Dental Implant
advertisement
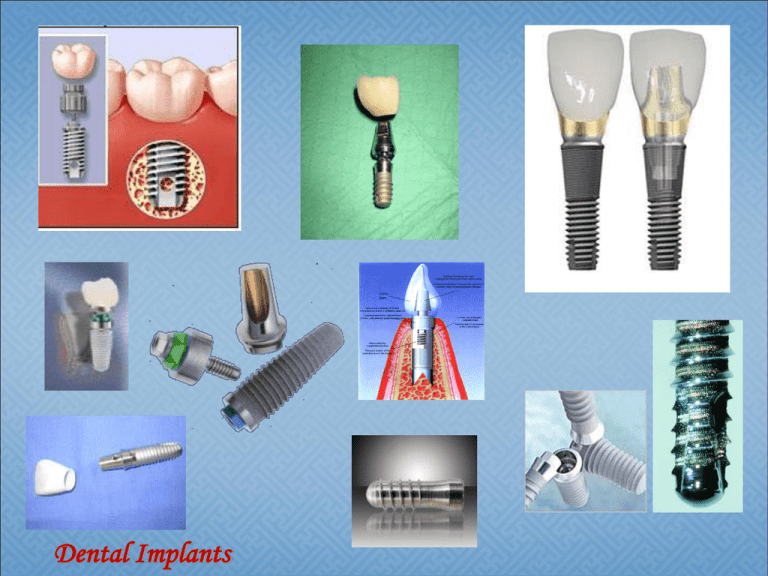
Dental Implants Dental restoration • Important factors: – Performance, durability, longevity and cost of dental restorations – The patient's oral and general health – The components used in the filling material – Where and how the filling is placed – The chewing load Dental amalgam • For the direct filling of decayed lesions or structural defects in teeth • Durable, easy to use, highly resistant to wear and relatively inexpensive in comparison to other materials • Supplied as a powder in bulk, tablet, or predosed capsule form • Combined of – Mercury (supplied as a liquid in bulk, or predosed capsule form), Silver, Tin, Copper • Suppliers: Novo Nordisk, Dentsply International, Lancer Orthodontics, Danaher, Kerr, … Amalgam Advantages. – Used more than any other material to restore carious teeth – Easy to insert into the cavity preparation and adapts readily to cavity walls – In its initial set, or hardness, amalgam allows time for condensing – Has an acceptable crushing strength – Having a long life as a restoration • • Disadvantages – Amalgam's color does not match the color of the teeth – Can not be used on the visible surfaces of anterior teeth – Amalgam will tarnish with time • Highly polished a day or two after its insertion – High thermal conductivity • An intermediate base that will not conduct heat or cold as readily (low thermal conductivity) is placed under the amalgam. FDA Literature Review for Amalgam Safety • In 1997, the U.S. Food and Drug Administration (FDA) and U.S. Public Health Service concluded from a review of nearly 60 peer-reviewed studies that the “data does not support claims that individuals with dental amalgam restorations will experience adverse effects, including neurologic, renal or developmental effects, except for rare allergic or hypersensitivity reactions.” Recently the FDA set out again to update its position on dental amalgam based upon the literature that has been published since the 1997 review. In 2009 they concluded “that there is insufficient evidence to support an association between exposure to mercury from dental amalgams and adverse health effects in humans, including sensitive subpopulations.” http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/DentalProducts/DentalAmalgam/ucm171117.html • Low strength materials prepared by mixing a powder with a liquid • Have lower heat conductivity than do metallic restorative materials • Advantages: – More natural in appearance – Easier and faster to use • Types: – Zinc phosphate cement – Polycarboxylate cement – Glass ionomer cement – Zinc oxide • Disadvantages : – Relatively low strength, varying degrees of solubility in mouth fluids, and setting shrinkage • Clinical Uses: – Zinc phosphate cement is used both as an intermediate base and as a cementing medium. • Intermediate base protects the pulp from sudden temperature changes that may be transmitted by the metallic restoration. • Cementing medium. Zinc phosphate cement is used to permanently cement crowns, inlays, and fixed partial dentures upon the remaining tooth structure. – The cementing medium does not cement two objects together. Instead, the cement fills the space between the irregularities • Chemical Composition. – Powder. The primary ingredients of zinc phosphate cement powder are zinc oxide and magnesium oxide. – Liquid. The liquid used with the powder is phosphoric acid and water in the ratio of two parts acid to one part water. The solution may also contain aluminum phosphate and zinc phosphate. • Uses: – Cementing medium – Intermediate base – Temporary restorative material • Composition – Powder. contains zinc oxide, 1 to 5 percent magnesium oxide, and 10 to 40 percent aluminum oxide – Liquid. Polycarboxylate cement liquid is approximately a 40 percent aqueous solution of polyacrylic acid copolymer with other organic acids such as itaconic acid • Properties – Lower compressive strength than Zinc-Phosphate – Setting reaction produces little heat Unlike zinc phosphate cement • Translucent, tooth-colored materials made of a mixture of acrylic acids and fine glass powders • Used to fill cavities, particularly those on the root surfaces of teeth • Can release a small amount of fluoride (in the case of decay) • Less tooth structure can be removed • Low resistance to fracture – Used in areas not subject to heavy chewing pressure – Used in small non-load bearing fillings • Ionomers experience high wear when placed on chewing surface • Advantages – Inherent adhesion to tooth structure – High retention rate – Little shrinkage and good marginal seal – Fluoride release and hence caries inhibition – Biocompatible – Minimal cavity preparation required hence easy to use on children in and suitable for use even in absence of skilled dental manpower and facilities • Disadvantages – Brittle – Soluble – Abrasive – Water sensitive during setting phase. – Not inherently radiopaque though addition of radiodense additives such as barium can alter radiodensity Composite Fillings • Mixture of glass or quartz filler in a resin medium that produces a tooth-colored filling • Provide good durability and resistance to fracture in small-to- mid size restorations that need to withstand moderate chewing pressure • Less tooth structure is removed when the dentist prepares the tooth, and this may result in a smaller filling than that of an amalgam • The cost is moderate and depends on the size of the filling and the technique used by the dentist • It generally takes longer to place a composite filling than what is required for an amalgam filling • The cavity must be kept clean and dry during filling Composite Resin Fillings (FDA) • The most common alternative to dental amalgam • Sometimes called “tooth-colored” or “white” fillings because of their color • Made of a type of plastic (an acrylic resin) reinforced with powdered glass • Advantages: – Require minimal removal of healthy tooth structure for Placement • Disadvantages: – May be less durable than dental amalgam and may need to be replaced more frequently --Discoloration over time Indirect Restorative Dental Materials • Porcelain-fused-to-metal – Provides strength to a crown or bridge – Very strong and durable – More of the existing tooth must be removed to accommodate the restoration – Highly resistant to wear – Allergic reaction may appear with by the using metals Dental Implantation • Dental extraction: The most frequent surgical procedure performed upon humans • Traumatic, congenital, or metabolic causes So • Denture: the most frequently employed prosthesis – Complete or partial – Fixed • Most desirable – Removable • Most often, because of ease of production as well as economy Complete, removable dentures are the prosthetic replacement used by most edentulous people Alternative Solutions Partial and Full Dentures Crowns Bridges Dental Crowns • In a dental crown the tooth is restored with the help of some material (porcelain) which is lined over the top of a tooth • Are used mostly to repair the look of the teeth Dental Bridges • Multiple crowns fused together Subperiosteal implants – Typically lie on top of the jawbone, but under gum tissues – Do not penetrate into the jawbone – Cobalt based • Endosseous implants – Surgically inserted into the jawbone – Titanium and titanium alloy, aluminum oxide, and surface coatings of hydroxyapatite • Transosseous implants – Surgically inserted into the jawbone – Penetrate the entire jaw – Secured with a device similar to a nut and a pressure plate Severely resorbed, toothless lower jaw bone, which does not offer enough bone height to accommodate Rootform Implants as anchoring devices Bone Grafting • Bone grafting to rebuild reduced jawbone • Fill in jawbone defects allowing the placement of dental implants • Autografts usually the hip • Allografts are taken from human donors • Xenografts are harvested from animals most commonly bovine (cow) • Alloplastic grafts are inert, man made synthetic materials A. Plate-form implant : Made of pure titanium • With one or two metal on one long side like fork • Placed in the jaw to support crowns or bridges Designed for the toothless lower jaw only • Surgically inserted into the jaw bone in three different areas – The left and right back area of the jaw – The chin area in the front of the mouth Endosteal or Endosseous implant C.Root form implant Since the introduction of the Osseointegration concept and the Titanium Screw by Dr. Branemark, these implants have become the most popular implants in the world today. Root form implant shape: Other variations dwell on the shape of the Root form implant. Some are screw-shaped, others are cylindrical, or even cone-shaped or any combination thereof. The two attachments The plate on the bottom is firmly pressed against the bottom part of the chin bone • The long screw posts go through the chin bone • The two attachments that will protrude through the gums can be used to attach an overdenturetypeprosthesis. long screw posts The plate DENTAL IMPLANT • An artificial titanium fixture (similar to those used in orthopedics) • Placed surgically into the jaw bone to substitute for a missing tooth and its root(s). Losing tooth/teeth is not new problem It is possible to replace teeth that look & function like natural teeth Implants is one of the means of achieving this through osseointegration (biological adhesion of bone tissue & titanium) Pioneered by prof. Per-Ingvar Branemark in 1952 ( Swedish orthopedics' surgeon) In 1952, Professor Per-Ingvar Branemark, a Swedish surgeon, while conducting research into the healing patterns of bone tissue, accidentally discovered that when pure titanium comes into direct contact with the living bone tissue, the two grow together to form a permanent biological adhesion named as "osseointegration". Implants do not involve preparation of the adjacent teeth, they preserve the residual bone, and excellent aesthetics can be achieved. However, it is expensive, the patient requires surgery, time consuming, and technically complex. Increasing the support, stability, and patient satisfaction for a full lower denture Increasing the patient's comfort in chewing Increasing the patient's confidence in smiling and speaking Increasing the patient's overall psychological health Replacing one or more teeth as single units with crowns Aesthetics Providing support for a partial denture Biocompatibility of Dental Material Desired Mechanical Properties • High yield strength • Modulus close to that of bone’s • Changes in environment around implant Surfaces • Composition • Ion release • Surface modifications • Problem: – Dental implant surface change with time due to oxidation, precipitation… • Possible solutions: – Oxide layers ( minimize ion release) – Prosthetic component from noble alloys – Phase stabilizers other than Al & V (eg. Ti13Nb-13Zr, Ti-15Mo-2.8Nb ) • Surface Modifications Screw Implants Left to Right: •TPS screw, •Ledermann screw, •Branemark screw, •ITI Bonefit screw Cylinder Implants Left to Right: •Integral, •Frialit-1 step-cylinder, •Frialit-2 step-cylinder First Surgical Phase (Implant Placement) Under Local anesthetic the dentist places dental implants into the jaw bone with a very precise surgical procedure. The implant remains covered by gum tissue while fusing to the jaw bone. Second Surgical Phase (Implant Uncovery) After approximately six months of healing. Under local anesthetic, the implant is exposed and a healing post is placed over top of it so that the gum tissue heals around the post. Prosthetic Phase (Teeth) Once the gums have healed, an implant crown is fabricated and screwed down to the implant. Interface geometry •External – Internal •Hexagonal – Octagonal – Cone •Rotational – non rotational •Height and Width The financial investment is greater. (Single implant costs anywhere from $500 - $6000) Treatment can take up to 9 months. There is a risk of infection and other complications. An implant may loosen and require replacement. Implant procedures may be challenging for some patients. Bruxism is a significant component of failed implants. Patients with certain medical complications should not have implants. Psychological evaluation The dentist assesses the patient's attitude, ability to cooperate during complex procedures, and overall outlook on dental treatment. Dental evaluation The dentist evaluates the condition of the teeth, soft tissues, areas of attached and unattached tissue, and the height and width of the edentulous alveolar bone ridge. (Cont’d) (Cont’d) Medical evaluation The dentist assesses any existing medical conditions that could worsen as a result of the stress of implant surgery. Radiographs Panoramic and cephalometric radiographs, as well as tomograms, are needed to evaluate the height, width, and quality of bone. Definition: A time-dependant healing process where by clinically symptomatic rigid fixation of alloplastic materials is achieved, and maintained, in bone during functional loading. (Zarb & Albrektson,1991) 1. 2. 3. 4. 5. 6. Implant biocompatibility Implant design Implant surface Implant bed Surgical technique Loading condition Materials used are: Cp titanium (commercially pure titanium) Titanium alloy (titanium-6aluminum-4vanadium) Zirconium Hydroxyapatite (HA), one type of calcium phosphate ceramic material Osseointegration interface: Osseointegration Biointegration Cylindrical Implant Some investigators explain the lack of bone steady state by overload due to micromovement of the cylindrical design, whereas others incriminates an inflammation/infection caused particularly by the very rough surfaces typical for these types of implant. Threaded Implant In contrast, Threaded implants have demonstrated maintenance of a clear steady state bone response. To enhance initial stability and increase surface contact, most implant forms have been developed as a serrated thread. Pitch, the number of threads per unit length, is an important factor in implant osseointegration. Increased pitch and increased depth between individual threads allows for improved contact area between bone and implant. Moderately rough surfaces with 1.5µm also, improved contact area between bone and implant surface. Reactive implant surface by anodizing (Oxide layer), acid etching or HA coating enhanced osseointegration Minimal tissue violence at surgery is essential for proper osseointegration. Careful cooling while surgical drilling is performed at low rotatory rates Use of sharp drills Use of graded series of drills Proper drill geometry is important, as intermittent drilling. The insertion torque should be of a moderate level because strong insertion torques may result in stress concentrations around the implant, with subsequent bone resorption. Delayed loading: 1. A tow-stage surgical protocol 2. One-stage surgical protocol Immediate loading: 1. Immediate occlusal loading (placed within 48 hours postsurgery) 2. Immediate non-occlusal Loading (in single-tooth or short-span applications) 3. Early loading (prosthetic function within two months) How many teeth are missing? What is the degree of bone loss? Are the remaining teeth in a good position and do they have a long-term prognosis? What does the patient expect for an end result? What treatment will result in the best cosmetic outcome? What is the patient's budget? I. II. III. The evaluation of a patient as a suitable candidate for implants should follow the same basic format as the standard patient evaluation, although some areas require additional emphasis and attention: Medical History. Psychological Status. Dental History. The greater the surface area of the implant-bone system, the less concentrated the force transmitted to the crest of bone at the implant interface. Similarly, the greater the surface area of the implant-bone system, the better the prognosis for the implant. For each 0.25 mm increase in diameter, the surface area of a cylinder increases by more than 10 per cent; For each 3.0 mm increase in length , the surface area of a cylinder increases by more than 10 per cent. Ideally, occlusal forces should be directed along the long axis of the implants. Therefore ,The angle of the osseous ridge crest is a key determinant of implant angulation. the distance between an implant and any adjacent "landmark" (natural tooth or another implant), which should be not less than 2.0 mm. The number of implants, their respective lengths and locations, the quality of bone support, the posterior ridge anatomy, occlusal forces, and the opposing dentition are of greater importance in determining the appropriate cantilever than a suggested formula. One method is to draw a line through the most anterior implant, and another through the two most posterior implants. The distance between the two lines can then be measured. A suggested maximum cantilever would be 1.5 times this distance. Dr,salah hegazy Dr,salah hegazy Dr,salah hegazy Dr,salah hegazy









