APRV
advertisement

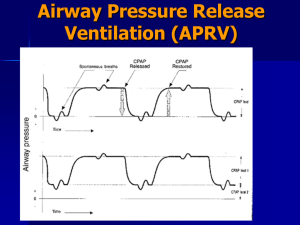
Airway Pressure Release Ventilation Muhammad Asim Rana In patients with acute lung injury (ALI) and ARDS, conventional mechanical ventilation (CV) may cause additional lung injury from overdistention of the lung during inspiration, repeated opening and closing of small bronchioles and alveoli, or from excessive stress at the margins between aerated and atelectatic lung regions. Increasing evidence suggests that smaller tidal volumes (VTs) and higher end-expiratory lung volumes (EELVs) may be protective from these forms of ventilator-associated lung injury and may improve outcomes from ALI/ARDS. APRV was introduced to clinical practice about 2 decades ago as an alternative mode for mechanical ventilation; however, it had not gained popularity until recently as an effective & safe alternative for difficult to ventilate/oxygenate patients of ALI/ARDS What is APRV APRV was introduced initially by Stock & Down in 1987 as a CPAP with an intermittent release phase APRV applies CPAP (P high) for a prolonged time (T high) to maintain adequate lung volume & alveolar recruitment, with a time cycled release phase to a lower set of pressure (P low) for a short period of time (T low) or (release time) where most of the ventilation & CO2 removal occurs The transition from P high to P low deflates the lungs and eliminates carbon dioxide. Conversely, the transition from P low to P high inflates the lungs. Alveolar recruitment is maximized by the high continuous positive airway pressure The difference between P high and P low is the driving pressure. Larger differences are associated with greater inflation and deflation, while smaller differences are associated with smaller inflation and deflation. The exact size of the tidal volume is related to both the driving pressure and the compliance. T high and T low determine the frequency of inflations and deflations. As an example, a patient whose T high is set to 12 seconds and whose T low is set to 3 seconds has an inflationdeflation cycle lasting 15 seconds. This allows 4 inflations and deflations to be completed each minute. Spontaneous breathing is possible at both P high and P low, although most spontaneous breathing occurs at P high because the time spent at P low is brief. This is a novel feature that distinguishes APRV from other types of IRV. If the patient has no spontaneous respiratory effort, APRV becomes typical to “inverse ratio pressure limited, time cycle-assisted mechanical ventilation (pressure control ventilation). In ARDS the functional residual capacity & lung compliance are reduced, & thus the elastic work of breathing is elevated. By applying CPAP, the FRC is restored & inspiration starts from a more favorable pressure-volume relationship, facilitating spontaneous ventilation & improve oxygenation. Applying ‘P high’ for a ‘T high’ (80-95% of the cycle time), the mean airway pressure is increased insuring almost constant lung recruitment (open lung approach), in contrast to the repetitive inflation & deflation of the lung using conventional ventilatory methods (which could ventilator induced lung injury), or the recruitment maneuvers which have to be done frequently to avoid derecruitment. Mean air way pressure on APRV is calculated using this formula: (P High х T High) + (P Low х T Low) (T High + T Low) Minute ventilation & CO2 removal in APRV depend on lung compliance, airway resistance, the magnitude & duration of pressure release and the magnitude of patient’s spontaneous breathing efforts. Spontaneous breathing plays a very important role in APRV allowing the patient to control his/her respiratory frequency without being confined to an arbitrary preset I:E ratio, thus improving patient comfort & patient-ventilator synchrony with reduction in the amount of sedation necessary. Additionally, spontaneous breathing helps derive the inspired gas to the nondependent lung regions by using patients own respiratory muscles & through pleural pressure changes without raising the applied airway pressure to a rather dangerous level, as in conventional mechanical ventilation, producing more physiological distribution to the non dependent lung regions & improving V/Q matching Adding Pressure Support to APRV The addition of PSV above P High to add spontaneous breaths is feasible, but this addition contradicts limiting the airway pressure & may cause significant lung distention. Furthermore, the imposition of PSV to APRV reduces the benefits of spontaneous breathing by altering the normal sinusoidal flow of spontaneous breathing Advantages of APRV APRV has not been shown to improve mortality. However, it may improve alternative important clinical outcomes compared to other modes of ventilation. In one trial, 30 patients being mechanically ventilated because of trauma were randomly assigned to receive APRV alone or pressure-limited ventilation for 72 hours followed by APRV. The APRV alone group had a shorter duration of mechanical ventilation, a shorter ICU stay, and required less sedation and pharmacologic paralysis. Mortality did not differ between groups. Effects on Oxygenation The improved oxygenation parameters i.e., PaO2/FiO2 & lung compliance are attributed to the beneficial effects of spontaneous breathing through better gas distribution & better V/Q matching to the poorly aerated dorsal regions of the lungs, along with higher mean airway pressure obtained compared to conventional ventilation. Effects on hemodynamics During spontaneous breathing the pleural pressure decreases leading to a decrease in intra thoracic & Rt atrial pressure thus improving venous return & improving o\pre load and consequently increasing the cardiac out put. Kaplan compared the hemodynamics effects in patients with ALI/ARDS on patients APRV vs IRV PCV; they found significantly higher cardiac index, oxygen delivery, mixed venous oxygen saturation, urine output & significantly lower vasopressors & inotropes usage, lactate concentration & CVP while on APRV Putnsen found same results in a separate study Effects on regional blood flow & organ perfusion In a study by Hering APRV improved respiratory muscle blood flow in 12 pigs with ALI In a similar study by same author APRV showed improved blood flow to stomach duodenum, ileum & colon Kaplan found significant improvement in GFR in pts on APRV Effects on sedation The level of sedation & analgesia required in CMV is usually equivalent to Ramsay score of 45, but during APRV a Ramsay score of 2-3 can be targeted APRV has shown to decreased the need of neuromuscular blockade use by 70% & use of sedation by about 40% compared to conventional ventilation Duration of ICU stay The decreased use of sedatives & neuromuscular blockade may translate into decreased length of mechanical ventilation & ICU length of stay Indications ARDS/ALI Atelactasis after major surgery Pulmonary edema Obesity/Ascities PIP>35 & PEEP> 10 cm of water Contraindications Increased Air way resistance Patients of COPD & Asthma Theoretically, using short release time is not beneficial for patients who require long expiratory time Because of lower levels of sedation used to allow spontaneous breathing APRV should not be used in patients who require deep sedation for management of their underlying disease (e.g.cerebral edema with increased ICP or status epilepticus) Likewise use of APRV has not been investigated in patients with neuromuscular disease & is not supported by any evidence Setting APRV Mechanical ventilation with PEEP titrated above the lower infliction point of the static pressure volume curve & a low tidal volume at 6 ml/kg are thought to prevent alveolar collapse at end expiration and over distension of lung units at end-inspiration in patients with ARDS. This is lung protective strategy. The setup at the bed side is simple and the goals are same: To maintain adequate oxygenation & ventilation without overt lung distention during P high & avoiding lung derecruitment during P low Setting Pressures P high should be below the high inflection point on the static volume-pressure curve, while P low should be above the low inflection point on the same curve Setting Time T high should allow complete inflation of the lungs, as indicated by end-respiratory phase of no flow when spontaneous breathing is absent, & T low should allow for complete exhalation with no flow at the end to assure absence of intrinsic or auto PEEP Initial setup & transition from conventional ventilation P high is usually set between 20 & 30 P low is set between 0 & 5 cm of H2O T high is 4 to 6 seconds T low is 0.2 to 0.8 seconds TROUBLESHOOTING Maneuvers to correct poor oxygenation 1) increase either ‘P high’, ‘T high’ or both to increase mean airway pressure; 2) change the patient position to the prone position along with the APRV. Maneuvers to correct poor ventilation 1) increase ‘P high’ and decrease ‘T high’ simultaneously to increase minute ventilation while keeping stable mean airway pressure (preferred method); 2) increase ‘T low’ by 0.05-0.1 s increments; 3) decrease sedation to increase the patient’s contribution to minute ventilation. Acknowledgements Dr. Mostafa Adel Dr. Omar Alsayed Dr. Ahmed fouad Dr. Ahmed Hossam Dr. Ahmed Rajab Dr. Sameer Ibrahim Dr. Bashir Ahmed Dr. Sayed Afzal Thank you For patient listening