OMM BOARD REVIEW
advertisement

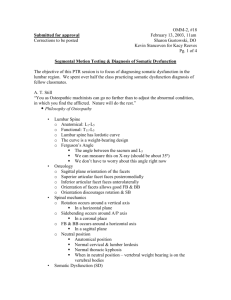
OMM BOARD REVIEW THE BASICS THE OSTEOPATHIC PRINCIPLES The body is a unit. Structure and function are reciprocally related. The body possesses self-regulatory mechanisms The body has the inherent capacity to defend itself and repair itself. When normal adaptability is disrupted, or when environmental changes overcome the body’s capacity for self maintenance, disease may ensue. THE OSTEOPATHIC PRINCIPLES Rational treatment is based on the previous principles Movement of the body fluids is essential to the maintenance of health. The nervous system plays a crucial part in controlling the body. There are somatic components to disease that are not only manifestations of disease but also are factors that contribute to maintenance of the diseased state. SOMATIC DYSFUNCTION An impairment or altered function of related components of the somatic (body framework) system: Skeletal, Arthroidial, and Myofascial structures and related vascular, lymphatic, and neural elements. Somatic Dysfunction is a Restriction in joints muscles, or fascia that may affects blood supply, lymph flow, and nervous function. SOMATIC DYSFUNCTION Diagnostic Criteria: Tenderness Asymmetry Restriction Tissue Texture Changes SOMATIC DYSFUNCTION Tenderness May be produced during palpation of tissues where it should not occur if there was no somatic dysfunction. SOMATIC DYSFUNCTION Asymmetry Bones, muscles, or joints may feel asymmetric to corresponding structures. SOMATIC DYSFUNCTION Restriction In somatic dysfunction, a joint will have a restrictive (pathologic) barrier. A restrictive barrier lies before the physiologic barrier. Barriers to Motion Physiologic Barrier: A point at which a pt can actively move a given joint. Anatomic Barrier: A point at a physician can passively move a given joint. Motion beyond the anatomical barrier will cause skeletal injury. Acute VS Chronic Somatic Dysfunction Findings Acute Chronic Tenderness Severe, Sharp Dull, Achy, Burning Asymmetry Present Present with compensation in other areas Restriction Present, painful ROM Present, dec. or no pain w/ROM Tissue Texture Changes Edema, erythema, boggy, Inc. tone, Inc. moisture Decreased or no edema or erythema. Cool dry skin, flaccid tone, fibrotic Fryette’s Principle’s Principle I If the spine is in neutral position (no flexion or extension) and if sidebending is introduced, rotation would then occur to the opposite side. Principle I In the Neutral position: Sidebending precedes rotation. Sidebeding and rotation occur in opposite directions. e.g.: NSLRR Typical of a group dysfunction Principle II If the spine is in a non neutral position (flexed or extended) and rotation is introduced, sidebending would then occur to the same side. Type II Somatic Dysfunction In a non neutral position: Rotation precedes sidebending, sidebending and rotation occur to the same side. e.g.: FRRSR Principle II is typical of a single vertebral dysfunction Principles I and II do not apply to cervical vertebral motion. Principle III Initiating motion of any vertebral segment in any one plane of motion will influence the mobility of that segment in the other two planes of motion. Eg: Forward bending will decrease the ability to sidebend and rotate. Naming Somatic Dysfunction Somatic Dysfunctions are always named for their FREEDOM OF MOTION. When referring to segmental motion, it is traditional to refer to motion of the segment above in a functional vertebral unit. e.g.: If L2 is restricted in the motions of flexion, sidebending to the right and rotation to the right, then L2 is said to be extended, rotated and sidebent to the left on L3……L2 is ERLSL. Evaluating Somatic Dysfunction Thoracic and Lumbar Spine Assess rotation by placing the thumbs over the transverse processes of each segment (posterior thumb). Then check the rotation of the segment. – Flexion – Extension – Neutral Somatic dysfunction is named for freedom of motion Evaluating Somatic Dysfunction Motion Testing of the Cervical Spine Translation– Best for evaluation of the OA. Right translation will induce left sidebending. Rotation– Best for evaluation of the AA. Remember to flex the neck 45* to lock out C2-C7. C2-C7—Typically evaluated with translatory force directed at the articular pillars Facet Orientation REGION Facet Orientation Cervical Backward, upward, medial (C2-C7) Thoracic Backward, upward, lateral Lumbar Backward, medial Main Motion OA-flexion/extension AA-rotation C2-C7—rotation/SB Rotation Flexion/Extension Physiologic Motion Motion Axis Plane FLx’n/Ext’n Transverse Sagittal Rotation Vertical Transverse Sidebending A/P Coronal Osteopathic Treatment GOAL: To eliminate restrictive barriers and restore equilibrium and symmetry within the body. Treatment techniques are aimed at improving quality and range of impaired movements, softening fibrotic areas, relieving muscle spasm, and mobilization of joints. Direct VS Indirect Direct Treatment: the practitioner engages the restrictive barrier eg; T3 FRRSR: TX: extension, left rotation and sidebending. Indirect Treatment: the practitioner moves tissues and joints away from the restrictive barrier. eg; T3 FRRSR : TX: flexion right rotation and sidebending Active VS Passive Active Treatment: the pt will assist in the treatment, usually in the form of isometric or isotonic contraction Passive Treatment: the pt relaxes and allows the practitioner to to move the body tissues. Myofascial Release Can be either direct or indirect, passive or active Palpate restriction Apply compression (indirect) or traction (direct) Add twisting or transverse forces Use enhancers---respiration, eye movement, muscle contraction. Await release Indications: acutely ill, elderly who cannot tolerate much movement. CHF, Asthma, COPD Contraindications: Cancer, Sepsis, osseous fracture, traumatic disruption of viscera. E.g. Diaphragm Release Counterstrain Passive, indirect technique. Extremely gentle technique where “tenderpoints” are treated at a point of balance, or ease. Positioning is aimed at shortening the muscles around the tenderpoint and held for 90 seconds.* Body part is then returned to resting position, passively. Treat the most tender area first. Know specific tenderpoints! Facilitated Positional Release Passive, indirect technique The component region of the body is placed into a neutral position, diminishing tissue and joint tension in all planes. A facilitating force, either compression or torsion, is then added to place a joint or muscle into it’s ease of motion. Used to treat superficial muscles, and deep intervertebral muscles to influence spinal motion. Muscle Energy An Active, direct technique.** Involved joint’s restrictive barrier is engaged. The pt is directed to gently push in the direction of freedom for about 3-5 sec and then relax the contracted muscle(s) Physician engages new barrier. Process is repeated for a total of 3 times. Don’t forget the passive stretch. ** postisometric relaxation High Velocity Low Amplitude A passive and direct technique The force is applied very quickly and the distance moved is very small. The physician directs a quick controlled force through the joint to move it. Absolute Contraindications: Sever RA Osteoporosis Fractures Osteomyelitis Bone metastases Most common overall complication: Vertebral artery injury. Methods of Treatment Treatment Direct or Indirect Active or Passive Myofascial Release Both Both Counterstrain Indirect Passive FPR Indirect Passive Muscle Energy Direct (rarely indirect) Active HVLA Direct Passive Choice of Treatment Elderly pts and hospitalized patients typically respond better with indirect techniques. The use of HVLA in a pt with advanced osteoporosis my lead to pathologic fractures. Acute neck strain/sprains are often treated with indirect techniques to prevent further strain. Pts with advanced stages of cancer should not be treated with lymphatic techniques due to increased risk of lymphogenous spread Dose and Frequency The sicker the pt, the less the dose. Allow time for the patient to respond to treatment Chronic disease requires chronic treatment Pediatric pts can be treated more frequently; geriatric pts need longer interval to respond to treatment. Acute cases should have a shorter interval between treatments; as they respond, the interval is increased. Sequence of Treatment For low back pain with psoas involvement, treat the lumbar spine first. Treat the upper thoracic spine and ribs before treating the cervical spine. Treat the T-spine before treating specific rib dysfunctions. For very acute SD, treat secondary areas to allow access to the acute area. For extremity problems, treat the axial skeleton components first (spine, sacrum, ribs). Question 1 Which one of the following is not a diagnostic characteristic of somatic dysfunction? A. Edema B. Temperature change C. Tenderness D. Full range of motion E. Asymmetry Question 1 Which one of the following is not a diagnostic characteristic of somatic dysfunction? A. Edema B. Temperature change C. Tenderness D. Full range of motion E. Asymmetry Question 2 While evaluating a pts upper back you notice T2 is rotated right. Flexing causes T2 to further rotate right. Extending the pts back cause T2 to return to neutral position. Which best describes this dysfunction? A. ERRSR B. FRRSR C. ERRSL D. FRRSL Question 2 While evaluating a pts upper back you notice T2 is rotated right. Flexing causes T2 to further rotate right. Extending the pts head cause T2 to return to neutral position. Which best describes this dysfunction. A. ERRSR B. FRRSR C. ERRSL D. FRRSL Question 3 Which cervical segment is best evaluated by flexing the neck 45* and rotating the head? A. B. C. D. E. OA C1 C2 C3 C4 Question 3 Which cervical segment is best evaluated by flexing the neck 45* and rotating the head? A. B. C. D. E. OA C1 C2 C3 C4