevent recurrent VTE
• LMWH is the preferred choice for the initial treatment.
• LMWH given for at least six months is preferred for long term.
• Vitamin K antagonist
INR (2-3) when LMWH not available.
Adapted from JCO 2007;25,5490-505.
Treatment: ASCO
• What is the best treatment for patients with cancer with established VTE to prevent recurrent VTE.
• After six months, indefinite anticoagulant therapy for selected patients with active cancer e.g. metastases.
• IVC Filter only in patients with contraindications to anticoagulant therapy and in those with recurrent VTE despite LMWH therapy.
Adapted from JCO 2007;25,5490-505.
Treatment: ASCO 2007
• What is the best treatment for patients with cancer with established VTE to prevent recurrent VTE.
• For CNS malignancy, same therapy as for other cancers. However avoid anticoagulants if active intracranial bleeding, low platelets, etc.
• For elderly patient with cancer and VTE same approach as for other age groups.
Adapted from JCO 2007;25,5490-505.
ESMO Guidelines
Initial Therapy dalteparin 200 IU/kg daily or enoxaparin 100 IU/kg BID daily or UFH by IV continuous infusion
If severe renal failure
(creatinine clearance < 30),
IV UFH or LMWH monitored by anti Xa monitoring
Thrombolytic therapy in selected patients
Adapted from Ann Oncol 2008.
ESMO Guidelines
Long Term long-term treatment for 6 months with
75 –80% of the initial dose of
LMWH
IVC filter in recurrent PE despite adequate anticoagulant Rx or with a contraindication to anticoagulants
Adapted from Ann Oncol 2008.
Consensus Statement: International Union of
Angiology and Union Internationale de Phlebologie
Initial Therapy
Weight adjusted
LMWH or IV UFH
Secondary Prevention dalteparin LMWH 200
IU/kg subcu for four weeks followed by five months of 75% of dose
Adapted from Int Angiol 2006;25,101-61.
So Where are We in 2008?
Has there been much research progress since 2003 in terms of treatment of VTE in Cancer?
Recurrent VTE
25
20
15
10
5
0
0
Risk reduction = 52%
P = 0.0017
OAC
Dalteparin
30 60 90 120
Days post-randomization
150 180 210
Adapted from Lee et al., NEJM 2003;349:146-53.
Progress in Treatment?
• Can we do better than 8% recurrence at six months?
• Has long term LMWH been adopted?
• What is the duration of long term treatment?
• How should a patient who develops recurrent
VTE on LMWH be treated?