Maximizing Failure Mode & Effects Analysis
advertisement

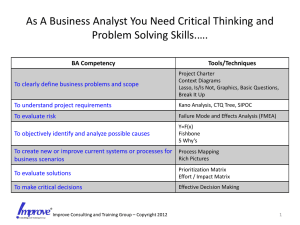
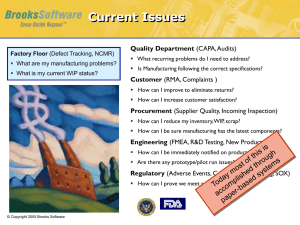
MAXIMIZING FAILURE MODE & EFFECTS ANALYSIS AS AN EFFECTIVE RISK MANAGEMENT TOOL Sandra Thompson Administrator, Quality Resources/Compliance Laurens County Health Care System Clinton, SC Thursday, May 31, 2012 TODAY’S GOALS Discuss establishing a “Culture of Safety” Describe the linkage between and importance of FMEA to RM Identify the TJC FMEA requirements Discuss the basics of failure mode and effects analysis Identify tools and resources for further information & study A GROWING CONCERN FOR PATIENT SAFETY…. 1995: “The year that medicine went to Hell in a handbasket” - Dennis O’Leary, JCAHO President, 9/01 Tampa: Wrong site surgery Dana Farber: Chemo event Martin Memorial: Anesthesia event These events helped drive a consensus for change “CULTURE OF SAFETY” Imperative driven by IOM reports “To Err is Human” – 1999 “Crossing the Quality Chasm” – 2000 Culture of Safety is owned by ALL Not physicians, Administration, or a single department Requires new tools, new thinking, new information not traditionally utilized in healthcare FMEA, RCA, Six Sigma, Lean, Systems Engineering, ???? NEW TOOLS/NEW THINKING Root cause analysis Lean Forcing functions (poke yoke) Standardization (5S) Customer focus (value stream mapping) Front-line staff involvement (observation – “going to the gemba”, spaghetti diagrams) Push/pull systems (patient flow) High-reliability organizations “Going for Zero” Electronic health record Proactive risk assessment Healthcare FMEA! TOOLS OF CHANGE Proactive Proactive Risk Assessment (FMEA, HFMEA) Automation, Computerization Standardization Protocols, PrePrinted Orders Checklists Least Effective Effectiveness Scale Forcing Functions Most Effective Rules & DoubleChecking Information Inspection Education Reactive Auditing HFMEA is a proactive means of assessing & decreasing risk in your organization! FMEA VS. HFMEA FMEA Failure Mode & Effect Analysis Traditionally used in industry Looks at a device or a component HFMEA Healthcare Failure Mode & Effect Analysis Looks at a process HFMEA Process developed by VA Pt. Safety Center Online tutorial at: http://www.patientsafety.gov/CogAids/HFMEA/ind ex.html#page=page-1 FAILURE MODE & EFFECT ANALYSIS Do you take actions to prevent yourself from being late to work? Yes or No Do you “take the shortcut” when you see traffic building up in a familiar place? Yes or No Do you try to distinguish “big problems” from “little problems”? Yes or No Do you see the possibility of eliminating some problems, but need a better way to show that to people? Yes or No FAILURE/FAILURE MODE Failure When process begins to produce undesired results/effects Failure Mode Weakness/vulnerability in any part of process Chain of events that has potential to cause safety problem RISK MANAGEMENT PERSPECTIVE Assists RMs to favorably impact the patient care environment Another tool in the box of RM strategies to understand and reduce medical error Assists RMs & others in driving change before it can do harm Proactively forecasts potential failures Applies risk /loss control techniques to those potential failures WHERE TO START: FOUNDATION What philosophy ? “Blame free” vs. “Just Culture” Do we see systems or individuals? Are the right tools & resources available for the job? What is an incident to be reported at your facility? Close call/near miss/”good catches”? Only adverse events (e.g., “harm”)? Sentinel events? Where do willfully unsafe acts fit in? Disruptive behavior? WHERE TO START: FOUNDATION Design/redesign incident reporting systems to capture near misses Predictive – show patterns around a process – 100:10:1 Rich source of information Reward/encourage near miss reporting Follow up on near misses and trend Don’t forget the narrative! Important details found here Close the loop – report back to staff on trends, patterns noted, solicit suggestions for improvement WHERE TO START: FOUNDATION Must filter the tidal wave! WHERE TO START: FOUNDATION For each reported incident: Assign Severity Catastrophic Failure could cause death or serious injury (Sentinel Events) Major Permanent lessening of bodily functioning, disfigurement, surgical intervention required, additional treatment required (3 or more patients) Moderate Increased LOS, increased level of care (1-2 patients) Minor No injury, no increased LOS, no increased level of care WHERE TO START: FOUNDATION Assign Frequency: Frequent: Likely to occur immediately or within a short period (may happen several times in one year) Occasional: Probably will occur (may happen several times in 1-2 years) Uncommon: Possible to occur (may happen sometime in 2-5 years) Remote: Unlikely to occur (may happen sometime in 5-30 years) CULTURE OF SAFETY: FOUNDATION Apply the risk management equation Severity x Frequency = RISK What resources per level of risk? Examine trends/patterns Severity Probability Catastrophic Major Moderate Minor Frequent 3 3 2 1 Occasional 3 2 1 1 Uncommon 3 2 1 1 Remote 3 2 1 1 GETTING STARTED: SELECT A HIGH-RISK PROCESS Sources: Your incident report data Loss runs/claims data Brainstorm list of HR processes for your organization Consider physical resources, environment, staffing, etc. Worker’s Compensation reports Literature Sentinel Event Alerts Infection Control data IHI Joint Commission Organizational strategic quality goals/objectives ASSEMBLE A TEAM Multidisciplinary group who have hands-on experience with the selected process/procedure Include physicians! RM role May be multifaceted CAUTION: Leader/Facilitator DIAGRAM THE PROCESS ABSOLUTE MUST: Tools: Direct observation of process (Lean) “Process Mapping” vs. Flowcharting Fishbone (Cause & Effect Diagram) Current State Stream Maps (Lean) Differentiate - need TWO maps! “The way things were intended to work” “The way things are actually working” PROCESS MAPPING Process Step Process Step Process Step 1 2 3 Medication ordered Auto electronic transfer to Pharmacy system Pharmacy fills scipt; sends to floor Process Step 4 Nurse administers Sub-Processes Sub-Processes A. B. A. B. Dummy terminal PCs Dummy terminal PCs Sub-Processes A. B. C. D. E. Check drug allergies Check drug interactions Check proper dosages Orders labs Order sent to auto dispensing Sub-Processes A. B. C. D. Automatically fills orders checked Drugs pulled and script filled Med cart filled Cart sent to floor Sub-Processes A. B. C. D. E. F. Log on to laptop Medcart Medications scanned Patient band scanned Medication given to pt. Pt. record updated IDENTIFY POTENTIAL FAILURE MODES Compare “ideal” vs. “reality” May be multiple failure modes – list all Each failure mode can have multiple possible effects Tool: Brainstorming Ask: What could fail with this step? (i.e., failure modes) Why would this failure occur? (i.d., causes) What could happen if this failure occurred? (i.e., effects) ASSESS FAILURE MODES-IDENTIFY CAUSES Assess risk – severity/probability Tools: Fishbone (C&E) Diagram Hazard Scoring Matrix (HFMEA) Probability Severity Catastrophic Major Moderate Minor Frequent 16 12 8 4 Occasional 12 9 6 3 Uncommon 8 6 4 2 Remote 4 3 2 1 ADDITIONAL STEPS Decision (proceed or stop) If score 8 or higher & decision to stop, document rationale Tools: Decision Tree (HFMEA) HFMEA Worksheet Develop action plan for change Include outcome measures, management concurrence PROTECTING THE PROCESS Concerns re: discoverability Could provide potent evidence for plaintiff if all potential failures not addressed & mishap occurs involving that failure point Follow current procedures under state law relative to peer review protection Must be produced under guidance of medical staff & reviewed in “medical staff committee” Include “disclaimer” on document Seek guidance from legal counsel REMEMBER….. Seek support from senior leadership Include physicians Executive/Administrative Sponsor? Physician Champion Seek out trained facilitator OR get training in facilitation Important to open communication Involve front-line staff; give them ownership Look for best practices already identified for the process being assessed QUESTIONS? RESOURCES VA Center for Patient Safety HFMEA Toolkit http://www.patientsafety.gov/CogAids/HFMEA/index.ht ml#page=page-1 Institute for Healthcare Improvement Online tool for conducting FMEA; can be shared Tutorials, journal articles Completed examples http://www.ihi.org/knowledge/Pages/Tools/FailureMod esandEffectsAnalysisTool.aspx OTHER RESOURCES http://www.patientsafety.gov/SafetyTopics/HFMEA /FMEA2.pdf http://psnet.ahrq.gov/resource.aspx?resourceID= 1531 http://www.patientsafety.gov/SafetyTopics/HFMEA /HFMEAIntro.pdf http://intranet.uchicago.edu/quality/FailureMode sandEffectsAnalysis_FMEA_1.pdf http://www.patientsafety.gov/SafetyTopics/HFMEA /HFMEA_JQI.pdf