Porter Slide Presentation - University of Pennsylvania School of
advertisement

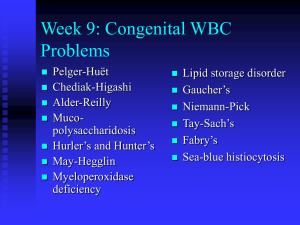
Disorders of Cholesterol Homeostasis Niemann-Pick disease, type C • Autosomal recessive, progressive, lethal, neurodegenerative disorder due to mutation of either NPC1 or NPC2 • Endolysosomal storage of unesterified cholesterol and lipids • Incidence: 1/100,000-120,000 • No FDA approved therapies Niemann-Pick Disease, type C1 • Variable phenotype and age of onset – Classical Disease: Late-infantile and juvenile (60-70%) – Infantile (20%) – Adult • Late-infantile and juvenile (classical) – Transient neonatal jaundice – Splenomegaly – Neurological symptoms (insidious onset) • • • • • Vertical supranuclear ophthalmoplegia Cerebellar ataxia and dysfunction Cognitive impairment and dementia Gelastic cataplexy Seizures Niemann-Pick Disease, type C1 • Therapeutic trial issues – Rare Disease – Heterogeneous phenotype • Variable age of onset • Variable symptom complex – Clinical progression occurs over years – Goal: Stabilization or delay of neurological disease – Optimal treatment may be prior to the onset of neurological signs and symptoms – Significant diagnostic delay – Lack of defined and accepted outcome measures Niemann-Pick disease, type C1 • 78 patients enrolled since August 2006 – Age range: 3 months to 54 years (median 10 years) – NPC1 Neurological Severity (range 0-50, median 14) – Miglustat therapy (42%) • Goals: Severity Score • Natural History Trial 40 20 0 10 20 30 40 Age (years) – Identify clinical or biochemical markers that can be used as an outcome measure in a therapeutic trial – Identify a biochemical marker that can be used for diagnostic testing or screening 50 Niemann-Pick Disease, type C1 Mean Diffusivity Volume Niemann-Pick Disease, type C Biomarker Development (Assembling a Tool Box) Niemann-Pick disease, type C1 • Biomarkers – Insight into pathology – Diagnostic/screening test – Tools to guide therapeutic trials • Biomarker identification – – – – Candidate proteins/lipids Multi-analyte profiling Expression analysis Proteomics Oxysterols Blood-based diagnostic test Niemann-Pick Disease, type C • Filipin Staining – Fluorescent antibiotic that binds unesterified cholesterol – Specialized testing – Requires a skin biopsy-invasive – Variable staining Filipin Staining Control NPC Vanier and Millat (2003) Clin Genet. 64: 269-281 • 80-85% “classical” • Molecular Testing – Expensive and requires a high index of suspicion – ~80% sensitive • 4-5 year diagnostic delay Dan Ory (personal communication) NPC1: Clinical Science • Oxysterols – Hypothesis: In NPC1 the unique combination of increased oxidative stress and intracellular accumulation of unesterified cholesterol will result in increased nonenzymatic oxysterols. Intracellular Cholesterol Accumulation in NPC1 Decreased Serum Antioxidant Capacity in NPC1 Subjects TEAC (mM) 10 8 6 n=40 p<0.0001 4 2 0 n=40 Control NPC Fu et al (2010) MGM, 101:214 Niemann-Pick Disease, type C1 Plasma Oxysterols 3β,5α,6β-cholestane-triol 7-ketocholesterol 3β,5α,6β-cholestane-triol 7-ketocholesterol Porter et al. (2010) STM, 2: 56ra81 Niemann-Pick Disease, type C1 Triol (24.5 ng/ml) Sensitivity 97% Specificity 100% Porter et al. (2010) STM, 2: 56ra81 Jiang et al. (2011) JLR, 52:1435 Niemann-Pick Disease, type C1 CSF Protein Biomarkers Niemann-Pick Disease, type C1 +/+ Calbindin ng/mL Calbindin D 20 15 p<0.001 10 5 0 -/- Control NPC1 Calbindin (ng/mL) 20 15 p=0.28 10 5 0 Control Untreated Treated Niemann-Pick Disease, type C Calbindin Percent Change +/- miglustat Serial Calbindin pre/post miglustat 30 20 Percent Change 15 10 5 10 0 -10 p<0.05 -20 -30 n=16,15,5 A B Miglustat C D e- ed ea t Months pr -50 30 tr 20 d 10 ea te 0 po st -40 0 un tr Calbindin ng/mL 20 Untreated Treated Pre/post B/A D/C C/B Niemann-Pick disease, type C1 • Fatty Acid Binding Protein 3 (FABP3) 62 62 59 59 Npc1+/+ Npc1-/p<0.0001 CSF Percent change FABP3 FABP3 (ng/ml) 100 40 80 p<0.0001 60 40 20 0 Controls NPC p=0.05 20 0 -20 untreated treated -40 -60 -80 pre/post miglustat Niemann-Pick disease, type C1 • Macrophage Inflammatory Protein 1-alpha (Mip1α, CCL3) – Proinflammatory cytokine – Activated microglia 30 CSF Mip1alpha (pg/mL) Mip1 (pg/mL) 30 p<0.0001 20 10 0 25 20 15 10 5 0 Control NPC 0 10 20 30 40 50 60 Severity Score Ranking Control 4.8 ± 1.9 pg/ml NPC 14.7 ± 4.2 Confidential CSF Biomarkers • CSF Biomarkers – Lipid-based • 3β,5α,6β-cholestane-triol and cholesterol esters – Protein-based • Markers of inflammation – MIP-1α, IL1a, IL3, IL4, IL12p40, IL13, IL15, and MMP2 • Markers of neuronal injury – Aβ(42), phosphorylated tau, fatty acid binding protein 3 (FABP3), and calbindin-D • Markers of oxidative stress – glutathione S-transferase alpha (GSTα) and superoxide dismutase 1 (SOD1) 2-Hydroxypropyl-β-cyclodextrin NPC1 HPβCD Trial • 2-Hydroxypropyl-β-cyclodextrin (HPβCD) – Cyclic oligosaccharide with a hydrophobic core – Pharmaceutical excipient • Drug repurposing NPC1 HPβCD Trial • Npc1 mouse model Survival Ramirez et al. (2010) Ped. Res. 68: 309 Cerebellar pathology: 49-days Npc1+/+ Npc1-/- Npc1-/- + CD Liu et al. (2009) PNAS 106: 2377 NPC1 HPβCD Trial • Npc1 cat model – 24 week Npc1 mutant cats (HPβCD, miglustat, untreated) Personal Communication: Charles Vite NPC1 HPβCD Trial • HPβCD Therapeutic trial – Pilot project for TRND/NCATS • Goal: Improve drug development for rare and neglected diseases – HPβCD does not cross the blood-brain barrier – Dose limiting toxicity: Ototoxicity • Cat, dog, and mouse NPC1 HPβCD Trial Lancet (1963) 282: 983-984 Risks Bleeding/strokes Infection Seizure NPC1 HPβCD Trial • Phase 1 trial – Goal: Establish a safe and biochemically effective dose – Cohort dose-escalation • Safety • Pharmacokinetics – Quantitative and validated assay for HPβCD • Pharmacodynamics (Biochemical efficacy) – Quantitative and validated assays for 24-hydroxycholesterol • Pathological efficacy – CSF protein and lipid biomarkers NPC1 HPβCD Trial • Pharmacodynamic response • Plasma 24(S)-hydroxycholesterol Neuron Cholesterol Synthesis ApoE NPC1 HPβCD CYP46 24(S)HC CSF 24(S)HC Blood NPC1 HPβCD Trial • Pharmacodynamic response • Plasma 24(S)-hydroxycholesterol Neuron Cholesterol Synthesis ApoE NPC1 HPβCD CYP46 24(S)HC CSF 24(S)HC Blood NPC1 HPβCD Trial Saline CSF and Plasma Sampling (0 to 72 hours) HPβCD CSF and Plasma Sampling (0 to 72 hours) • Baseline standard deviation of the saline area under the curve (AUC) estimated by resampling (bootstrapping) • Biochemical response defined as: – In an individual patient the difference between the drug and saline AUC greater than 2.3 x SD is considered a positive response – Positive response observed in at least 2 out of 3 patients NPC1 HPβCD Trial • 50 mg HPβCD – No drug related adverse events or reactions – AUC8-72 • Patient 1 + 3.1 x sd • Patient 2 + 0.8 x sd • Patient 3 + 4.1 x sd • P. acnes – Infection/Colonization Plasma 24-OH Cholesterol (ng/ml) • 2/3 patients had a biochemical response Saline 50 mg 35 30 25 0 12 24 36 48 Time (hours) 60 72 Niemann-Pick disease, type C1 • ICV versus lumbar IT • Dose escalation response • Repetitive dosing response: Attenuation • Response of other biomarkers • Safety-Ototoxicity Cohort Dose-escalation Not Tolerated Cohort 1 50 mg Dose STOP Not Tolerated Tolerated No Response Cohort 3 Cohort 1/2 200 mg Dose Cohort 1/2/3 300 mg Tolerated Biochemical Response Tolerated Biochemical Response Tolerated No Response Cohort 3/4 400 mg Cohort 1/2 Maintain 200 mg Maintain 300 mg Maintain 400 mg Niemann-Pick disease, type C1 • No significant response at 50 and 200 mg IT • Positive response in 2/3 subjects at 300 mg IT – Response similar to 50 mg ICV – Grade 1 Ototoxicity in 2 subjects (siblings) • 400 mg cohort completed this week Niemann-Pick disease, type C1 • Clinical efficacy trial • Multicenter: Funding and IRB complexity • Multinational: Funding, IRB and regulatory complexity • NeuroNext Network – Concept proposal accepted • Clinical outcome measures – Ataxia (Cerebellar Function) • Gross motor • Fine motor – Swallowing 26 US Sites Common IRB Common Trial Agreement NPC1 HPβCD Trial • HPβCD selected as a TRND clinical candidate in February 2011 • PreIND meetings with FDA in October and December 2011 • Juvenile dog toxicity study, formulation, and device compatibility studies performed in 2012 • IRB approval July 2012 and IND filing November 2012 • First ICV infusion February 4, 2013 • First IT infusion September 28. 2013 NPC1 TRND Team NICHD Nicole Yanjanin Aiyi Liu (DESPR) Roopa Shankar NHGRI Washington University School of Medicine Daniel Ory University of Pennsylvania Charles Vite Bill Pavan NINDS Russell Lonser John Heiss Albert Einstein Collage of Medicine Steven Walkley TRND/NCATS Johnson and Johnson Chris Austin John McKew Nuria Carrillo Liz Ottinger Juan Marugan Pramod Terse Xin Xu Wei Zheng Steven Silber Mark Kao Marcus Brewster SAIC/Leidos Jon Stocker Molly Buehn Leah Giambarresi RRD International Charles Finn Frank Hurley Joy Vanderwal Clinical Center Carmen Brewer Beth Solomon Naomi O’Grady Kelly King Patrick Frenchick Sandra Morseth Kimberly Lilly Acknowledgements SMD, PDEGEN, NICHD Nicole Yanjanin Lee Ann Knight Roopa Shankar Chris Wassif Celine Cluzeau Stephanie Cologna Ryan Lee Cynthia Toth Jiang Xiao-Sheng Ian Williams Antony Cougnoux Ara Parseghian Medical Research Foundation National Niemann Pick Disease Foundation ORD/CC SOAR-NPC Bench to Bedside Awards Dana’s Angels Research Trust Niemann-Pick disease, type C1 Niemann-Pick disease, type C1 Hydroxypropyl-β-Cyclodextrin Mouse Cat Mouse Cat Human Newborn 0.5 g 30.0 1400.0 375.0 Niemann-Pick Disease, type C1 Vertical supranuclear ophthalmoplegia Differential -Niemann-Pick Disease, type C1 -Progressive Supranuclear Palsy -Midbrain lesions Niemann-Pick disease, type C1 Attenuation of the 24OHC response with repetitive dosing