bivent-pitts
advertisement

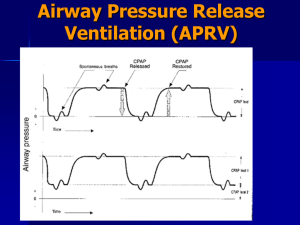
The “How To” of BiVent (APRV) David Pitts II, RRT Clinical Applications Specialist, Maquet Birmingham, Alabama Sponsored by Maquet, Inc – Servo Ventilators Objectives Provide the definition and names for APRV Explain the four set parameters. Identify recruitment in APRV using exhaled CO2. Recommend appropriate initial settings for APRV Make adjustments based on arterial blood gas results Discontinue ventilation with APRV Lung Protective Strategies Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) Keep plateau pressures < 30 cm H2O Use low tidal volume ventilation (4-6 mL/kg IBW) Use PEEP to restore the functional residual capacity (FRC) Keeping Plateau Pressure < 30 cm H20 What do you do if CO2 is rising and the plateau pressure is at 30 cm H2O? Alternative Techniques Increase the ventilator rate Permissive Hypercapnia Airway Pressure Release Ventilation High Frequency Ventilation Extracorporeal Life Support Indications Primarily used as an alternative ventilation technique in patients with ARDS. Used to help protect against ventilator induced lung injury. Goal To provide the lung protective ventilation supported by the ARDSnet research. Use an “Open lung” approach. Minimize alveolar overdistension. Avoid repeated alveolar collapse and reexpansion. Restore FRC through recruitment and, Maintain FRC by creating intrinsic PEEP. APRV Description A mode of ventilation along with spontaneous ventilation to promote lung recruitment of collapsed and poorly ventilated alveoli. The CPAP is released periodically for a brief period. The short release along with spontaneous breathing promote CO2 elimination. Release time is short to prevent the peak expiratory flow from returning to a zero baseline. Ventilation With APRV The short release along with spontaneous breathing promote CO2 elimination. Release time is short to prevent the peak expiratory flow from returning to a zero baseline. APRV AKA BiVent – Servo APRV – Drager BiLevel – Puritan Bennett APRV – Hamilton Etc. Consider APRV when the Patient Has - Bilateral Infiltrates PaO2/FIO2 ratio < 300 and falling Plateau pressures greater than 30 cm H2O No evidence of left heart failure (e.g. PAOP of 18 mm Hg or greater) In other words, persistent ARDS Possible Contraindications Unmanaged increases in intracraneal pressure. Large bronchopleural fistulas. Possibly obstructive lung disease. Technically, it may be possible to ventilate nearly any disorder. Terminology P High – the upper CPAP level. Analogous to MAP (mean airway pressure) and thus affects oxygenation PEEP (Also called Plow) is the lower pressure setting. T High- is the inspiratory time IT(s) phase for the high CPAP level (P High). T PEEP or T low- is the release time allowing CO2 elimination Terminology T High plus T PEEP (T low) is the total time of one cycle. I:E ratio becomes irrelevant because APRV is really best thought of as CPAP With occasional releases Bi-Vent Set-up Screen Advantages of APRV Uses lower PIP to maintain oxygenation and ventilation without compromising the patient’s hemodynamics (Syndow AJRCCM 1994, Kaplan, CC, 2001) Shown to improved V/Q matching (Putensen, AJRCCM, 159, 1999) Required a lower VE suggesting reduced VD/VT (Varpula, Acta Anaesthesiol Scand 2001) Compared to PCIRV – Advantages of APRV APRV uses lower peak and mean airway pressures, Increases cardiac index, Decreases central venous pressure, Additional Advantages Compared to PCIRV APRV increases oxygen delivery and Reduces the need for sedation and paralysis APRV also improves renal perfusion and urine output when spontaneous breathing is maintained. (Kaplan, Crit Care, 2001; Hering, Crit Care Med 2002) New Water Coolers are Being Installed in the ICU Waiting Rooms Advantages of Spontaneous Breathing The benefits of APRV may be related to the preservation of spontaneous breathing. Maintaining the normal cyclic decrease in pleural pressure, augmenting venous return and improving cardiac output. (Putensen, AJRCCM, 1999) The need for sedation is decreased. Preserve Spontaneous Breathing The dashed line in each figure represents the normal position of the diaphragm. The shaded area represents the movement of the diaphragm. (Froese, 1974) Spontaneous v.s. Paralyzed Spontaneous breathing provides ventilation to dependent lung regions which get the best blood flow, as opposed to PPV with paralyzed patients. ((Frawley, AACN Clinical 2001. Froese, Anesth, 1974). Spontaneous v.s. Paralyzed During PPV (paralyzed patient), the anterior diaphragm is displaced towards the abdomen with the nondependent regions of the lung receiving the most ventilation where perfusion is the least. Try as we might. We can’t get away from it? Other Advantages of Spontaneous Breathing Reduces atrophy of the muscles of ventilation associated with the use of PPV and paralytic agents. (Neuman, ICM,2002) Another Advantage During PPV atelectasis formation can occur near the diaphragm, when activity of this muscle is absent. (paralysis) However, if spontaneous breathing is preserved, the formation of atelectasis is offset by the activity of the diaphragm. (Hedenstierna, Anesth, 1994) Initial Settings – P High P High – Set a plateau pressure (adult) or mean airway pressure (pediatric) Typically about 20-25 cm H2O. In patients with Pplateau at or above 30 cm H2O, set at 30 cm H2O Setting Phigh Over-distention of the lung must be avoided. Maximum Phigh of 35 cm H2O. (controversial) Exceptions for higher settings – morbid obesity, decreased thoracic or abdominal compliance (ascites). Setting Thigh The inspiratory time (Thigh) is set at a minimum of about 4.0 seconds In children, others use lower settings (Children’s Med Ctr. Uses 2 sec.) Thigh is progressively increased (10 to 15 seconds (Habashi, et al) Target is oxygenation. Setting Thigh Progress slowly. For example, 5 sec Thigh to 0.5 sec Tlow, a 10:1 ratio. Increasing to 5.5 sec to 0.5 sec is an 11:1 ratio; not a big change. Old patients may be fragile. APRV Release Time - TPEEP Currently, with ARDS thinking is not to let exhalation go to complete emptying, i.e. do not let expiratory flow returning to zero. (McCunn, Crit Care 2002) Thus, regional auto-PEEP a desirable outcome with APRV FLOW Setting PEEP or Plow in APRV Set PEEP at zero cm H2O. This provides a rapid drop in pressure, and a maximum DP for unimpeded expiratory gas flow. (Frawley, AACN Clin Issues 2001) Avoid lung collapse during Tlow. Establishing T PEEP (Time at low pressure) Set T PEEP (T low) so that expiratory flow from patient ends at about 50 to 75% of peak expiratory flow. This can be determine saving a screen and calculating peak expiratory flow. Or, it can be estimated Expiratory Flow T PEEP – Setting The Time Adults 0.5 to 0.8 seconds Pediatric/neonatal settings 0.2 to 0.6 seconds. Or one time constant. (TC = C x R) T PEEP – Using the Tc Release Time in ARDS Atelectasis can develop in seconds when Paw drops below a critical value in the injured lung. (Neumann P, JAP 1998, Newmann P, AJRCCM 1998, Frawley, 2001; McCunn, Internat’l Anesth Clinics 2002). Too long a release time would interfere with oxygenation and allow lung units to collapse. Rat Lung Model – Dr. Slutsky Initial Settings P high 20-30 cm H2O, according to the following chart. P/F <250 <200 <150 MAP 15-20 20-25 25-28 T high range 4-6 sec. T low = 0.5 sec and P low = 0 T High/T low- 12-16 releases T High (s) T low (s) Freq. 3.0 0.5 17 4.0 0.5 13 5.0 0.5 11 6.0 0.5 9 PS- as indicated with special attention given to PIP. Bi-Vent Settings Set Releases and I:E Create releases and I:E Bi-Vent Ventilation P High T PEEP T High Spontaneous Breathing Spontaneous Breaths (On P High) Patient Trigger (On P High) Spontaneous Breathing w/PS Spontaneous Breaths w/PS Identifying Lung Recruitment – CO2 Monitoring Making Changes in APRV Settings Based on ABGs Control Settings for CO2 DP (Phigh – Plow) determines flow out of the lungs and volume exchange (VT and PaCO2). Some clinicians suggest a target minute ventilation of 2 to 3 L/min. (Frawley, 2001). Optimize spontaneous ventilation. CO2 Elimination To Decrease PaCO2: Decrease T High. – – – – Shorter T High means more release/min. No shorter than 3 seconds Example: T High 5 sec. = 12 releases/min T High 4 sec = 15 releases/min Increase P High to increase DP and volume exchange. (2-3 cm H2O/change) – Monitor Vt – PIP (best below 30 cm H2O) Check T low. If possible increase T low to allow more time for “exhalation.” To Increase PaCO2 Increase T high. (fewer releases/min) Slowly! In increments of 0.5 to 2.0 sec. Decrease P High to lower DP. – Monitor oxygenation and – Avoid derecruitment. It may be better to accept hypercapnia than to reduce P high so much that oxygenation decreases. Management of PaO2 To Increase PaO2 1. Increase FIO2 2. Increase MAP by increasing P High in 2 cm H2O increments. 3. Increase T high slowly (0.5 sec/change) 4. Recruitment Maneuvers 5. Maybe shorten T PEEP (T low) to increase PEEPi in 0.1 sec. increments (This may reduce VT and affect PaCO2) Going Too Fast Weaning From APRV 1. 2. 3. FiO2 SHOULD BE WEANED FIRST. (Target < 50% with SpO2 appropriate.) Reducing P High, by 2 cmH20 increments until the P High is below 20 cmH2O. Increasing T High to change vent set rate by 5 releases/minute Weaning From APRV 3. 4. The patient essentially transitions to CPAP with very few releases. Patients should be increasing their spontaneous rate to compensate. During Weaning Add Pressure Support judiciously. Add Pressure Support to P High in order to decrease WOB while avoiding overdistention, P High + PS < 30 cmH2O. Pressure Support with APRV Weaning Bi-Vent Lower Rate Longer T High Lower P High Add PS Weaning Bi-Vent Lower Rate Longer T High Add PS Lower P High Weaning- Habashi method: Drop-and-Stretch Perceived Disadvantages of APRV APRV is a pressure-targeted mode of ventilation. Volume delivery depends on lung compliance, airway resistance and the patient’s spontaneous effort. APRV does not completely support CO2 elimination, but relies on spontaneous breathing Disadvantages of APRV With increased Raw (e.g.COPD) – the ability to eliminate CO2 may be more difficult – Due to limited emptying of the lung and short release periods. If spontaneous efforts are not matched during the transition from Phigh to Plow and Plow to Phigh, may lead to increased work load and discomfort for the patient. Limited staff experience with this mode may make implementation of its use difficult. The End Thank You!