Document
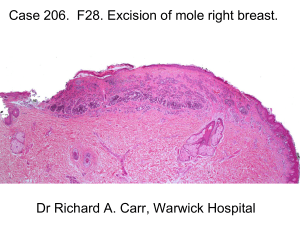
advertisement
Lumps, Bumps & Pigmented Things By Iain Macleod Assessment of a lump Site Size Shape Surface Colour Consistency Edge Solitary or Multiple Differential diagnosis of a lump Hyperplasia vs Neoplasia Neoplastic Benign vs Malignant Wide differential diagnosis Common clinically benign lumps Fibroepithelial polyp Pyogenic granuloma Epulides Denture granuloma Squamous cell papilloma Mucoceles FORDYCE DISEASE (Fordyce Granules) • Yellowish Plaques or Papules • Usually Multiple and Bilateral • Usually Buccal Mucosa (but may be found anywhere) • Ectopic Sebaceous Glands • Common (~80%) • No treatment required clinical diagnosis FOLIATE PAPILLAE (Lingual Tonsil??) • Normal Anatomic Structures • Posterior Lateral Tongue • Tissue Swelling with Vertical Grooves Containing Taste Buds and von Ebner Salivary Glands • Often Include Hyperplastic Lymphoid Aggregate • No Treatment Required - May require biopsy for diagnosis LYMPHOID AGGREGATES • Small “ReddishYellow” Nodules / Papules • Soft Palate or Base of Tongue (Lingual Tonsils) – Part of Waldeyer’s Ring • “Ectopic” Lymphoid Tissue • No treatment required - may require biopsy for diagnosis VASCULAR ANOMALIES Vascular anomalies • • • • Hamartomas – Benign neoplasms Haemangioma Lymphangioma Sturge – Weber syndrome (encephalofacial angiomatosis) • Malignant variants – eg. Kaposi’s sarcoma • Varicosities / venous lakes VARICOSITIES • Reddish-Blue to Purple Nodules (Usually < 5 mm.) - Dilated Veins • Lip, Buccal Mucosa, Ventral/Lateral Tongue, Floor of Mouth • Age Associated (more common in older patients) • Will Blanch on pressure • No treatment required May require biopsy for diagnosis CONNECTIVE TISSUE HYPERPLASIAS Connective tissue hyperplasias • • • • • • • Epulides (epulis) Denture irritation hyperplasia Papillary hyperplasia of palate Fibroepithelial polyp Fibrous tuberosities Chronic hyperplastic gingivitis Drug induced gingival hyperplasias Epulides • Fibrous • Vascular – pyogenic granuloma , pregnancy epulis • Giant cell – peripheral , central , hyperparathyroidism (raised PTH , calcium) • Congenital Giant cell granuloma • • • • • Peripheral Central Radiographs Hyperparathyroidism Check blood chemistry – calcium & PTH levels Gingival fibrous hyperplasia • Familial • Drug induced – eg.phenytoin, cyclosporin , nifedepine • Pubertal Salivary Gland Swellings Salivary Disorders • • • • • Developmental Obstructive Infectious Autoimmune Neoplastic Obstructive Salivary Diseases • Mucous Extravasation (Mucocele) • Ranula • Sialolithiasis • Ductal Compression (Tumours) Mucous Retention (Extravasation) • Lower lip>Buccal mucosa>Ventral tongue • Trauma, ductal laceration • Mucous escape into connective tissue • Walling-off effect • Excision, extirpation of feeder glands Sialolithiasis • • • • • SMG>Parotid>Minor Glands Pain at mealtimes Glandular tender swelling Negative secretion upon milking Occlusal and other radiographs Sialadenitis • Endemic Parotitis (Mumps) • Sclerosing, secondary to duct blockage • Bacterial Sialadenitis • Autoimmune Sialadenitis Sialosis (sialadenosiss) • Idiopathic enlargement of salivary glands – most often parotids – Metabolic factors • • • • Alcohol Drugs Diabetes Anorexia & bulimia Necrotizing Sialometaplasia • • • • • • Ulcerative Lesion Non-elevated margins with necrotic centre Palate most common site Often Painless Necrosis of acini Ducts undergo squamous metaplasia Salivary Gland Neoplasia Classification – WHO (modified) • Adenomas – – – – – – Pleomorphic adenoma Warthin tumour (adenolymphoma) Basal cell adenoma Oncocytoma Canalicular adenoma Ductal papillomas • Carcinomas – – – – – – Mucoepidermoid carcinoma Acinic cell carcinoma Adenoid cystic carcinoma Carcinoma arising in pleomorphic adenoma Polymorphous low grade adenocarcinoma Other carcinomas Salivary Neoplasms • Rule of nines: 9/10 are benign; 9/10 occur in parotid; 9/10 are pleomorphic adenomas • Look for rate of growth • Parotid – facial nerve involvement – highly suggestive of malignancy • Most painless but adenoid cystic carcinoma spreads perineurally – painful! Rule of thumb!-----• Swellings in lower lip – mucoceles; swellings in upper lip neoplasms Facial Palsy • Upper motor neurone - Spares forehead • Lower motor neurone – complete palsy Bone lumps TORI (plural) / TORUS (singular) Palatal or Mandibular • Bony Growths – Mid-Hard Palate (20%) – Lingual Mandible (10%) – May show up as X-Ray Radiopacity – Anywhere else called “Exostoses” – subject to trauma and ulceration • No Treatment Required (unless necessary for Denture construction) Pigmentation Definitions • Endogenous: the source of pigment is from inside the body – Haemoglobin red / blue – Haemosiderin brown – Melanin brown • Overproduction • Overpopulation • Exogenous: the source of the pigment is from outside the body – Traumatic deposition (amalgam / graphite tattoo) – Ingested heavy metals – Colonization of bacteria (hairy tongue) Classification of pigmented lesions: 1. Blue/purple vascular lesions 2. Brown melanotic lesions 3. Brown Haem-associated lesions 4. Grey/black pigmentations I- Blue/purple vascular lesions • Haemangioma • Varix • Angiosarcoma • Kaposi’s sarcoma • Hereditary Haemorrhagic Talangiectasia (HHT) Hereditary Haemorrhagic Talangiectasia (HHT) • Microaneurysms caused by weakening defect in the adventitial coat of venules • Genetic disease (autosomal dominant) • Multiple round/oval purple papules <0.5 cm • >100 lesions oral and nasal mucosa • Facial skin and neck may also be affected • Diagnosis: – – – – • Family history Epistaxis which might be severe Platelet studies are normal More purple and nodular not macular like petechiae No treatment Brown melanotic lesions 1. Physiologic pigmentations 2. Smoker’s melanosis 3. Ephilis and oral melanotic macule 4. Naevocellular nevus and blue nevus 5. Malignant melanoma 6. Drug-induced melanosis 7. Café-au lait pigmentation 8. Pigmented lichen planus 9. Endocrinopathic pigmentation 10. HIV oral melanosis 11. Peutz-jeghers syndrome Ephelis and oral melanotic macule • Ephelis in skin and intra-oral melanotic macule in mucosa • oval / irregular in outline, brown or black • Don’t enlarge if they reach a certain size • Overproduction of melanin confined to the basal cell layer or the immediately adjacent keratinocytes • Have no malignant transformation risk • Surgical excision and review Naevus • Naevi results from benign proliferations of melanocytes • When a meloncyte mature it becomes a naevus cell • Two types: – Naevocellular naevi – Blue naevi • common on the skin but rare in the oral mucosa Naevocellular naevus JUNCTIONAL NAEVUS • Focal proliferation of melanocytes in the basal layer clinically appear as round or oval melanotic macule COMPOUND NAEVUS • contains groups of naevus cells in the connective tissue • Some cells remain in contact with the basal keratinocytes clinically appear as dome shaped nevus INTRAMUCOSAL / INTRADERMAL NAEVUS: located entirely within the lamina propria. Clinically in skin appear as nodule with few hairs often protruding Blue naevus • Form ~ 1/3 of all oral naevi • Located deeper than intramucosal naevi blue color • Characterized by a proliferation of spindle-shaped pigmented melanocytes and melanophages loosely grouped together Moles! Look for: Asymmetry, Irregular border, Colour, Change in size Bleeding or Itchiness Malignant melanoma • Rare • Arises from neoplastic transformation of either melanocytes or naevus cells • Aetiology of oral melanoma is unknown • Peak incidence 40-60 years • Lesions typically dark brown/bluish black/ mixture of colours or rarely non-pigmented (red) • Starts as asymptomatic macule of irregular margins (months/years) then become slightly raised or nodular • Ulceration, pain, bleeding, loosening of teeth may present Malignant melanoma • Metastases are common with spread to regional lymph nodes, lungs, liver, brain and bones • 5 year survival rate is only 5% in patients who present with cervical lymph node metastases • Tumour thickness is the single most important prognostic feature • HISTOPATHOLOGY: malignant melanocytes invading both epithelium and connective tissue Drug-induced melanosis • Large multifocal melanotic macule (no nodularity/swellings) • Increase in melanin pigmentation NOT in number of melanocytes • Pigmentation remains some time after stopping medication • Examples: 1. Minocycline 2. Anti-malarials 3. Zidovudine (AZT) 4. Oral contraceptives 5. Cytotoxics 6. Anti-convulsants (phenothiazines) Pigmented lichen planus • Rarely erosive OLP can be associated with diffuse melanosis • This can be related to the T cell infiltration and basal cell layer degeneration • Histologically: the usual features of OLP are observed along with basilar melanosis and melanin incontinence. Endocrinopathic pigmentation ADDISONS DISEASE: • Cortisol ACTH & Melanin Stimulating Hormone (MSH) diffuse cutaneous pigmentation and multiple oral melanotic macules PITUITARY GLAND BASED CUSHING’S DISEASE: • adenoma in the pituitary gland ACTH & MSH HIV oral melanosis • Aetiology remains undetermined • Could not be related to adrenocortical involvement or medications • affect skin, nails and mucous membrane (Buccal mucosa most commonly affected) Peutz-jeghers syndrome • Autosomal dominant inheritance • Multiple peri-oral epelides less than 0.5 cm in diameter. • Similar lesions may occur on the tongue, buccal mucosa and labial mucosa • Intestinal polyposis: This is low possibility for malignant transformation Albrights Syndrome • Polyostotic fibrous dysplasia • precocious puberty • other endocrine abnormalities • Skin pigmentation frequently overlies affected bones • pigmentation of oral mucosa is rare Brown Haem-associated lesions • Ecchymosis • Petechia • Haemochromatosis Ecchymosis • Common on the face and lips but not intraorally • Immediately after the trauma it will appear as a red macule or a swelling, after few days it becomes brown (hemoglobin degraded to haemosiderin) • Ecchymosis can be seen in – Patients taking anticoagulant drugs – Chronic liver failure Petechia • Generalized if secondary to platelet deficiencies or aggregation disorder – Idiopathic thrombocytopenic purpura (ITP) – HIV- related ITP – Aspirin toxicity – Bone marrow suppression by chemotherapy • Localized to soft palate – Excessive suction to relieve pruritus caused by common cold or allergy Haemochromatosis • Iron overload leading to deposition of haemosiderin pigment in multiple organs • Primary heritable disease with a prominent male predilection • Can be secondary to chronic anaemia, cirrhosis, or excess intake of iron • Brown to grey diffuse macules that tend to occur on the palate and gingiva Grey/black pigmentations • • • • Amalgam tattoo Graphite tattoo Hairy tongue Pigmentation related to heavy-metal ingestion Pigmentation related to heavymetal ingestion • Now is rare • Heavy metals ingestion caused by: – Medication – Occupational (industry & paint) • Deposited in skin and oral mucosa • Typically linear distribution in gingivae • Can also get systemic toxicity (behavioural changes & neurological disorders)