Pediatric Infectious Disease
advertisement
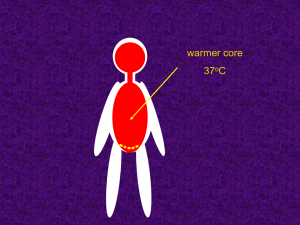
Pediatric Infectious Disease Brenda Beckett, PA-C Immunizations Reduced childhood infectious disease markedly US: 14 diseases – Diphtheria, tetanus, pertussis, measles, mumps, rubella, poliomyelitis, Hib, S. pneumoniae, HBV, HAV, influenza, varicella, rotavirus Vaccine preventable diseases Viral exanthems (covered in derm) Hepatitis (covered in ID) Polio Other dermatology Impetigo Tinea Molluscum Cellulitis Fever Normal body temp: 37 C, 98.6 F Range of 97-99.6 Rectal temp >100.4F (38 C) is FEVER Diurnal variation Age variation Fever, Newborns Neonates do not have febrile response <3 months old, any fever is risk of serious bacterial infection May not have localizing signs Warrants workup: bacteremia, UTI, meningitis, pneumonia, etc Fever, <3 years Exaggerated febrile response: up to 105 No localizing sx: risk of S. pneumo, N. meningititis, Hib, Salmonella Observe child for alertness, irritability, consolability FUO Fever of unknown origin T >100.4 F lasting >14d with no obvious cause List, p 463 Nelson Febrile Seizure Usually <3 yo Seizure can be first sign of fever Rule out other causes Increased risk of repeat seizures with fever Treat with antipyretics Conjunctivitis progressive redness of conjunctiva discharge – bacterial = profuse,purulent – viral = minimal, mucoid unilateral ---> bilateral preauricular node enlargement – viral Treat: bacterial – topical antibiotics Ophthalmia Neonatorum Conjunctivitis in the newborn – occurs during first 10 days of life – Acquired at brith red, swollen lids & conjunctiva, discharge. – Can lead to blindness Erythromycin at birth Cause : includes – Chlamydia trachomatis – N. gonorrhoeae Nasolacrimal Duct Obstruction Cause - obstruction in any part of drainage system wet eye with mucoid discharge – skin irritation – Increased risk of bacterial conjunctivitis most clear spontaneously – massage – Antibiotics for bacterial surgical treatment - probing Periorbital Cellulitis Infection of the structures around the eye Cause : – S. aureus or S. pyogenes Lid edema, pain, mild fever Arises from local, exogenous source Treatment – systemic antibiotics Orbital Cellulitis Usually from bacterial sinus infection Signs of periorbital cellulitis, plus: – proptosis – restricted and painful eye movement – high fever CT or MRI Treatment – drainage, systemic antibiotics Otitis Externa Cause : Pseudomonas or S. aureus minor itching ---> intense pain tenderness tragus/auricle erythema/swelling of canal purulent discharge possible postauricular node involvement Treatment: Otic antibiotics, drying Otitis Media S. pneumo, H. influenza, M. catarrhalis Many resistant to penicillin Major reason for pediatrics visit Risks: young age, bottle feeding, fam hx, smoke exposure, viral URI Otitis Media Recurrent: >6 episodes in 6 mo Treat: Typmanostomy tubes Sx: Fever, irritability, poor feeding, otalgia. Otorrhea (rupture) Exam: Effusion, erythema, decreased mobility Otitis Media Treat: based on age and severity – < 6mo – 6mo-2yr – >2yr Antibiotics ABX for certain, observation or ABX for uncertain Observation or ABX for severe Acute Viral Rhinitis Under age 5 --> 6-12 colds per year Symptoms : – clear to mucoid rhinorrhea/nasal congestion – *fever – mild sore throat/cough Management : – saline drops/bulb suction Sinusitis Symptoms : – URI lasting longer than 10-12 days – low-grade fever, cough, HA in older child – malodorous breath – intermittent AM periorbital swelling/redness Trt: amox, augmentin, azythromycin Thrush Cause : Candida albicans mainly affects infants – refusal of feedings (?soreness of mouth) lesions are white plaques on buccal mucosa – cannot be washed away – bleed if scraped treatment - nystatin oral suspension Lymphadenopathy Most prominent in 4-8 yo Cervical most common Location can differentiate cause of infection Patient Presentation 5 year old with sore throat x48 hrs Temp 101 at home last night Other history questions? PE: erythematous pharynx, white exudate. Enlarged ant. Cervical nodes DD??? Pharyngitis/Tonsillitis School-age 5-15 years Symptoms : – sorethroat – fever/chills – general malaise – referred ear pain – headache – abdominal pain/vomiting Pharyngitis/Tonsillitis Signs : – red, inflamed posterior pharyngeal wall – swollen, erythematous tonsils – petechiae and beefy red uvula – tender cervical adenopathy Causes: Group A strep, rhinovirus, EBV, etc Pharyngitis/Tonsillitis Scarlet fever: strawberry tongue Peritonsillar abscess: “hot potato voice” Strep pharyngitis: Always treat with abx, definitively diagnose strep EBV: blood test - “monospot”, EBV titers Viral pharyngitis: URI sx Mononucleosis Symptoms : – – – – – prodromal phase fever sorethroat *tender lymph nodes abdominal pain Signs : – exudative pharyngitis/tonsillitis – **lymphatic enlargement posterior cervical, axillary, inguinal – splenomegaly, less often hepatomegaly Mononucleosis Lab: Positive monospot or EBV titer Treat: usually supportive unless lymphadenopathy is severe, then oral steroids Patient Presentation 18 month old with “wheezing” URI sx for 2-3 days No fever Other history questions? DD?? Larnygotracheobronchitis (Croup) Cause : parainfluenza virus type 1 peak age 6 months to 2 years Symptoms : – URI (prodrome) – harsh, barking (seal-like) cough – hoarseness – inspiratory stridor – fever (absent or low-grade) Treatment for Croup Self-limiting – mist – hydration Dexamethasone Injection – 0.3-0.6mg/kg, repeated in 12 hours Racemic epinephrine – via nebulizer – rebound effect in 2 hours Epiglottitis *true medical emergency cause : Haemophilus influenza type B sudden onset of fever dysphagia / drooling / muffled voice inspiratory retractions / soft stridor **sitting position *cherry-red, swollen epiglotittis **Endotracheal intubation Bronchiolitis RSV = respiratory syncytial virus winter and early spring peak age 2-10 months fever URI ---> wheezing and tachypnea – nasal flaring, retractions, crackles/wheezing labs : CXR, nasal swab/washing Treatment Usually self-limiting, supportive – 3-7 days Hospitalization, O2 – younger than 6 months of age – respiratory distress, hypoxemia – underlying disease Ribavirin (antiviral therapy) Immunoglobulin anti RSV (Synagis) Pertussis (Whooping cough) Cause : Bordetella pertussis most common and most severe under 1 year adults frequently source of infection Three stages of disease – catarrhal stage – paroxysmal stage – convalescent stage Pertussis Labs : – WBC = 20-30K, 70-80% lymphs – nasopharyngeal swab for PCR, culture Treatment : – erythromycin 40-50mg/kg/24hours x 14 d – nutritional support – steroids/albuterol Pneumonia S. pneumo and HiB – immunizations Viral (RSV) Sputum? Mycoplasma Pneumonia Most common cause of pneumonia in school-age children peaks in fall slow onset of symptoms – scratchy throat – low-grade fever – headache – dry, non-productive cough Mycoplasma Pneumonia Signs : – widespread crackles – decreased breath sounds CXR - patchy infiltrates Labs : – WBC = normal – cold agglutinin titer = 1:32 or greater Treatment – erythromycin, azythromycin Chlamydial Pneumonia Acquired from infected mother at delivery Age : 2-12 weeks Symptoms/Signs : – – – – – *conjunctivitis rhinitis and cough (resembles pertussis) / OM scattered inspiratory crackles / tachypnea **wheezes rarely present no fever Chlamydial Pneumonia Labs : – serum immunoglobins usually high – nasopharyngeal swab – peripheral eosinophilia > 400 cells/mm3 CXR : – diffuse infiltrates and hyperexpansion Treatment : – Erythromycin, azythromycin Meningitis Causative organisms change with age Preceding URI sx HA, irritability, nausea, nuchal rigidity, lethargy, photophobia, vomiting Fever Kernig and Brudzinski signs LP Patient Presentation 7 month old with 24 hrs of vomiting, diarrhea No fever Other history questions? DD?? Acute Viral Gastroenteritis Rotavirus - cause of 80% of infections in infants and young children (4-24 months) winter months vomiting, followed by profuse, watery diarrhea and low-grade fever abdominal pain, nausea, cramping History duration, frequency, description of stool duration, frequency of vomiting amount and type of fluids and solids ingested frequency of urination exposure to others with V/D Signs of Dehydration body weight mucous membranes skin turgor / color fontanelles pulse/BP/respirations/perfusion tears urinary output Treatment Infants : – continue breast feeding – oral rehydration solution-->1/2 strength formula-->full strength formula Older child : – sips of clear fluids – ORT **New vaccine Pinworms Most common parasitic disease in children cause : Enterobius vermicularis symptom : perianal itching, esp. nocturnal labs : adhesive tape test treatment : mebendazole 100 mg CH Urinary Tract Infection Infants : – strong-smelling urine – Irritability – Or just fever Preschooler : – – – – abdominal pain vomiting strong-smelling urine fever UTI School-age : ‘classic’ – Dysuria, frequency, urgency, secondary enuresis, foul-smelling urine, fever, flank pain Treat: Neonates 10-14 days Older children 7-14 days Recurrent UTI’s Renal ultrasound VCUG – vesicoureteral reflux Causes : – infrequent or incomplete voiding – poor perineal hygiene – pinworms – bubble baths Antibiotic Dosing in Children Dose based on weight Taste Dosing schedule