AD? - Alzheimer Europe
advertisement

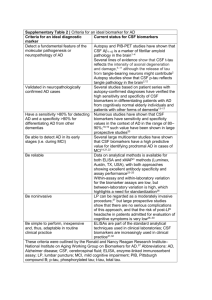
Changing the criteria for Alzheimer’s disease Alzheimer Europe - Vienna, October 2012 Pr Bruno Dubois Head of the Dementia Research Center (IMMA) Director of INSERM Research Unit (ICM) Salpêtrière Hospital – Paris 6 University DISCLOSURE 1) Reimbursed travels for speaking engagements, congress participation or educational activities: Eisai, Janssen-Cilag, Novartis 2) Consultancy: Affiris, BMS, Eli Lilly, Pfizer, Roche 3) Funding for my Institution: Novartis, Roche 1984 The NINCDS-ADRDA criteria The rules 1) The diagnosis of AD is clinico-pathological: it cannot be certified clinically and needs a post-mortem confirmation to be ascertained 2) The diagnosis of AD can only be ‘probable’ 3) The diagnosis of AD can only be made when the disease is advanced and reaches the threshold of dementia MCI CLINICAL [ POSTMORTEM dementia probable/possible AD neuropathology The current NINCDS-ADRDA diagnostic criteria have several limitations A low accuracy (60 to 80%) because they do not take into account the specific features of the disease Late in the course of the disease only when the dementia threshold is reached ! Two requirements: 1) to be earlier 2) to be more specific To be earlier: potential benefits • Obtain appropriate treatment earlier • Stop searching for other causes • Help the family to understand and accept • Financial and legal plans while competent • Enable the patient and family to make lifestyle choices • Induce better adherence and management of other medical conditions • Take appropriate steps to prevent injury (driving, weapons) • Get greater access to help within the healthcare system • Participate in clinical trials with disease modifier treatments from Cummings, 2011 To be earlier What is Alzheimer’s disease? Preclinical states Current point of diagnosis First symptoms 3–5 yrs Biomarkers AD? Specific memory disorders AD? Dementia AD? Subcortical dementia MCI Drugs Sleep disorders Depression AD FTD Normal aging Confusion Vascular disorders Low free recall AD is a progressive amnestic disease In more than 85% of the cases, AD starts as a progressive amnesic disease in relation with an early involvement of the hippocampus The Different Stages of LT Memory Dubois and Albert, Lancet Neurology, 2004 Stimulus Stimulus Registration Storage Retrieval Attention (depression) Temporal lobe (AD) Frontal lobe (aging) 1 Control of encoding with cueing 2 Facilitate the retrieval with cueing FCSRT (cued recall measures) is the best predictor of AD pathology CSF (+) n = 74 CSF (–) n = 111 effect size (d) FCSRT Total Recall 13.4 15.4 0.97 Logical Memory Delayed Recall 8.12 13.59 0.74 CERAD verbal Delayed recall 4.22 5.63 0.71 memory measures AD: can the exam predict the pathology? Wagner M et al, Neurology 2012 PET imaging A specific pattern in Molecular Neuroimagery (Klunk et al., 2004) • PET-PiB. Increased radioligand retention in AD compared to control subjects (Klunk, 2004) • PET-FDG. Pooled sensitivities and specificities (9 studies) of 86% for temporo-parietal hypometabolism (Patwardhan, 2004) specific pattern of CSF changes (low A beta; high tau and P-tau levels) even at an eary stage No progression to AD 1.0 0.8 0.6 0.4 Normal CSF Pathological CSF 0.2 (low A beta, high tau/p-tau) 0 0 10 20 30 40 50 Time (months) 60 Normal CSF 67 66 62 56 47 40 28 Pathological CSF 67 65 49 31 27 15 3 (Hansson et al. LN, 2006) Being more specific even at the prodromal stage of AD memory NINCDS ADRDA CSF not specified exclusion MRI PET-FDG PETligand exclusion not specified not known P–T hypo metabolism PiB retention IWG criteria amnestic ε H type Abeta T- P tau MTL atrophy Specificity for Prodromal AD >90% >90% >85% >80% >95% Sarazin 2007 Hanson 2006 Colliot 2008 Mosconi 2004 Rowe 2007 Sarazin et al. Neurology. 2007;69:1859-2016. Hansson et al. Lancet Neurol. 2006;5:228–234. Colliot et al. Psychiatr Sci Hum Neurosci. 2008;6:68-75. Mosconi et al. Neurology. 2004;63:2332-2340. Rowe et al. Alzheimers Dement. 2007;3. Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS-ADRDA criteria Dubois et al., Lancet Neurol., 2007 1 major clinical criterion Amnestic syndrome of the ‘hippocampal type’ (that can be isolated or associated to other cognitive / behavioral changes) + 1 or more biomarker present Structural: atrophy of medial temporal lobe (MRI) Biological: changes in biomarkers (CSF) Metabolic neuroimaging: regional hypometabolism on PET Molecular neuroimaging: amyloid ligand retention on PET New Diagnostic approach Before 2007 1) dementia: loss of autonomy 2) elimination of other causes of dementia: blood exams : endocrinopathies, infectious or inflammatory disorders… CT-Scan/MRI : vascular lesions, tumor, hydrocephalus… Diagnosis based on an exclusionary process Since 2007 1) an amnestic syndrome of the hippocampal type 2) integration of biomarkers in the diagnostic process: a biological signature on CSF the visualisation of brain lesions with PET amyloid tracer Diagnosis based on positive arguments The conceptual shift alzheimer’s disease 1984 NINCDS-ADRDA clinical pathological entity CLINICAL [ MCI POST-MORTEM dementia probable/possible neuropathology alzheimer’s disease 2007 IWG clinical biological entity CLINICAL typical / atypical BIOLOGICAL Biomarkers [ Applicability of the New Criteria: When? 1) In research settings: A high diagnostic accuracy is needed for: • study of specific outcomes: requires well phenotyped cohorts • academic research projects: not on heterogeneous population with a low/intermediate likelihood of diagnostic accuracy • inclusion in clinical trials : most of ongoing trials are based on the New Criteria: BMS (γ secretase inhibitor); Affiris (immunotherapy): Roche (immunotherapy); Lilly (BACE inhibitor); Nutricia (Medical food-Souvenaid); Sanofi (immunotherapy) … 2) In specific clinical conditions: BMs increase diagnostic accuracy that may be required in case of: • young onset AD • complex cases: PCA, PPA… The new lexicon 1) AD: starts with the first specific symptoms and encompasses both the prodromal and dementia phases 2) AD dementia: phase of AD with an impact on ADL 3) Prodromal AD: the early symptomatic, predementia phase of AD 4) Typical AD: common clinical phenotype of AD, characterized by an early amnestic syndrome of the hippocampal type 5) Atypical AD: less common but well characterized clinical phenotypes logopenic aphasia, posterior cortical atrophy, frontal variant of AD The diagnosis of AD needs in vivo evidence of pathophysiological markers 6) Mixed AD: patients who fulfill the criteria for AD with clinical and biomarkers evidence of other co-morbid disorders 7) Asymptomatic at risk: cognitively normal individuals with in vivo pathophysiological biomarkers of AD 8) Presymptomatic AD: cognitively normal individuals with a proven autosomal dominant mutation 9) Alzheimer’s pathology: neurobiological changes responsible for AD 10) MCI: patients for whom there is no disease clearly identified (Dubois et al, Lancet Neurology 2010)