Bronchietasis - Macomb
advertisement
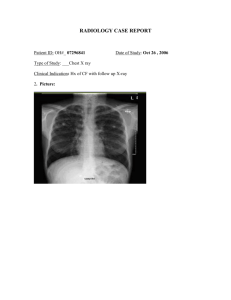
Bronchiectasis Chapter 14 – Des Jardins P. 584-589 – Merck Manual Objectives • • • • • State the clinical definition for Bronchieactasis Describe the anatomic alterations of the lungs in Bronchieactasis Describe the etiology of Bronchieactasis List the clinical manifestations seen in Bronchieactasis. Include findings of the physical examination, laboratory tests, pulmonary function tests, chest x-rays, arterial blood-gas values, and hemodynamic indices. Describe the management of Bronchieactasis. Definition • A chronic dilation and distortion of one or more bronchi due to extensive inflammation and destruction of the bronchial wall cartilage, blood vessels, elastic tissue and smooth muscle. Etiology • Usually occurs secondary to: • Repeated, severe pneumonia • • • • • • • Measles, Pertussis, Adenovirus in children Klebsiella Staphylococci Influenza virus Fungal infections Myocbacteria Mycoplasma • Bronchial Obstruction • Congenital Defect • Manifestation of Cystic Fibrosis • Kartagener’s Syndrome • Primary ciliary dyskinesia (PCD) Etiology (cont.) • Idiopathic • Accounts for roughly 50 to 80% of cases • Possible immunologic defect or autoimmune abnormality. • Immune-related diseases • Allergic bronchopulmonary aspergillosis (ABPA) • Collagen Vascular diseases • Rheumatoid arthritis • Sjögren syndrome • Ulcerative colitis • Crohn’s disease • Immune deficiencies (?) Pathophysiology • Either one or both lungs may be involved. • It is commonly limited to a lobe or segment and is frequently found in the lower lobes. • Right Middle Lobe and Left Lingula also possible. • Extent and character of pathologic changes determines the functional abnormalities. • Increased mucus production with impaired mucociliary clearance • Changes in lung volumes distal to obstruction • Increased due to Ball-Valve effect • Decreased due to atelectasis • Reduced flow rates • / defects with hypoxemia Types of Bronchiectasis Varicose Saccular Technically there are 2 other kinds: Follicular and Traction. But….who cares? Cylindrical Varicose Bronchiectasis • Bronchi are dilated and constricted in an irregular fashion similar to varicose veins. • Varicose bronchiectasis is also called fusiform. Cylindrical Bronchiectasis • Bronchi are dilated and have regular outlines similar to a tube. The dilated bronchi fail to taper for 6-10 generations and then in the bronchogram appear to end squarely because of mucous obstruction Saccular Bronchiectasis • Bronchi progressively increase in diameter until they end in large, cyst-like sacs in the lung parenchyma. • This form causes the greatest damage to the tracheobronchial tree. • The bronchial walls become composed of fibrous tissue. • Cartilage, elastic tissue and smooth muscle are all absent. Anatomic Alterations • Copious amounts of bronchial secretions. • Mucociliary clearance mechanism is impaired. • Foul smelling mucous from anaerobic organisms. • Mucous plugs cause partial or complete obstruction. • Hyperinflation of the distal alveoli as a result of an expiratory check valve obstruction. • Atelectasis, consolidation, and fibrosis results from complete bronchial obstruction. Pathophysiology • Obstructive Lung Diseases but can have a restrictive component if alveolar lung volumes are reduced. • Obstructive and Restrictive Disease Physical Examination • Vital Signs: • f: Increased (tachypnea). • HR: Increased • BP: Increased (Increased CO) • Inspection: • • • • • Pursed lip breathing. Cyanosis. Prolonged expiratory phase. Increased A-P diameter Digital clubbing Physical Examination • Palpation: • Use of accessory muscles during I & E. • Percussion: • Hyperresonant if obstructive, Dull if restrictive. • Auscultation: • Inspiratory crackles and/or rhonchi. • May be diminished if obstructive, bronchial with restrictive. Physical Assessment • Chief complaint: • Cough with large volume of sputum • Hemoptysis • Sputum settles into distinct layers with streaks of blood often seen • Thick, tenacious sputum • Chronic sinusitis is a common complaint. • Also nasal polyps • Kartagener’s Syndrome (Bronchiectasis, dextrocardia & paranasal sinusitis). • 20% of Bronchieactasis is as a result of Kartagener’s. ABG • Mild to Moderate Bronchiectasis • Acute alveolar hyperventilation with hypoxemia. • Severe Bronchiectasis • Chronic ventilatory failure with hypoxemia. • Oxygenation Indices • Increased shunting. • Decreased oxygen delivery. Pulmonary Function Studies • Obstructive Disease • Decreased FVC and FEV1.0 • Decreased Flowrates • Increased RV, FRC, TLC, RV/TLC • Restrictive Defect • Reduced RV, FRC, TLC • RV/TLC ratio normal • Flows are normal. Chest X-ray • Obstructive Lung Disease • • • • Translucent (dark) lung fields Depressed, flattened diaphragms Long, narrow hearts Right ventricular enlargement • Restrictive Process • Atelectasis and consolidation • Increased opacity Laboratory Findings • Culture and Sensitivity • • • • • • Haemophilus influenzae Streptococcus pneumoniae Staphylococcus aureus Pseudomonas aeruginosa Anaerobic organisms Sputum separates into layers • CBC • Polycythemia and increased WBC (infection). Diagnosis • Bronchography (Bronchogram) • Injection of opaque contrast material into the TB tree • Rarely done. • High-Resolution CT Scan • Bronchial walls appear thick, dilated. • Replaced standard CT scan and Bronchography as gold standard. Prophylaxis • Awareness and early identification may allow for earlier intervention. • Childhood immunizations. • Reduce exacerbations. Treatment Goals • • • • Reduce infections/exacerbations Manage secretions Reduce airway obstruction Treat complications • • • • Hemoptysis Hypoxemia Respiratory Failure Cor Pulmonale Treatment • • • • Antibiotics to treat pneumonia Inhaled steroids to reduce inflammation Oxygen therapy (low FiO2) Bronchial Hygiene Protocol • • • • CPT/PD Hydration Deep breathing/coughing Humidification Therapy • Aerosol Therapy • Mucolytics • Bronchodilators • • • • Flu shots/Pneumonia Vaccinations Bronchoscopy Avoidance of respiratory irritants Surgical resection • Saccular is most suitable for surgery Prognosis • Mild Bronchiectasis – may have a normal life span • Extensive Bronchiectasis – shorter life span • Result of respiratory infection and complications • Disease of slow deterioration interspersed by episodes of exacerbation