Diabetes - Loma Linda University Medical Center
advertisement

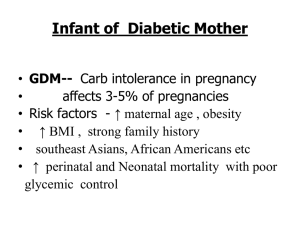
Infant of the Diabetic Mother Sunhwa Kim, MD Loma Linda University Children Hospital Diabetes … Obesity Not every high blood sugar is Diabetes Obesity Diabetes Obesity…Diabetes Metabolic abnormalities associated with obesity – Hyperglycemia, dyslipidemia, alterations in growth factors, hyperinsulinism etc. Excessive abdominal fat independently associated with diseases: cardiovascular, cancer, osteoarthritis, gall bladder, diabetes, etc Excess body fat leads to type 2 diabetes within 20 years Undiagnosed diabetes Obesity… Pregnancy Complications Adjusted* Odds Ratios for Pregnancy Complications by Maternal BMI Adjusted Odds Ratio 5 4 Normal (BMI 20.0-24.9) 3 Overweight (BMI 25.0-29.9) 2 Obese (BMI >= 30.0) 1 0 Gestational diabetes Preeclampsia Eclampsia *Adjusted for maternal age, smoking, education, marital status, trimester prenatal care began, payer, and weight gain during pregnancy; BMI<20.0 (lean) reference group. Baeten et al., Am J Public Health 91;436, 2001 Maternal Complications of Diabetes Unstable maternal BG Cardiovascular conditions Sepsis Birth Difficulties PP recovery issues Psychosocial issues Delivering an affected infant Infant of the Diabetic Mother First described: 1880 Insulin isolated in 1921 maternal mortality decreased from 50 to 9 % Stillbirhts decreased from >20% to 2% in the 1980’s Perinatal mortality decreased after 1970NICU is still higher than controls (17 vs. 6/1000 in Europe 22 vs. 10/1000 in CA) Congenital malformations remain high IDM - Definitions Any offspring of a gestational or insulin dependent diabetic woman – Type 1-insulin dependent – Type 2 – Gestation Diabetes Mellitus – Impaired Glucose Tolerance Diabetes complicating Pregnancy 0.5-1.0% of all pregnancies are complicated by pre-existing diabetes 0.1 % are insulin dependent diabetes 1-5% gestational diabetes IDM -Incidence 50-150,000 Perinatal 5% IDMs born annually mortality: 20/1000 total births of all NICU admissions IDM - Outcome Outcome is largely dependent on consistent blood glucose control from the preconception period through embryonic and fetal life. Lack of control in early or late pregnancy leads to different problems in the offspring IDM -Early Pregnancy Diabetic Embryopathy Poor early control (Hyperglycemic embryo) Risk for Congenital Malformations Glucose Control and Malformations MALFORMATION RATES BY LEVEL Of MATERNAL HEMOGLOBIN A1c 6.9 or less 7.0-8.5 8.6 or greater 0% 5.1 % 22.4 % Miller et al. N Engl J Med 304:1331-1333, 1988 Glucose Control and Malformations HbA1c* % Malformations <6 6.1-9.0 9.1-12.0 12.1-15.0 >15.0 3.0% 5.2% 4.3% 38.9% 40.0% RR (95% CI) 1.0 1.7 (0.4-1.7) 1.4 (0.3-8.3) 12.8 (4.7-35.0) 13.2 (4.3-40.4) *1st trimester HbA1c in 303 insulin-requiring diabetics (Green et al. Teratology 39:224-231, 1989) Embryopathy Gestational Diabetic Women’s Risk Becerra JE et al., 1990 – Relative risk for major malformations among IDM was 7.9 compared to infants of non-diabetic mothers – Gestational diabetics who require insulin in 3rd trimester were 20.6 times more likely to have a child with a cardiovascular defect Kouseff BG, 1999 – 152 infants of women with gestational DM, 87 had anomalies compatible with diabetic embryopathy Embryopathy Gestational Diabetic Women’s Risk Schaefer-Graf et al., Am J Obstet Gynecol 182:313-320, 2000 – 4,180 consecutive pregnancies complicated by gestational diabetes (3,764) or type 2 diabetes (416) diagnosed after 20 weeks gestation (County USC). » Initial fasting glucose < 120 mg/dL 2.1% malfs » Initial fasting glucose 121-200 mg/dL 5.9% malfs » Initial fasting glucose > 200 mg/dL 12.9% malfs Watkins et al., Pediatrics 111:1152-1158, 2003 – Prepregnancy obesity (with no known diabetes) associated with increased risks for spina bifida, omphalocele, heart defects, and multiple anomalies. Diabetic Embryopathy -Incidence 2 to 4-fold Increased Risk for Malformations (48%) 7 to 10-fold Increased Risk for Major Anomalies that are fatal or require surgery Central nervous system Cardiac malformations Renal / urinary and GI tract anomalies Skeletal anomalies Diabetic Embryopathy -CNS anomalies Central nervous system Neural tube defects – Anencephaly – Meningomyelocele Hydrocephaly Holoprosencephaly Diabetic Embryopathy Midline facial defects Facial microsomia and microtia/anotia: Diabetes in 10.3% of 155 case mothers versus 1.4% of 854 control mothers Multivariate-adjusted odds ratios (CI): Diabetes 6.3 (2.7 -1 4.9) (Werler et al., Birth Defects Research 70:258, 2004) Diabetic Embryopathy – Cardiac anomalies Transposition of great vessels Coarctation of the aorta Atrial & Ventricular septal defects Dextrocardia Single ventricle, hypoplastic right heart Patent ductus arteriosus Pulmonary hypoplasia / atresia DiGeorge sequence Diabetic Embryopathy, GI anomalies GI: Small Left Colon Syndrome Bowel atresia Bowel dysmotility (feeding intolerance) Diabetic Embryopathy – Skeletal Anomalies Caudal Dysplasia or Regression SD – Rare disorder (1/25000) – The most specific malformation related to diabetes 200-400 times more often in IDMs – Sacral agenesis with hypoplastic pelvis and spinopelvic instability – Usually with other malformations like: femoral hypoplasia, extrophy of the bladder, and club foot Diabetic Embryopathy Pathophysiology Hyperglycemia + Genetic background Teratogenic period (3-6 weeks) Disturbances in maternal-fetal circulatory transport systems Concentrations of metabolites – – – – Hyperglycemia Hyperketonemia Elevated intracellular levels of free oxygen radicals Disturbances in arachadonic acid and prostaglandin/prostacyclin metabolism affecting intracellular signaling and circulation – Somatomedin inhibitors – Genotoxicity as a result of aberrant fuels (Reece et al., Teratology 54:171-182, 1997) Diabetic Embryopathy PREVENTION BEFORE CONCEPTION Good Glycemic control Folic Acid/ Vitamin intake IDM - Late Pregnancy Fetal and Neonatal Complications Poor late control (Hyperglycemic fetus) Risk for Hyperinsulinemia (growth factor) IDM -Late Pregnancy Fetal and Neonatal Complications of Hyperinsulinemia – Macrosomia growth of insulin-sensitive tissues plus glycogen and fat deposition – – – – – Hypoglycemia Polycythemia/hyperbilirubinemia Renal vein thrombosis Cardiomyopathy RDS Fetal & Neonatal Complications Macrosomia LGA – Birth weight > 4 kg or above the 90th percentile for gestational age Occurs in 20-60% IDM Physical findings – Increased adipose tissue – Disproportionate head/shoulder ratio – Plethoric – Large placenta & cord IDM may also be SGA in advanced diabetes complicated with renal and cardiac disease Fetal & Neonatal Complications Macrosomia Complications associated with delivery Birth trauma – – – – Shoulder dystocia Brachial plexus injury Fractured clavicle Visceral hemorrhage CPD – Risks associated with C/Section and operative vaginal deliveries (vacuum extraction, forceps, etc.) – Fetal distress – Meconium aspiration – Birth Asphyxia Hypoglycemia Symptoms Jitteriness 81% Seizures 58% Apnea/cyanosis 47% Irritability 41 % Hypotonia 26% Poor feeding Hypothermia None Defintition: Blood glucose <40 mg/dL Usually presents at ½-2 hours of life Incidence: up to 40% of IDM Hypoglycemia Treatment If stable give early feedings If not able to feed: D10%W 2mL/kg (slow IVP) plus Continuous IV infusion of D10%W at 80-100 mL/kg/day Use Follow glucagon in extreme cases blood glucose with frequent Chemstrips Hyperbilirubinemia Definitions: Elevated indirect (unconjugated) bilirubin >10mg/dL in term infant, lower levels for preterms Incidence in IDM 20-40% Pathophysiology – Increased bilirubin production » Polycythemia » Heme turnover (ineffective erythropoeitin. and trauma) – Decrease in bilirubin binding and excretion » Liver immaturity Hyperbilirubinemia Prevention – Early, adequate breastfeeding – Good hydration and stooling Diagnosis – Transcutaneous or serum bilirubin at 24 hours of age, and at signs of increasing jaundice Treatment: – Adequate hydration and nutrition – Phototherapy – Exchange transfusion – Medications (agar) – Family teaching – Appropriate follow-up after discharge Polycythemia Due to bone marrow stimulation (high erythropoietin levels) Elevated venous hematocrit of > 65% Caused by chronic hypoxia and increased O2 requirements in utero Placental insufficiency during fetal life May be worsened by placental transfusion at birth Incidence in IDM 35% Signs and symptoms – Plethora – Jitteriness – Tachypnea – Cyanosis (general or circumoral) – Oliguria – Poor feeding – Lethargy/seizures Screening: obtain hematocrit at 24 hrs of life or if symptoms noted Polycythemia Treatment – Treat underlying symptoms – Hydration – Hyperbilirubinemia treatment – Partial exchange transfusion Common complications – – – – – Respiratory Distress Hyperbilirubinemia Respiratory distress Renal vein thrombosis Hypertension IDM -Cardiomyopathy Cardiomegaly present in 30% Septal hypertrophy Myocardial dysfunction – Glycogen stores – Hypoxia CHF in 5% – Treatment: supportive therapy and beta blockers Other Fetal & Neonatal Complications Perinatal hypoxia/asphyxia Respiratory Distress Metabolic abnormalities: – Hypocalcemia – Hypomagnesemia Small left colon Syn. Neurologic dysfunction Perinatal Hypoxia May lead to fetal demise or neonatal asphyxia May result from complicated labor and delivery – – – – – – – Placental insufficiency (vascular disease, pre eclampsia) Maternal ketoacidosis CPD/ Prolonged labor due to Macrosomia Meconium Aspiration Intra-abdominal hematoma/hemorrhage Polycythemia Increased oxygen utilization from hyperinsulinism and increased metabolism Respiratory Distress Transient Tachypnea of Newborn (delayed lung fluid clearance) Aspiration of meconium or amniotic fluid Prematurity Diagnosis Tachypnea/Retractions Grunting Cyanosis Apnea Hypoxemia Chest X-Ray Respiratory Distress Syndrome RDS (delayed lung maturity), higher risk than non IDMs. Respiratory Distress Syndrome surfactant from decreased steroids due to insulin Prevention: Check for lung maturity with presence of PG and L:S ratio >2 Treatment: – Surfactant – Assisted support and ventilation – Supplemental oxygen Hypocalcemia/Hypomagnesemia Incidence: 25% Secondary to hypoparathyroid function due to maternal-fetal hypomagnesemia Related to severity of maternal diabetes Develops in first 3 days Hypocalcemia/Hypomagnesemia Symptoms: – Irritability – Jitteriness – Apnea – Lip smacking – Tongue thrusting Laboratory Tests – Calcium – Ionized CA – Magnesium Treatment – Transfer to Neonatal Intensive Care Unit – Calcium gluconate – Magnesium sulfate IDM - Neurologic Dysfunction Due Jitteriness Irritability Increased or Decreased tone Seizures to: – Chronic and/or acute hypoxia – Immaturity – Hypoglycemia – Hypocalcemia – Polycythemia/strokes – Delivery trauma – Iron deficiency Oral Feedings Significant feeding difficulties Severe uncoordination Assess oral-motor coordination Assess adequacy of feeding Monitor pre feeding blood glucose IDM and Breastfeeding Offer breast as soon as possible within 1 hour of delivery Encourage feedings whenever oral cues noted or at least every 3 hours Formulas: only when medically indicated or mother has given informed consent Keep mother and infant together continuously Support mothers to nurse often (10-12 times per day) IDM- Long Term Prognosis Metabolic Syndrome (identifiable early precursor to adult chronic diseases including diabetes, heart disease, certain cancers, and others) • Obesity • Glucose Intolerance • Dyslipidemia • Hypertension Predisposing factors . Infant of a diabetic mother . Infant of an obese mother . Large for gestational age infant Long Term Prognosis Growth / Development Childhood obesity (50%, 5 fold higher at adolescence) Risk of Developing Insulin Dependent DM . Diabetic mother 2% . Diabetic father 7% Risk for delayed motor and cognitive development Neurological development indefinite IDM Neurodevelopmental Outcome The IDM needs to be supported since conception If we are to help the mothers to achieve